Cannabis is one of the most common psychotropic substances in the world, along with nicotine and alcohol. What are the effects of regular cannabis use on the likelihood of developing psychosis? How does it affect those with a predisposition or those who already have the disease?
Cannabis is one of the most commonly used psychotropic substances in the world, along with nicotine and alcohol. While consumption in Switzerland increased during the 1990s and at the beginning of the new millennium, a decline is now evident again. According to the Swiss Health Survey, in 2012, among 15- to 19-year-olds, approximately 10% of men and just under 2% of women, and among 20- to 24-year-olds, approximately 9% of men and 4% of women, used cannabis at least once a month in the past 12 months [1]. Among men aged 25 to 29 years, this prevalence was approximately 9%; among women in the same age group, it was an estimated 2.5%. Among those over 34 years of age, few individuals were still found to be current cannabis users [1].
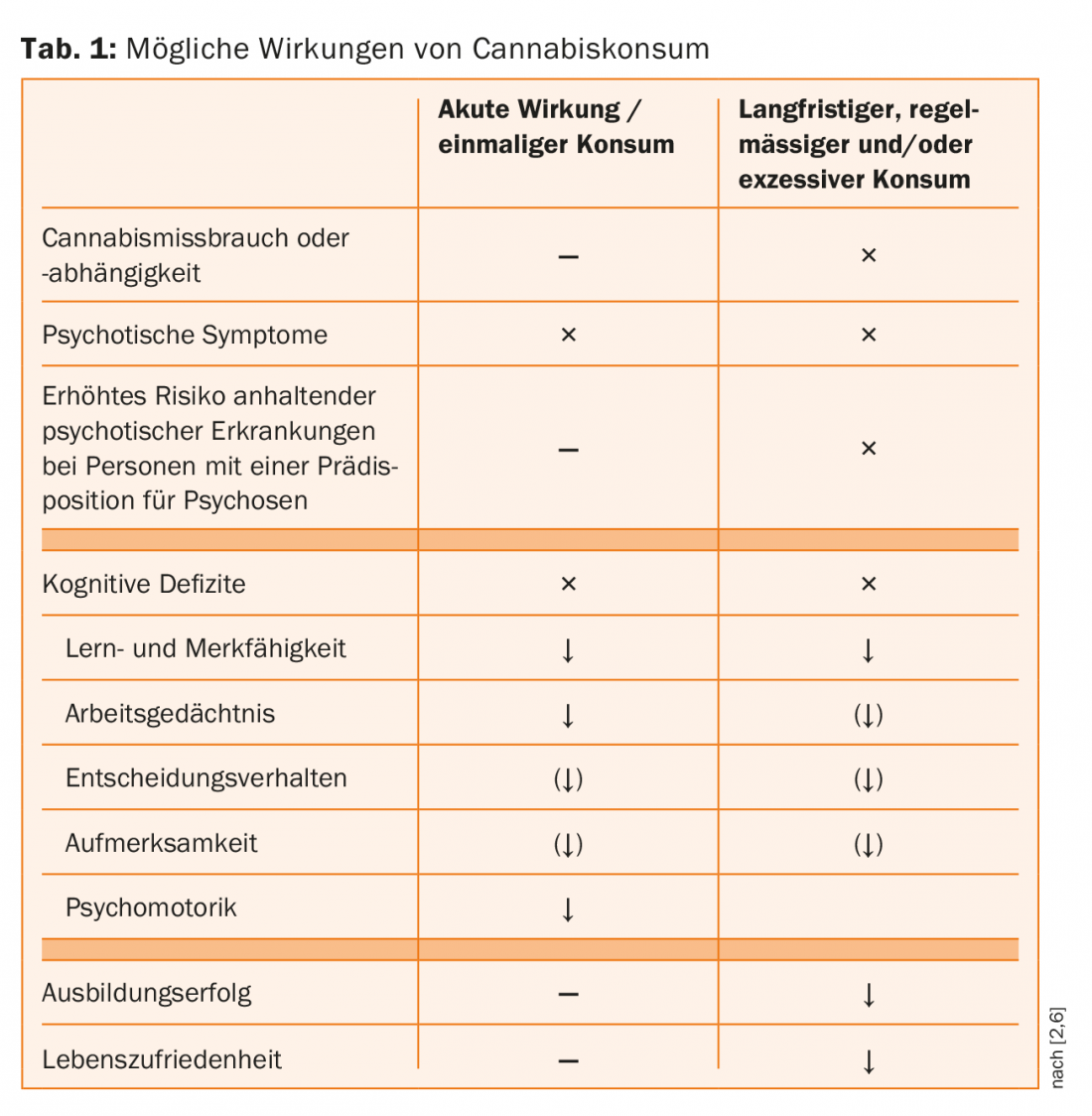
The main cannabinoids found in cannabis are tetrahydrocannabinol (THC) and cannabidiol (CBD). The use of THC produces the “high” experienced by most users, with euphoria, increased sociability, and feelings of heightened insight. At the same time, however, use can also be associated with acute and longer-term negative consequences (tab. 1). These are primarily cognitive deficits, school and educational difficulties, dependence disorders, psychotic symptoms and – in individuals with a predisposition to psychosis – potentially also persistent psychotic disorders [2].
Cannabis use and psychosis
The relationship between cannabis and psychosis has been the subject of a large number of studies in recent decades. Patients with a (first episode of) schizophrenic psychosis have significantly higher rates of current (approximately 30-40%) and lifetime (up to 60-80%) [3,4] cannabis use than individuals in the general population [5].
Higher rates of current (around 30%) and lifetime (around 50%) cannabis use are also found in patients with a risk status for psychosis, i.e., patients suspected of having an onset of psychosis [6].
In experimental studies, healthy volunteers given oral and intravenous THC developed psychotic symptoms [7].
Cannabis as a risk factor for schizophrenic psychosis.
Several findings point to the role of cannabis as a potential risk factor for schizophrenic psychosis. Longitudinal studies showed that cannabis use in these patients is usually present before the diagnosis of schizophrenic disorder [8]. It is now also well established that regular and/or excessive cannabis use is associated with an increased likelihood of developing a long-term psychotic disorder of the schizophrenic type [2,9].
A risk group with regard to psychotic disorders associated with regular cannabis use are individuals with a predisposition to psychosis [2]. In individuals at genetic risk for psychosis, regular cannabis use may increase both the likelihood of developing clinical risk status for psychosis and the occurrence of persistent psychotic illness [2,9,10]. In particular, there is much evidence that the onset or presence of regular cannabis use as early as early adolescence potentially increases the risk of schizophrenic psychosis in vulnerable individuals [11]. In addition, the more extensive the cannabis use, the higher the likelihood of psychotic illness. To date, it is still unclear what level of cannabis use is “unproblematic” [12–14].
Cannabis potency
THC can cause acute psychotic symptoms in high doses, and regular use of high-potency cannabis appears to increase the likelihood of psychotic illness [15]. Against the background of the change in the composition of consumed cannabis in recent decades towards higher THC and lower CBD content [12], this finding is to be taken particularly seriously. CBD appears to partially attenuate the negative effects of THC, thus potentially having an antipsychotic effect, among others, without affecting the subjectively desired effects of THC.
Potential, neurobiological mechanisms of action.
The fact that THC can induce psychotic symptoms and that, in animal models, administration of exogenous cannabinoids usually results in increased dopamine release [7] led to the hypothesis that cannabis is associated with persistent psychotic disorders via this dopaminergic mechanism of action. Although this explanation seems plausible in the context of the dopamine hypothesis of schizophrenia, current research suggests that increased dopamine release is only one of several possible neurobiological bases here. Patients with chronic abuse or cannabis dependence seem to be more likely to develop a hypodopaminergic state, but with increased sensitivity of dopamine D2/D3 receptors, making them vulnerable to psychosis [7].
Cannabis use and earlier onset of schizophrenic psychosis.
Regular cannabis use appears to be associated with earlier onset of schizophrenic psychosis [16]. The use of high-potency cannabis and heavy use to the extent of cannabis use disorder seem to be associated with an even earlier onset of schizophrenic psychosis, especially in women. Previous studies showed an approximately six-year earlier onset in this regard [4,15]. This has potentially far-reaching consequences for the further course, especially in psychosocial terms, as these patients are in a critical phase of life.
Influence of cannabis on the course in already ill patients
In patients with schizophrenic psychosis, regular cannabis use is associated with more severe psychotic symptoms and a worse course [17,18]. A study that followed patients with schizophrenic psychosis from their first hospitalization over ten years found evidence of a bidirectional association, i.e., increased cannabis use followed by more psychotic symptoms and, conversely, more severe psychotic symptoms followed by increased cannabis use [18]. The latter could be explained in terms of the self-medication hypothesis, which states that patients try to reduce psychotic symptoms and their accompanying symptoms, such as anxiety and depressive symptoms, by using cannabis. However, the evidence for this hypothesis is rather weak [17]. In patients with a risk status for psychosis, those with regular cannabis use show more severe (subclinical) psychotic symptomatology [6].
Summary
Regular use of cannabis may be associated with various negative consequences such as cognitive impairment, school and educational difficulties, and cannabis dependence [2]. In addition, cannabis can cause acute psychosis when administered acutely.
In addition, regular as well as heavy cannabis use – especially in individuals with a predisposition to psychosis and use already in early adolescence – is associated with an increased likelihood of developing a persistent psychotic illness. Cannabis with a high THC content appears to be even more strongly associated with psychotic symptomatology. This is particularly relevant in light of the increased prevalence of high-potency cannabis (also called “skunk” or “spice”) and the increasing THC and decreasing CBD content of cannabis in general.
Several findings, such as the temporal relationship, the presence of a dose-response relationship, and the earlier onset of schizophrenic psychosis in regular cannabis users, as well as, last but not least, the interference with dopaminergic transmission, point to the role of cannabis as a risk factor and/or trigger for schizophrenic psychosis – at least in individuals prone to such disorders.
Whether this is also a causal relationship, whether schizophrenic psychoses are also triggered in people who are not predisposed to this, has not been clearly clarified. One of the difficulties in exploring the causal relationship is the influence of a large number of confounding variables. An alternative, possible explanation would also be that common etiological factors play a role with regard to the association between cannabis use and psychosis. Individuals who exhibit vulnerability to psychosis may be more prone to use cannabis regularly and, at the same time, may be more susceptible to persistent psychotic illness due to their vulnerability [5].
Although the causality of the relationship between regular or heavy cannabis use and the occurrence of long-term schizophrenic psychosis has not yet been clearly established, the available evidence suggests that chronic cannabis use can trigger such disorders in vulnerable individuals. In any case, the public should be made aware of the harmful effects of regular cannabis use – also with regard to the risk of persistent psychotic disorders [9].
Take-Home Messages
- Patients with a suspected onset of psychosis and patients with a (first episode of a) psychotic disorder from the schizophrenic group use cannabis significantly more often than persons of the same age in the general population.
- Regular cannabis use is associated with an increased likelihood of the onset of persistent psychotic illness-particularly in individuals predisposed to psychosis and when use occurs in early adolescence.
- Patients with regular cannabis use before the onset of schizophrenic psychosis have a lower average age of onset.
- Patients with schizophrenic psychosis who regularly use cannabis show a worse course with more pronounced psychotic symptoms.
Literature:
- Addiction info suisse, Notari L: Summary results of the 2012, 2007, 2002, 1997, and 1992 Swiss health surveys regarding the use of tobacco, alcohol, medications, and illicit drugs. Addiction info suisse 2014.
- Volkow ND, et al: Adverse health effects of marijuana use. N Engl J Med 2014; 370(23): 2219-2227.
- Bugra H, et al: Cannabis use and cognitive functions in at-risk mental state and first episode psychosis. Psychopharmacology 2013; 230(2): 299-308.
- Crocker CE, Tibbo PG: The interaction of gender and cannabis in early phase psychosis. Schizophr Res 2017.
- Ksir C, Hart CL: Cannabis and psychosis: a critical overview of the relationship. Curr Psychiatry Rep 2016; 18(2): 12.
- Carney R, et al: Cannabis use and symptom severity in individuals at ultra high risk for psychosis: a meta-analysis. Acta Psychiatrica Scandinavica 2017.
- Murray RM, Mehta M, Di Forti M: Different dopaminergic abnormalities underlie cannabis dependence and cannabis-induced psychosis. Biol Psychiatry 2014; 75(6): 430-431.
- Bugra H, et al: Can cannabis increase the risk of psychosis? Fortschr Neurol Psychiatr 2012; 80: 635-643.
- Gage SH, Hickman M, Zammit S: Association Between Cannabis and Psychosis: Epidemiologic Evidence. Biological Psychiatry 2016; 79(7): 549-556.
- Stowkowy J, Addington J: Predictors of a clinical high risk status among individuals with a family history of psychosis. Schizophr Res 2013; 147(2-3): 281-286.
- Casadio P, et al: Cannabis use in young people: the risk for schizophrenia. Neurosci Biobehav Rev 2011; 35(8): 1779-1787.
- Curran HV, et al: Keep off the grass? Cannabis, cognition and addiction. Nat Rev Neurosci 2016; 17(5): 293-306.
- Kraan T, et al: Cannabis use and transition to psychosis in individuals at ultra-high risk: review and meta-analysis. Psychological medicine 2016; 46(04): 673-681.
- Marconi A, et al: Meta-analysis of the Association Between the Level of Cannabis Use and Risk of Psychosis. Schizophrenia Bulletin 2016; 42(5): 1262-1269.
- Di Forti M, et al: Daily Use, Especially of High-Potency Cannabis, Drives the Earlier Onset of Psychosis in Cannabis Users. Schizophrenia Bulletin 2014; 40(6): 1509-1517.
- Large M, et al: Cannabis Use and Earlier Onset of Psychosis. Archives of General Psychiatry 2011; 68(6): 555-561.
- Murray RM, et al: Traditional marijuana, high-potency cannabis and synthetic cannabinoids: increasing risk for psychosis. World Psychiatry 2016; 15(3): 195-204.
- Foti DJ, et al: Cannabis Use and the Course of Schizophrenia: 10-Year Follow-Up After First Hospitalization. American Journal of Psychiatry 2010; 167(8): 987-993.
Additional literature can be requested from the authors.
InFo NEUROLOGY & PSYCHIATRY 2018; 16(1): 14-17.











