22-40% of all COPD patients experience at least one moderate or severe exacerbation annually. Patients with frequent exacerbations have a worse prognosis. A team of researchers has been looking at how biomarkers can be used to better diagnose, target and prevent COPD exacerbations in the future.
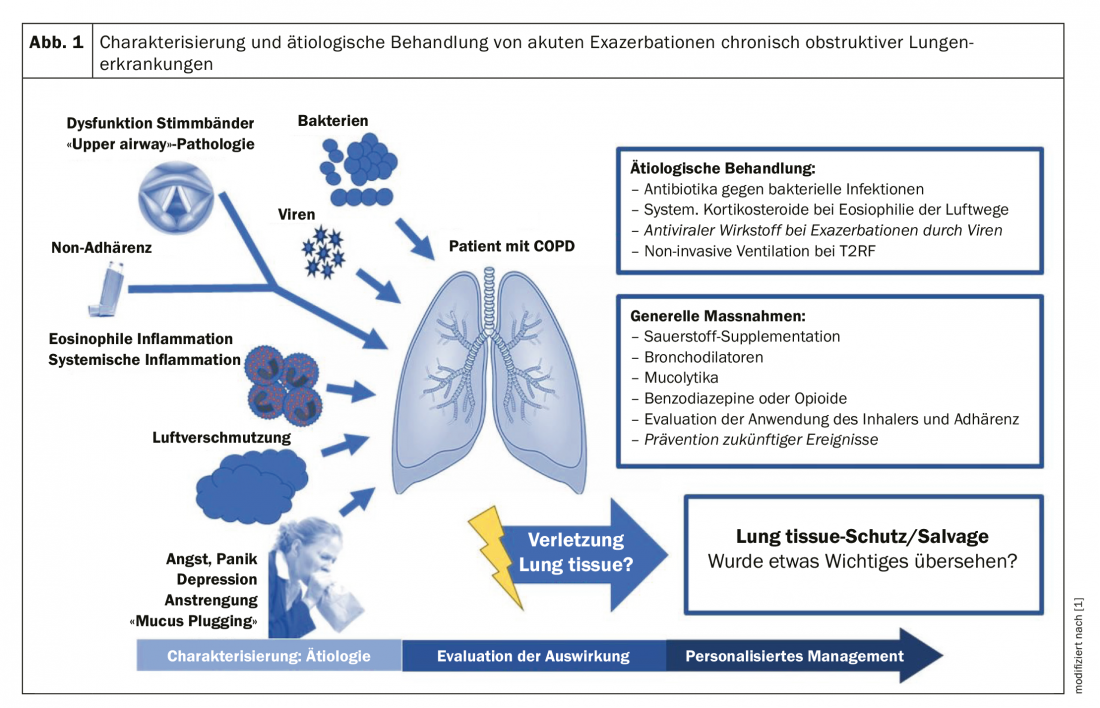
Therapeutically, exacerbations are uniformly treated with bronchodilators, systemic corticosteroids, and usually antibiotics. In fact, however, they are heterogeneous and characterized by different underlying mechanisms, outcomes, and treatment needs. Thus, only between 30% and 50% of all exacerbations are associated with increased eosinophilic airway inflammation and appear to respond to systemic corticosteroids, whereas approximately 50% are caused by bacterial infections and may respond to antibiotics.
In the context of COPD exacerbations, biomarkers may be used in a variety of settings. They can be used as a diagnostic tool for early detection of events, as a staging tool to classify disease severity and/or identify important subgroups, as a prognostic tool to predict clinically important outcomes, and probably most importantly as a therapeutic tool to identify treatment indications and monitor response. Ideally, a biomarker for COPD exacerbations is mechanistically linked to the acute onset of airway inflammation, which it detects with both high negative and high positive predictive value.
In acute myocardial infarction, cardiac troponin T covers most of these requirements. The challenge in COPD exacerbations has long been to find an equally meaningful biomarker. However, because of the heterogeneity of exacerbations, it seems to be generally accepted that such a “global” marker most likely does not exist, write scientists led by Alexander G. Mathioudakis, M.D., of the Division of Infection, Immunity and Respiratory Medicine at the University of Manchester in the United Kingdom. Nevertheless, there are several promising approaches to improve the treatment of COPD using biomarkers.
Blood and sputum markers with potential
In 6574 patients with COPD identified in general population studies in Copenhagen, concomitant elevated CRP, fibrinogen, and total white blood cell levels were associated with a higher risk of exacerbations, particularly in the clinical subgroup of patients at risk because of a history of exacerbations or poor FEV1. In addition, a study analysis identified an accurate imaging biomarker. A pulmonary artery to aortic diameter ratio greater than one, indicative of pulmonary hypertension, was independently associated with a threefold increase in the risk of exacerbations. Physiologic markers such as increased respiratory impedance also predicted future exacerbations.
Another study examined the association of exacerbations with lung tissue injury and found altered levels of several airway extracellular matrix turnover biomarkers with diagnostic potential in two independent patient cohorts. These biomarkers may be able to identify events associated with future risk of poor outcomes. Such patterns of lung tissue injury biomarkers could revolutionize the management of exacerbations in the same way that troponin revolutionizes the management of acute cardiac symptoms by distinguishing myocardial infarctions from simple episodes of angina, the authors write. Unfortunately, Dr. Mathioudakis and colleagues noted, the European COPD audit was unable to evaluate the added value of blood or sputum biomarkers for prognosis.
One potential way to better determine biomarkers in COPD exacerbations may be to better identify and characterize the subtypes of exacerbations. Accordingly, classifying exacerbations according to their causative agents, such as bacterial infections, viral infections, or amplified airway inflammation, seems to be most promising (Fig. 1).
Bacteria and COPD exacerbations
Bacteria are frequently identified in sputum cultures in over 50% of exacerbations, especially during the winter months. However, high detection rates (>25%) also occur in stable disease. Therefore, identification of bacteria during an exacerbation may establish No bacterial etiology. In the absence of experimental studies, it remains unconfirmed whether bacteria can directly trigger exacerbations.
Alterations in the lung microbiota have also been considered as possible causes of exacerbations. Modern molecular sequencing techniques have shown that healthy airways are colonized by microbiota. The microbiota in COPD is largely characterized by an outgrowth of Proteobacteria phylum and an increase in the proportion of Streptococci and Staphylococci in the Firmicutes phylum.
Our knowledge of the dynamic shifts that occur within the lung microbiota during exacerbations is limited, but recent studies have shed some light on this topic. One study showed that microbial dysbiosis was present in 41% of exacerbations and was associated with acute FEV1 decline and elevated COPD assessment test (CAT). Further studies are needed to understand if and how shifts occur, the authors express confidence.
Although the role of bacterial infection as a trigger for COPD exacerbations has not been confirmed, antibiotic use remains prevalent, with >80% in secondary care and about 50% in primary care. The Global Initiative for Chronic Obstructive Lung Disease (GOLD) give the use of antibiotics for COPD exacerbations a category B evidence rating.
Respiratory viruses and COPD exacerbations.
Respiratory viruses are identified in 30-50% of all COPD exacerbations. However, it is also found in >10% of patients during a stable disease state at any given time. The most commonly detected viruses in COPD include rhinovirus, influenza, and respiratory syncytial virus (RSV). In contrast to the uncertainty about how bacteria trigger exacerbations, experimental studies of viral load have confirmed a direct causal relationship between viral infections and COPD exacerbations.
Because viral-triggered COPD exacerbations are characterized by prolonged and distressing symptoms, antiviral vaccines and treatments may be beneficial. Several RCTs and large real-world studies have shown that influenza vaccination is highly effective in reducing the incidence of COPD exacerbations. In practice, however, influenza is underdiagnosed during exacerbations.
An accurate biomarker that can confirm the viral etiology of exacerbations is still lacking. Symptoms of an upper respiratory infection or cold may coincide with or precede viral-associated exacerbations. However, the diagnostic accuracy of this approach is limited.
Exacerbations due to eosinophilic airway inflammation
Airway inflammation in COPD includes the presence of various inflammatory cells such as neutrophils, CD8 + T lymphocytes, mast cells, eosinophils, and macrophages. Until recently, COPD was considered to be a primarily neutrophil-mediated inflammatory disease. However, 20% to 40% of patients with COPD have been found to have eosinophilic airway inflammation, both during a stable phase and during exacerbations, even after patients with concurrent asthma have been excluded. Interestingly, these patients respond better to corticosteroid therapy. Blood eosinophil count correlates relatively well with sputum and airway eosinophil levels and could be used as a surrogate measure of airway eosinophilia in COPD.
In stable COPD, higher blood eosinophil counts are associated with increased risk of future exacerbations, especially eosinophilic exacerbations. It is also a predictor of treatment response (reduction in exacerbation) to ICS.
COPD exacerbations characterized by increased eosinophilic airway inflammation are generally milder, being associated with lower mortality and shorter length of hospital stay. Bacterial infections are rarely present, whereas the presence of viral infection in eosinophilic exacerbations remains controversial. A higher blood eosinophil count during exacerbations is indicative of clinical response to oral corticosteroids.
Better characterization of the eosinophilic COPD phenotype may allow the introduction of more targeted therapeutic strategies. This could limit the use of corticosteroids in a patient population with low eosinophil counts.
Precision medicine for the prevention of exacerbations
Prevention of exacerbations is a critical therapeutic goal in stable COPD. Most available treatments address this to some extent, as shown by randomized controlled trials in patients with COPD and frequent exacerbations.
In one study, the addition of an ICS (fluticasone furoate) consistently reduced the frequency of exacerbations treated with systemic corticosteroids alone or with both antibiotics and systemic corticosteroids (treatment was decided by the responsible physician). On the other hand, fluticasone resulted in a 12% increase in the frequency of exacerbations treated with antibiotics alone compared with placebo.
The results from a comparison of indacaterol glycopyrronium vs. Fluticasone Salmeterol on COPD exacerbations showed that the combination of a long-acting beta agonist (indacaterol) with a long-acting antimuscarinic (glycopyrronium) significantly reduced the rate of moderate or severe exacerbations treated with antibiotics or with antibiotics and systemic corticosteroids compared with the combination of a long-acting beta agonist (salmeterol) with an ICS (fluticasone propionate).
Such observations suggest that long-acting bronchodilators are effective in preventing all subtypes of exacerbations, lead Mathioudakis et al. off. On the other hand, ICS may be more effective in people with frequent eosinophilic exacerbations but should be avoided in patients with recurrent bacterial exacerbations. Further research is needed to validate these findings and evaluate the role of different medications in the defined patient groups of exacerbations.
The future of COPD management
The assessment, management, and prevention of exacerbations are likely to change significantly in the future, the authors summarize their research. Heterogeneity in mechanisms and outcomes of COPD exacerbations can be addressed by etiologic grouping. Therefore, the greatest challenge is to develop and validate accurate biomarkers for early characterization of the different types of exacerbations, beyond the bacterial, viral, and eosinophilic forms presented. Such biomarkers could facilitate optimization of exacerbation management and development of novel targeted treatments. Because most exacerbations are treated in primary care, the biomarkers selected must be rapid, close to the patient, and easy to measure to facilitate implementation in primary care. This probably improves clinical outcomes of exacerbations, but also COPD in general, he said.
Literature:
- Mathioudakis AG, Janssens W, Sivapalan P, et al: BMJ; online first: 26 March 2020; doi: 10.1136/thoraxjnl-2019-214484
InFo PNEUMOLOGY & ALLERGOLOGY 2020; 2(2): 28-31.