According to a secondary analysis published in 2019, low vitamin D levels are associated with worse disease progression and impaired quality of life. Regarding possible beneficial effects of vitamin D supplementation in this patient population, further research is needed.
As data from a Systematic Review published in 2019 [1] show, low 25-OH-D levels are a biomarker of disease activity in inflammatory bowel disease (IBD) and a predictor of worse outcome. The concentration of 25-OH-D reflects the intake of vitamin D with food and its formation from the provitamins in the skin by UV light. A distinction is made between normal vitamin D status (serum 25-OH vitamin D level >75 nmol/l), vitamin D insufficiency (<75 nmol/l), and actual vitamin D deficiency (serum 25-OH vitamin D level <15 nmol/l).
Multifactorial etiology and relapsing-remitting course
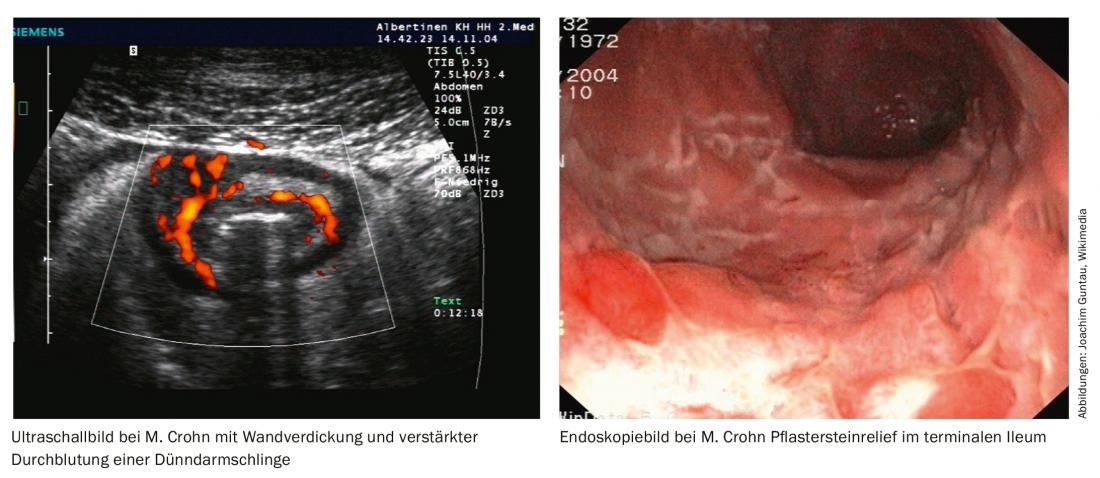
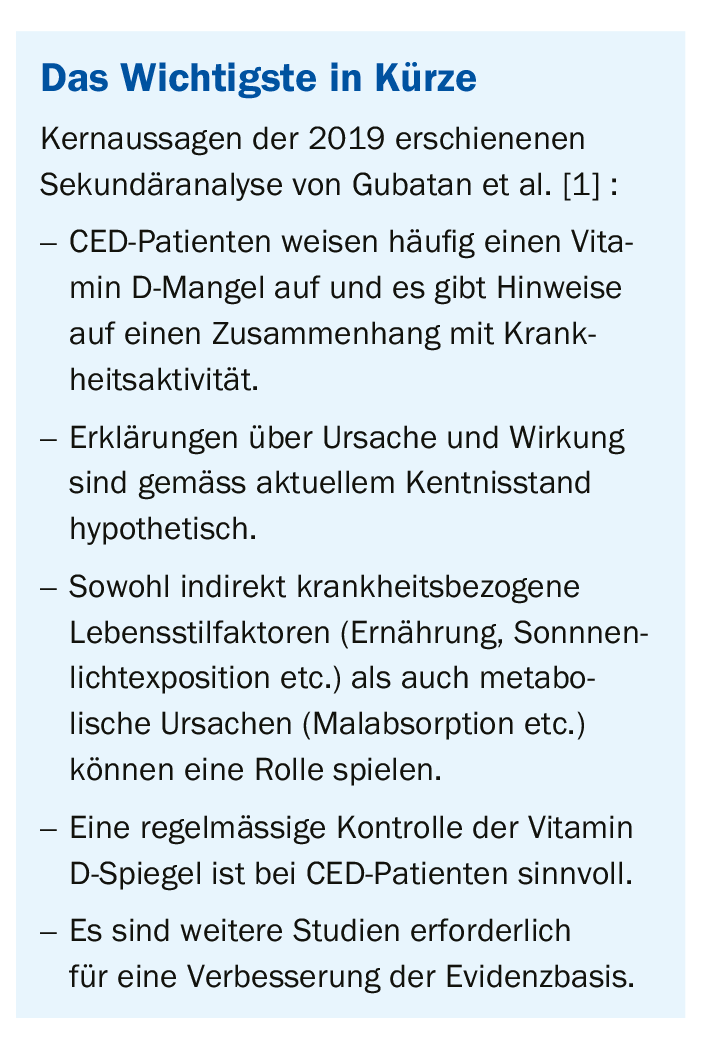
Ulcerative colitis and Crohn’s disease, the two major types of IBD, are characterized by alternating periods of low disease activity with severe exacerbations. Lifelong treatment is often required for symptom control and improvement of quality of life. The therapeutic goal is primarily relief and a reduction in the occurrence of relapses. Symptoms vary interindividually and range from mild abdominal pain to colicky symptoms and numerous bouts of diarrhea. Chronic inflammation in the intestine is due to a dysregulation of the immune system.
Regarding the etiology of IBD, there are still many unanswered questions. Current knowledge suggests multifactorial causes, involving complex interactions between genetic predisposition, immune and gut microflora dysregulation, and environmental trigger factors [1]. There is a growing body of evidence supporting that vitamin D may play a protective role in the pathogenesis of IBD [2,3]. For example, vitamin D has been shown to play an important role in maintaining epithelial barrier function in the intestinal tract to defend against inflammatory and pathogenic factors [4,5]. In addition, previous studies have demonstrated anti-inflammatory functions and regulatory effects on the gut microbiome in the context of immune responses [6,7].
High prevalence of deficiency symptoms
Too low vitamin D levels are common in patients with IBD. According to a secondary analysis with data from more than 900 patients [8], deficiency was present in 38.1% of people with Crohn’s disease and in 31.6% of people with ulcerative colitis (criterion: serum level 25(OH)D ≤25 ng/mL). A possible association between vitamin D and IBD has been discussed for some time, but previous studies did not reach clear results [1]. This may be due to methodological aspects (e.g., small subject sample, heterogeneous disease stages, small effect sizes, different cutoff values for determining vitamin D deficiency). Thus, there are still knowledge gaps in understanding the role of vitamin D in the pathogenesis of IBD.
Complex interaction structure
The study by Gubatan et al. In 2019, the goal was to learn more about how low vitamin D levels, which are common in IBD patients, are related to disease-relevant parameters (disease activity, mucosal inflammation, relapse rate, quality of life). A total of 27 publications from 2011 to 2018 were included (ulcerative colitis: n=3115; Crohn’s disease: n=5201) [1]. Data are from patients from 6 continents and 14 countries (Australia, Brazil, Canada, China, Denmark, Germany, Iran, Ireland, Netherlands, Norway, Portugal, Slovakia, South Africa, USA). The mean age was 41.4 years, and the gender distribution was 45.7%:54,3% (males:females). The mean 25(OH)D concentration of all CED patients was 25.5 ng/mL. The quality of the included studies was assessed using the Newcastle-Ottawa scale (mean = 7, range = 4-9). 17 studies (n = 3143) met the “clinically active disease” criterion. The evaluation showed that low 25(OH)D levels were associated with disease activity, both related to all IBD patients (pooled OR 1.53; 95% CI 1.32-1.77; p<0.00001) as well as in the subgroups ulcerative colitis (pooled OR 1.47; 95% CI 1.03-2.09; p=0.03) and Crohn’s disease (pooled OR 1.66; 95% CI 1.36-2.02; p<0,00001). There was no significant difference between the two subgroups (p=0.43).
Because the meta-analysis included observational studies, direct causality cannot be inferred. Evidence suggests that low baseline vitamin D levels are associated with increased risk of future disease activity and recurrence. It is possible that vitamin D plays a role as both a cause and an effect with respect to clinical course parameters of IBD.
Supplementation useful?
Possible explanations for low vitamin D levels in IBD patients include nutritional factors and malabsorption associated with inflammatory processes. On the other hand, malaise as a consequence of an acute episode may lead to less time spent outdoors with correspondingly reduced sunlight exposure and thus lower endogenous vitamin D production.
In a meta-analysis published in 2018 by Li et al. [9] demonstrated that vitamin D supplementation resulted in an increase in baseline 25(OH)D levels and was associated with a decreased risk of CED relapse compared with placebo. However, the relationship between relapse rates and the supplemented vitamin D dose could not be clearly elucidated. Vitamin supplementation had no effect on the inflammatory markers ESR and CRP.
According to Gubatan et al. [1], it can be deduced from the results of various secondary analyses that routine monitoring of vitamin D levels should be performed in patients with IBD. Further studies are needed to conclusively answer the question of whether supplementation for vitamin D deficiency is a potential therapeutic target, he said.
Literature:
- Gubatan J, Chou ND, Haagen Nielsen O, Moss AC: Systematic review with meta-analysis: association of vitamin D status with clinical outcomes in adult patients with inflammatory bowel disease. Alimentary Pharmacology and Therapeutics 2019, https://doi.org/10.1111/apt.15506
- Gubatan J, Moss AC: Vitamin D in inflammatory bowel disease: more than just a supplement. Curr Opin Gastroenterol 2018; 34: 217-225.
- Nielsen OH, Rejnmark L, Moss AC: Role of vitamin D in the natural history of inflammatory bowel disease. J Crohns Colitis 2018; 12: 742-752.
- Assa A, et al: Vitamin D deficiency predisposes to adherent-invasive Escherichia coli-induced barrier dysfunction and experimental colonic injury. Inflamm Bowel Dis 2015; 21: 297-306.
- Chen SW, et al: Protective effect of 1, 25-dihydroxyvitamin d3 on lipopolysaccharide-induced intestinal epithelial tight junction injury in caco-2 cell monolayers. Inflammation 2015; 38: 375-383.
- Gubatan J, et al: Higher serum vitamin D levels are associated with protective serum cytokine profiles in patients with ulcerative colitis. Cytokine 2018; 103: 38-45.
- Tabatabaeizadeh SA, et al: Vitamin D, the gut microbiome and inflammatory bowel disease. J Res Med Sci 2018; 23: 75.
- Del Pinto R, et al: Association between inflammatory bowel disease and vitamin D deficiency: a systematic review and meta-analysis. Inflamm Bowel Dis 2015; 21: 2708-2717.
- Li J, Chen N, Wang D, et al: Efficacy of vitamin D in treatment of inflammatory bowel disease. Medicine 2018; 97: e1266.
HAUSARZT PRAXIS 2019; 14(11): 22-24