Assuming that beauty goes hand in hand with harmonious proportions, it is understandable that breast augmentation is a strong trend among women. Implants filled with silicone or saline are the most common method here. But more and more often women are afraid of clearly visible or palpable implants and ask for a “natural” alternative. Lipofilling per se as well as specifically of the female breast has been among the top 5 aesthetic surgical procedures worldwide for many years and has long since established itself among cosmetic surgeries.
The desire to feel good in your body is probably one of the basic needs of every human being. But why is it important for us to conform to the “common ideal of beauty”? We know from developmental psychology studies that even babies smile more often at “beautiful people.” In our society today, we equate beautiful people with attributes such as: Health, attractiveness, higher efficiency, safe survival and higher reproduction. We trust them to have better jobs, more wealth and a better standard of living.
But what is fundamentally beautiful? The ideal of beauty varies from country to country and has changed massively over the last millennia. A mathematical calculation gives us “the golden ratio” of Leonardo Da Vinci, who calculated the universal standard of beauty with the proportion 1:1.618. Assuming that beauty goes hand in hand with harmonious proportions, it is understandable that breast augmentation is a strong trend among women. Implants filled with silicone or saline are the most common method of permanently changing proportions. But more and more often women are afraid of clearly visible or palpable implants and ask for a “natural” alternative. The desire to make one’s own breasts appear larger and plumper again by half a cup to one cup per procedure can be fulfilled simply and easily: permanent breast augmentation with autologous fat!
Lipofilling per se, as well as specifically of the female breast, has been among the top 5 aesthetic surgical procedures worldwide for many years and has long since established itself among cosmetic surgeries.
History
The history of lipofilling began in 1893 with the German surgeon Dr. Gustav Neuber. 2 years later, it was Dr. Vincenz Czerny who transplanted a lipoma for breast reconstruction for the first time, followed by other numerous colleagues who further developed the procedure of autologous fat relining. In 1985, Dr. Jeffrey Klein introduced tumescent local anesthesia, which is considered one of the greatest achievements in the development of liposuction.
However, when Dr. Mel Bircoll published his experience and results in 1987, autologous fat grafting for breast augmentation was banned by the American Society of Plastic Surgeons for years (1987-2008). This was due on the one hand to the unfortunately unspectacular results at that time, and on the other hand to the radiological-diagnostic limitations of being able to clearly distinguish fat necrosis from breast cancer. It took 20 years and the work of many other renowned colleagues (Dr. R. Khouri, Dr. S. Coleman, Dr. S. Spear or Dr. G. Rigotti and many more) to lift this ban and develop breast reconstruction with autologous fat into an established, standardized and safe procedure. One of the most important publications includes “Fat grafting to breast revisited: safty and efficancy” by Coleman [1]. The numerous studies were the basis of the 2009 Fat Graft Task Force of the American Society of Plastic and Reconstructive Surgeons, which concluded that lipofilling outcomes vary with surgeon technique and experience, but there is no evidence of an increased risk of breast cancer associated with breast lipofilling.
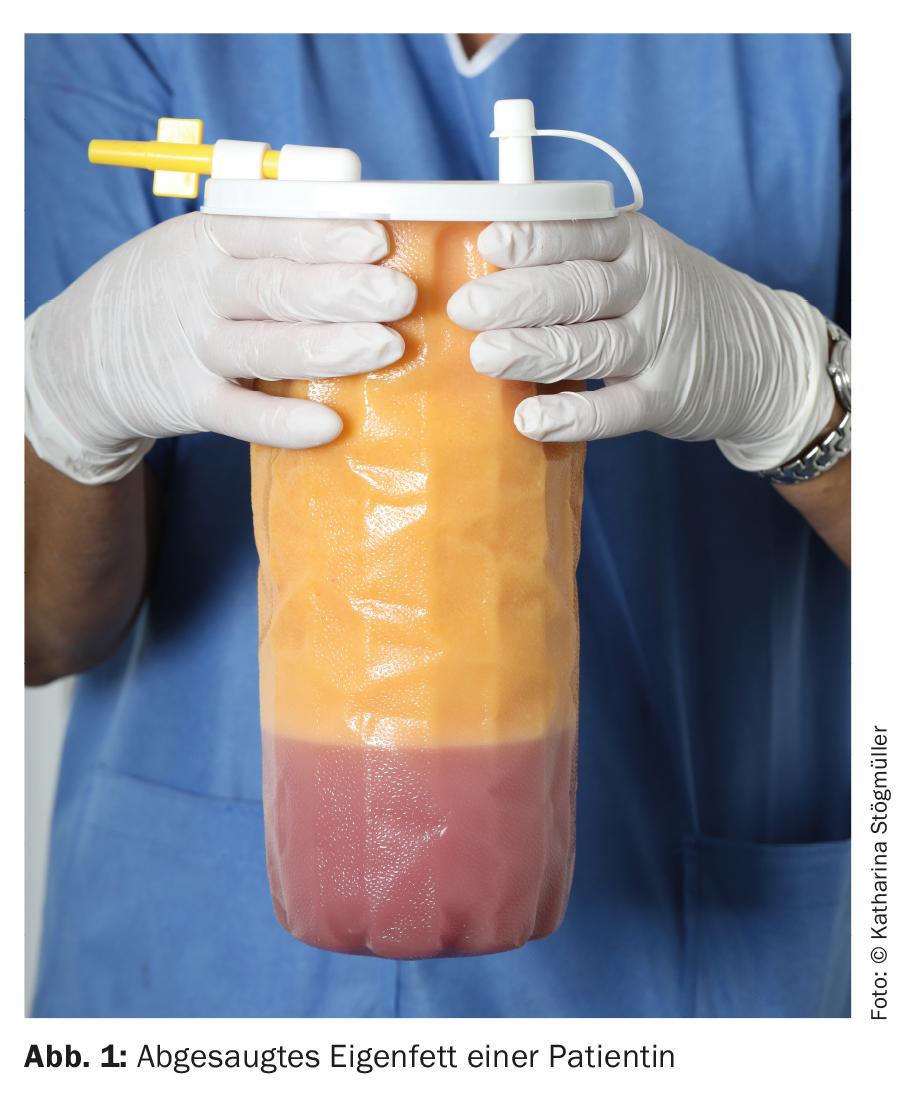
Radiological findings after lipofilling of the breast were listed in a publication by Carvial and Patino, among others [2]. The most common findings include benign bilateral scattered microcalcifications, radiolucent oil cysts. In 3 of 20 patients, the clustered microcalcifications resulted in a BIRADS III classification. There are now hundreds of studies that classify the procedure as harmless. Confusing calcification with intraductal carcinoma, for example, is now ruled out by the possibility of sonography, mammography, MRI and CT examinations and any necessary biopsies. Not only the technique of autologous fat implantation has changed from simple bolus injection with massive central necrosis that could be visualized radiologically to the three-dimensional fan technique. Of course, the equipment in radiology practices and institutes has also improved significantly, making the diagnosis of benign and malignant tumors of the breast more reliable. The fact that breast reconstruction with autologous fat (Fig. 1) is now routinely performed to reconstruct the breast after tumor disease is also an indicator of the safety of the procedure, although this should always be done in close consultation with the treating radiologist and oncologist.
Facts: Fat tissue
Adipocytes are among the largest cells in the body at 50-150 μ in diameter, with 500-1000 adipocytes in 1 mm3 of adipose tissue. When we transplant adipose tissue, it is important to remember that we are not transplanting isolated, pure fat cells, but it is a “dynamic tissue” that is additionally composed of fibroblasts, endothelial cells, preadipocytes, stem cells, and so on. This basically explains the high regenerative potential of lipofilling, which we can now establish without a doubt in volume replacement (atrophies, etc.) or also for functional improvement (e.g. injection into joints (off label) or scar treatment).
Aliquots up to 1 mm in diameter can survive in the breast after lipofilling – they connect to the vascular system and “grow on”. On the other hand, if larger pieces of tissue (more than 2 mm in diameter) are injected, central necrosis and side effects occur, which can be radiologically visualized as cysts, calcifications, and necrosis, for example.
On the other hand, from which sites we obtain the autologous fat in order to transplant it is still controversial. In my eyes, it strongly depends on the patient’s figure – do I have a woman in front of me with basically several “problem areas” and thus enough autologous fat or is the patient delicately built and one has to almost gather the autologous fat in the different areas.
In the former case, in any case, care should be taken to ensure that, as mentioned at the beginning, the patient’s proportions are in the best possible harmony after the procedure. For this, a consultative conversation and analysis of the entire body are essential. Whether the patient benefits from liposuction of the riding breeches or rather the hips and abdomen must therefore be considered on a case-by-case basis.
Indication
For those who do not want implants for breast augmentation, but would like a natural breast structure, this wish can often be fulfilled with autologous fat implantation. Lipofilling is used for mild to moderate augmentation of a small breast or a breast that has sagged after weight loss. Of course, an existing asymmetry can also be compensated or emerging implant borders can be concealed with autologous fat. If, for various reasons, an implant has to be removed, lipofilling can be used to restore the necessary volume to the breast. However, in these cases, 3-4 procedures are often necessary for a good result.
As already mentioned, breast reconstruction with autologous fat has long been established for reconstruction after tumor resection or ablation of the breast.
Advantages and disadvantages
The biggest advantage of lipofilling is that it is autologous material and therefore a “filler” with ideal properties and no allergy potential. At the same time, liposuction of a “problem area” improves the patient’s body proportions in a long-lasting way.
The procedure itself is minimally invasive, can easily be performed on an outpatient basis, and heals with virtually no visible scars (Figs. 2 and 3). The autologous fat is introduced into the breast with a thin cannula of about 1 mm and the incision sites for fat extraction are usually only a few mm narrow. This is appreciated by the majority of women, as repeated sessions are usually required to meet the expectations of most patients. Assuming that half to one cup size can be achieved per procedure, our patients are usually satisfied with the long-term result after the second procedure and are grateful not to have to accept a general anesthetic for it.

But there is no surgical procedure without disadvantages: Of course, there are also patients with a desire for breast augmentation in whom we can hardly obtain enough of their own fat to effectively perform lipofilling due to a lack of fat deposits on the body, or the patient’s expectations are an unrealistic one.
In addition, as with any surgical procedure, there is a learning curve and the procedure, performed under TLA (tumescent local anesthesia), is quite time and labor intensive. However, even if numerous operations have already been performed, the radiological follow-up examinations always reveal the images and findings described above. For some women, this can become a psychological burden, despite prior information.

The “accretion rate” of the injected autologous fat depends on various factors. However, the exact prediction of how much fat will actually grow cannot be given to the patient. This is of course a serious disadvantage compared to the use of implants. Patients who, for example, consume nicotine or start a diet directly after the procedure will, according to experience, achieve a worse outcome. We therefore strongly recommend abstaining from nicotine already in the run-up to the procedure!
Results
Again and again, one is confronted with the opinion that the results of the procedure are variable and unpredictable. The comparison is indeed not easy, if one looks at the literature in this regard: A survival rate of the adipocytes is given here with 15-83% (!). However, it is difficult to compare the individual publications because the result depends on various factors: the aspiration itself, the processing, the type of reinjection or, for example, the different pre- and post-treatment of the patients.
Even in the first surgical step, liposuction, there are many different methods of liposuction. While waterjet assisted liposuction (WAL) is preferred in some clinics, centers or surgeries, numerous colleagues perform liposuction with power assisted liposuction (PAL). In addition to the various methods, the treating physician also has access to various suction devices established on the market. For small regions, one can also resort to manual aspiration using syringe aspiration. Therefore, assuming that no specific suction method has become established, but that breast augmentation with autologous fat is performed differently in different practices and that the results are satisfactory, the experience and learning curve of the practitioner is obviously the more important factor for a good result.
In addition, care should always be taken to minimize fat cell damage at all steps! Low mechanical stress during fat extraction by adjusting the suction vacuum, use of gentle suction cannulas such as various small-lumen multihole cannulas, careful processing, and uniform, fan-shaped three-dimensional reinjection of fat cells should always be the top priority.
The aforementioned point of “careful processing” of the autologous fat when filling it into sterile syringes also offers another broad discussion. Looking at the literature, 31% of colleagues relied on pure gravity separation of the aspirated fat cells from the e.g. co-sucked local anesthetic and destroyed cell material. About the same number of colleagues (30%) centrifuge the extracted autologous fat before reinjection and about a quarter wash and filter the lipoaspirate before treatment. The rest is composed of other techniques or no manipulation. In Austria, routine enzymatic processing to obtain a larger quantity of stem cells has not become established or is offered only sporadically by colleagues. On the one hand, this is due to the significantly higher cost factor for the patient; on the other hand, the legal framework for the manipulation and reinjection of tissue has become stricter and can hardly be applied in an ordination/practice. However, the results of the procedure are very satisfactory even without additional stem cell addition (Figs. 4 and 5)!


Where we can obtain the “longest-lasting” autologous fat, as already mentioned, is also regularly discussed among experts. Many preferentially tend to remove on the inner sides of the knees or the fat on the abdomen. I personally, on the other hand, do not have a preference, but rather base my decision on the patient’s circumstances. The great advantage of the harmonious body proportion is, besides the primary goal of breast augmentation, for me one of the greatest benefits of the procedure. If patients have “problem areas,” we will discuss with them which area of the body to perform liposuction on. Whether this is the abdomen, the waist, the arms or the legs depends individually from woman to woman. If there is enough autologous fat for two procedures, the patient can enjoy a permanent improvement in her overall figure.
We see a special case in patients suffering from “lipohyperplasia dolorosa”. In my practice, we specialize in the surgical treatment of this condition. In this case of fat cell hyperplasia and hypertrophy (colloquially called “lipedema”), women suffer from a steadily increasing painful dysproportion of the extremities, caused by a genetic increase in fatty tissue at the extremities with a mostly extremely slim upper body. Patients often have 2-8 liters of fat suctioned out in multiple procedures to relieve symptoms (pain on pressure, pain on touch, tendency to hematoma, limited range of motion, etc.). During an international “lipedema” congress in Vienna in 2017, the question of whether this “diseased” fat can or should also be used for breast reconstruction was openly discussed. Only one colleague spoke out against its use at the time; the vast majority of around 100 colleagues, like myself, see no contraindication to using this fat for breast reconstruction.
Diagnostic survey/clarification
If the patient comes for a consultation on “breast reconstruction with autologous fat”, the indication and expectations must of course first be clarified precisely. As with any medical procedure, medical history and any possible contraindications are obtained. Especially in the case of aesthetic surgery, which in Austria is subject to the ÄsthOpG (Aesthetic Surgery Act, since January 2013), a particularly detailed explanation must be provided, preferably with standardized information sheets. In our office, all patients receive the so-called Diomed form, as well as a special, very comprehensive “information brochure”, which is tailored to the procedure and in which all details are once again discussed in accordance with the procedure, as well as the “OP passport”, which is obligatory in Austria.
Treatment
As mentioned, the performance of lipofilling varies among colleagues. I will therefore discuss the procedure here as it is performed in our practice on an outpatient basis.
Preoperative preparation for ASA1 patients includes a recent mammogram, blood findings (red and white blood counts, coagulation), and routine per os shielding with an antibiotic (Augmentin® penicillin and clavulanic acid) for one week, starting the evening before surgery. (Thromboprophylaxis is started subcutaneously on the first postoperative day with a low molecular weight heparin).
Immediately before the procedure, after checking all findings and consents, only per os sedation with 6mg of Lexotanil, the exact photo documentation and the placement of a venous access is performed. After that, the place of fat extraction and the breast is marked, which is also accurately photo-documented, sterilely washed and covered. The procedure is performed in my office as an outpatient under pure local anesthesia (TLA), and we use Klein’s mixture, without cortisone (1000 ml NaCl plus 50 ml Xylanest purum 1%® plus 1 ml Suprarenin® plus 10 ml NaBic 8.4%). Injecting anesthesia takes approximately 30-60 minutes and is performed in my office by a specially trained scrub nurse using an infiltration pump and a 20G needle. After an exposure time of about 30 minutes, I suction out the autologous fat with the PAL (power assisted liposuction) system (Microair®) using 3-mm multihole cannulas.
The extracted autologous fat is left to stand for about 20 minutes to separate it from the local anesthetic that was partially aspirated at the same time, washed with saline, and then filled into 20 5 ml Luer Lock syringes. The use of small syringes reduces the pressure on the fat cells during reinjection and enables an even application.
This is done in my practice with a Tulip®1 .2-mm cannula using a three-dimensional tunnel technique to evenly replant the autologous fat. The advantage of this is undoubtedly the scarless technique of injection. For the insertion of the blunt cannula, only a puncture of the skin with a 20G needle is necessary.
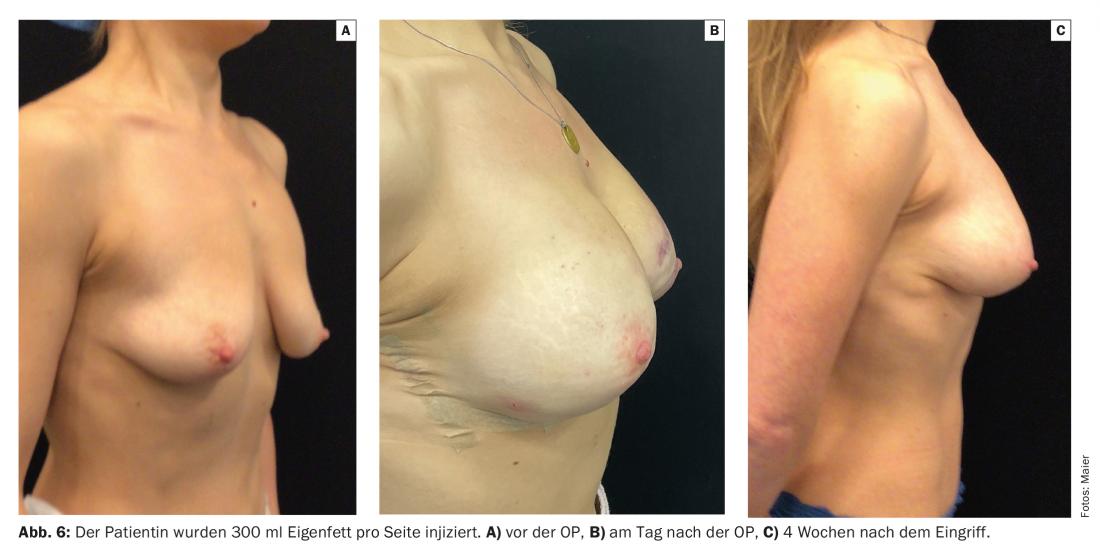
Depending on the size of the breast, about 100-500 ml of fat is injected per side. The accesses are placed here on both sides of the nipple. From here, the upper two quadrants of the breast can be relined well. Lipofilling of the outer lower breast quadrant and the area under the mammary gland is performed from a lateral approach just above the inframammary fold. The final approach is usually medial to treat the medial inferior quarter.
After the treatment, the puncture sites on the breast are treated with sterile plasters, compresses as well as light compression. The liposuction region is treated similarly, but with more absorbent fleece and compression garments for 4 weeks, since when TLA is used, the injected local anesthetic leaks back over the incision sites much more than at the breast. Patients may therefore have to reconnect several times at home, but this can usually be done without any problems.
Complications
Patients should expect bruising, swelling, and a small amount of wound pain. Basically, however, all general complications (infection, thrombosis, etc.) must be explained, as we know them from other surgical procedures. In any case, the radiologist must be informed about lipofilling during the following routine radiological control examinations of the breast. Benign microcalcifications, oil cysts or necrosis could otherwise be misinterpreted.
As a rule, patients are fully fit for social life again after a few days. Sports can be restarted in light form after 1 week, sauna and similar treatments should be skipped for 3 weeks. Compression garments as with any liposuction at the site of fat extraction for a few weeks or a sports bra to support the breasts are quite sufficient and hardly disturb the patients in their daily routine.
Conclusion
The patients gladly take advantage of the minimally invasive procedure in my office and are very satisfied with the long-term results. About two-thirds of patients have 2 procedures performed about 3 months apart, and one-third are satisfied after the first lipofilling. However, breast augmentation with autologous fat leads not only to a long-lasting improvement in body proportion, but also to an increase in self-esteem. Conclusion: Small interventions can achieve a lot, because who feels good in his body, radiates this!
Take-Home Messages
- Lipofilling has been one of the top 5 aesthetic surgical procedures worldwide for many years and has long since established itself among cosmetic surgeries.
- Lipofilling involves the use of autologous material and therefore a “filler” with ideal properties and no allergic potential. At the same time, liposuction of a “problem area” improves the patient’s body proportions in a long-lasting way.
- The procedure itself is minimally invasive, can be performed on an outpatient basis, and heals with virtually no visible scars. The autologous fat is inserted into the breast with a cannula that is only about 1 mm thin, and the incision sites for fat extraction are usually only a few mm narrow.
- However, there are also patients in whom, due to a lack of fat deposits on the body, hardly enough of their own fat can be harvested to create an
- lipofilling effectively, or the patient’s expectations are unrealistic.
- As a rule, patients are fully fit for social life again after a few days. Sports can be restarted in a light form after one week, sauna and similar treatments should be skipped for 3 weeks.
Literature:
- Coleman S, et al: Fat grafting to breast revisited: safty and efficancy. PRS 2007; 119(3): 775-785.
- Carvial J, Patino J: Mammographic findings after breast augmentation with autologous fat. Aesthetic Sugery journal 2009; 28(2): 153-162.
DERMATOLOGIE PRAXIS 2022; 32(3): 14-19










