From April 11-13, 2013, the Review Course in Clinical Cardiology was held in Zurich for the eleventh time. Renowned experts dealt with a variety of topics from the field of “Cardiac Therapy” in short presentations. We report on the highlights.
At the beginning of his presentation, PD Dr. med. Bernhard Hess, Zurich, introduced an anecdote. In 1931 Arsenal FC got a new coach who was convinced that sunlight was important for “strong bones”, the players received regular exposure to sunlight – Arsenal FC became English champions. Coincidence?
Vitamin D deficiency – what is the benefit of substitution?
The definitions for vitamin D insufficiency resp. -deficiency are as follows:
- Normal vitamin D reserves: 25-OH-D >75 nmol/l
- Vitamin D insufficiency: 25-OH-D 50-75 nmol/l
- Vitamin D deficiency: 25-OH-D <50 nmol/l
In Switzerland, according to the latest data, only 25.3% of the population have normal vitamin D levels, 36.5% have insufficiency, and 38.2% have manifest vitamin D deficiency. Two-thirds of all elderly people are undersupplied with vitamin D. One reason for this is the decline in sun exposure due to the risk of skin tumors.
More than 90% of vitamin D in the organism comes from the precursor cholecalciferol, which is formed in the skin under UV-B irradiation and metabolized in the liver to 25-hydroxy vitamin D. Only a few percent of 25-OH vitamin D is converted to endocrine (i.e., via blood) active 1,25-dihydroxyvitamin D (calcitriol) by renal 1-α-hydroxylase; 80% of calcitriol is formed locally in tissues (endothelium, vascular smooth muscle, skin, pancreas) by tissue 1-α-hydroxylase. Calcitriol exerts numerous auto- and paracrine functions that have not been fully explored. Thus, vitamin D deficiency leads to a decrease in muscle strength, clustered diabetes mellitus, stimulation of the renin-angiotensin-aldosterone system, immune dysfunction, and a decrease in antitumor activity. Epidemiologically, vitamin D deficiency increases all-cause mortality as well as mortality from cardiovascular disease, cancer, and respiratory disease.
Numerous studies show that daily doses of vitamin D up to 4000 IU are safe, even during pregnancy and lactation. However, a high dose of 500,000 IU of vitamin D administered annually has led to increased falls and fractures in women over 70 years of age. Therefore, vitamin D substitution at shorter intervals is recommended today. This measure is simple, inexpensive and useful.
Achieving consistent vitamin D levels between 75 and 100 nmol/l is most useful.
Statins – more harm than good?
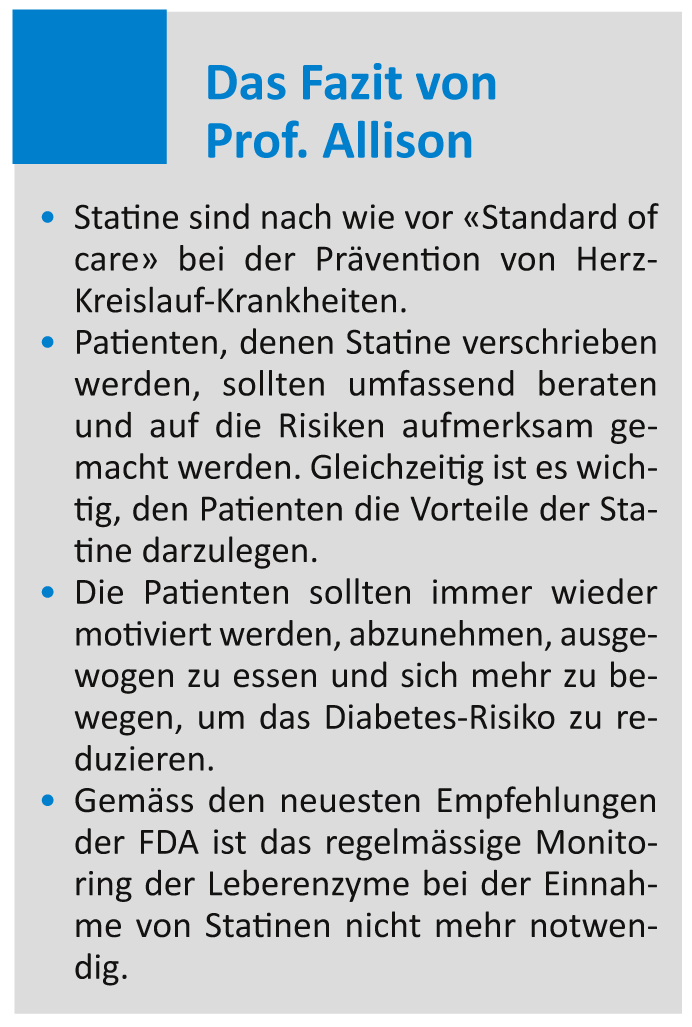
Prof. Thomas Allison, MD, from Rochester, USA, took up the cudgels for statin therapy. Although many randomized clinical trials show the benefit of statins in the primary and secondary prevention of cardiovascular events, controversy remains about their use. The main problems with statins are myopathies, a possible increased risk of cognitive impairment, and increased risk of diabetes.
Myopathies actually occur in 4-5% of all statin users. However, in the vast majority of cases, this muscle pain is CK negative and has no effect on muscle strength and endurance. Myositis with CK elevation as well as rhabdomyolysis are very rare events that primarily affect individuals on very high statin doses. Possible cases of dementia secondary to statin use have been reported to the FDA, but currently there is no convincing evidence that statins cause cognitive decline. Observational studies tend to provide evidence that statins may delay certain forms of dementia.
The risk of developing type 2 diabetes is increased when taking (especially high doses of) statins. However, this risk increase is linked to other risk factors such as obesity, impaired glucose tolerance, hypertriglizeridemia, and hypertension. For the risk of diabetes to actually increase with statin use, three of these four risk factors must be present. Furthermore, it is important to keep in mind that for every case of diabetes triggered by statins, 2.5 deaths or cardiovascular events were prevented.
Vitamin K antagonist or new anticoagulant?
The vitamin K antagonists (VKA) have commonly known drawbacks and are unpopular with many physicians and patients, said Prof. Bernard J. Gersh, MD, of Rochester, USA. Now that new oral anticoagulants (NOAKs) have entered the market, experts and the media are already proclaiming the “retirement of VKA.” Prof. Gersh believes this is unrealistic, as VKAs also have important advantages: they are inexpensive, widely known, effective, and relatively safe. In some patients, their use remains superior to therapy with NOAKs.
Nevertheless, the RE-LY study and the marketing authorization of dabigatran (Pradaxa®) have heralded a new era. The advantages and disadvantages are shown in Table 1.

Dabigatran, rivaroxaban (Xarelto®), and apixaban (Eliquis®) have all shown a reduced risk of bleeding, and they are more effective or at least as effective as warfarin.
Liver toxicity due to drugs
Drug induced liver injury (DILI) was explained by Prof. Dr. med. Res Jost, Winterthur. 20% of all hospitalizations for jaundice, 10% of all cases of acute hepatitis, and 20-50% of all fulminant liver failures are caused by drugs. In 80% of patients, paracetamol is responsible for this, which is not infrequently taken with suicidal intent. The spectrum of manifestations of DILI ranges from minor elevation of liver enzymes to liver failure. Early detection is critical for prognosis. DILIs are also the most common cause of market withdrawal for drugs that have already been introduced.
DILI are classified by cause (hepatocellular, cholestatic, mixed) and duration (acute: up to 6 weeks; subacute: 6 weeks to 6 months; chronic: more than 6 months). Liver enzymes are always elevated. If the bilirubin >50 mmol/l and/or the INR >1.5 increases, this is an indication of a higher severity. If all three parameters are elevated, hospitalization is required.
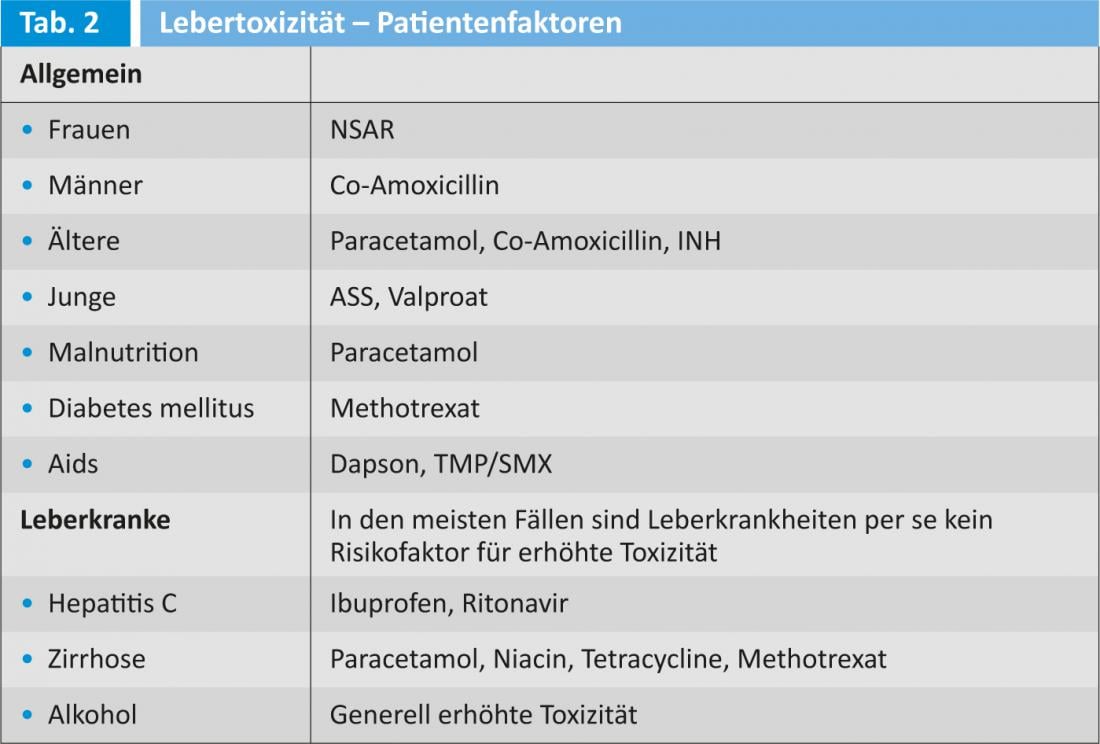
A DILI is a diagnosis of exclusion: is there another cause of liver damage (viral hepatitis, autoimmune disease, alcohol toxicity?) Various patient factors increase the risk for liver toxicity (Table 2).
Liver enzymes increase slightly and transiently in 10% of patients taking statins. The FDA recently decided that routine monitoring of liver enzymes during statin therapy is not useful because liver damage resulting from statin use is rare and cannot be predicted in individual patients. Liver values should therefore be checked at the start of statin therapy; if these are normal, no further checks are necessary unless there is a clinical suspicion of liver toxicity. Liver toxicity is not common with the new anticoagulants. The speaker recommended the following websites that provide more information about the problem of DILI:
More potent is not always better
Prof. Dr. med. Hans Rickli, St. Gallen, provided information on the different platelet (Tc) aggregation inhibitors and their application. Current ESC recommendations in STEMI, NSTEMI, and perioperatively are complex, as are individual hospital guidelines on how to proceed in acute ACS; multiple antithrombotic treatment regimens are possible.
- Prasugrel or ticagrelor is superior to clopidogrel according to the TRITON and PLATO studies, respectively.
- A direct comparison between prasugrel and ticagrelor in the acute setting does not exist. Regarding the assessment of the benefit of Tc aggregation inhibition, the risk of bleeding is crucial, and the TRITON and PLATON trials cannot really be compared because different patient groups were studied.
- A clear simple strategy may be helpful for successful network treatment.
- Clopidogrel is still indicated or NOAKs should not be used if there are contraindications to the new Tc aggregation inhibitors or if oral anticoagulation is required.
- Combination with new OAKs is also not evidence-based.
- In elective PCI with stent implantation, no conclusive data exist yet for the use of new Tc aggregation inhibitors.
- Clopidogrel in addition to aspirin is still indicated.
- No indication for systematic use of the new Tc aggregation inhibitors in stable CHD.
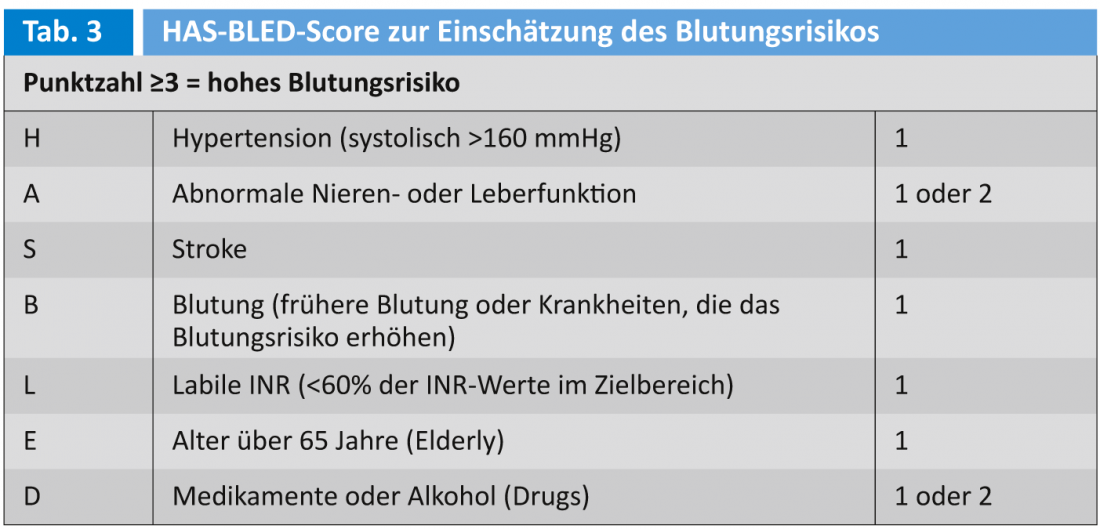
The WOEST trial (patients after stenting) showed that bleeding and death were more frequent under triple therapy (oral anticoagulation, clopidogrel, ASA) than under dual therapy (DAPT: oral anticoagulation, clopidogrel). There is evidence that omitting ASA may improve it (lower risk of bleeding without increasing the risk of stent thrombosis), but the situation is not clear on this. In assessing the risk of bleeding, the HAS-BLED score can help (Table 3).
Studies on the duration of antithrombotic therapy after drug-eluting stent (DES) insertion have shown that DAPT is most beneficial between six and 12 months. Shorter DAPT increased the risk of death or myocardial infarction, and longer DAPT increased the risk of bleeding.
The PPI controversy is not quite over yet. It is valid to use pantoprazole when clopidogrel is administered.
Source: 11th Zurich Review Course in Clinical Cardiology, April 11, 2013, Zurich.