Abdominal complaints have a high prevalence and the diagnosis is very multilayered and complex. In addition to a wide range of possible somatic causes, psychosocial factors often play a role.
The workup of abdominal pain requires consideration of a variety of factors to decide what further diagnostic testing should be ordered and whether a patient should be referred to a specialist. Therefore, a multidisciplinary approach to this issue is extremely important.
Experience values of surgery
If cholecystitis is suspected, the patient should be referred to an emergency department, says Cornelia Frei-Lanter, MD, senior physician, Clinic for Visceral and Thoracic Surgery, Winterthur Cantonal Hospital. Differential diagnostic clues for distinguishing between cholecystitis and cholecystolithiasis include the type of pain (continuous vs spontaneous) and the presence of fever (possible vs absent). With regard to sigmoid diverticulitis, according to current knowledge, it is primarily the degree of suffering that is decisive for the indication of surgical intervention and not the number of relapses [1]. If passenger dysfunction is present, Dr. Frei-Lanter recommends hernia identification and reduction. The diagnostic gold standard is computed tomography, and abdominal radiography is not recommended.
Gastroenterological perspective
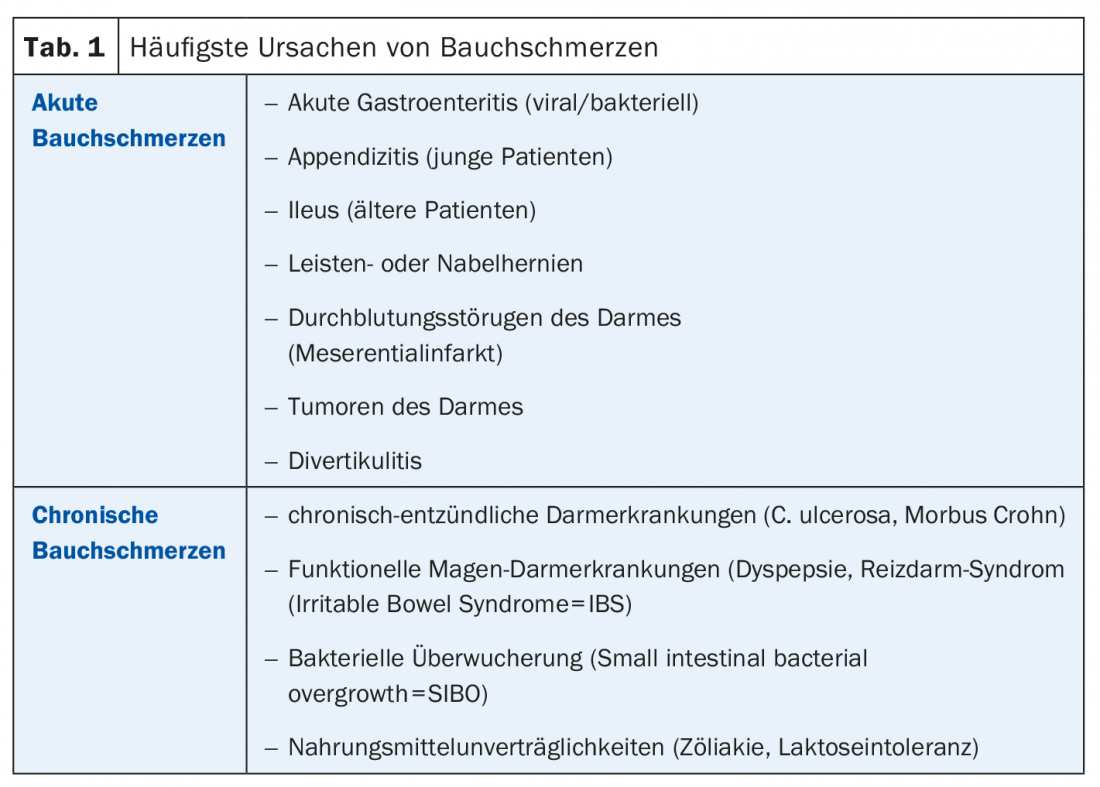
Henriette Heinrich, MD, senior physician, Stadtspital Triemli, Zurich, explained the criteria for deciding whether endoscopy is required for abdominal complaints: In addition to pain intensity and location (right upper abdomen), there are certain anamnestic criteria (e.g., age >50-year-old, fever, chronic diarrhea, anal bleeding, dysphagia) in combination with findings in the blood count (e.g., anemia, iron deficiency, leukocytosis, and normal deviations of ESR, CRP, and TSH/T4), which are relevant. Acute or chronic abdominal pain can conceal a variety of diseases (Tab. 1). If celiac disease is suspected, antibody determination of TTG (IgA and IgG based) is recommended. IBS and SIBO (small intestinal bacterial overgrowth) are functional gastrointestinal disorders with a large symptom overlap: abdominal pain, bloating, diarrhea. It is believed that there is an etiologic link and that it is possible to influence it with antibiotics, but their efficacy is controversial.
Rheumatological perspective
Pius Brühlmann, MD, specialist in rheumatology, Bethanien Private Clinic, reported on a case of lumbo-spondylogenic syndrome with lower abdominal pain and postural weakness, in which mobilization and physiotherapy (strengthening of abdominal muscles) resulted in considerable symptom relief. In cases where drug treatment is necessary, the effect/side-effect profiles of the various preparations should be weighed up, with the dosage also playing an important role. The use of nonsteroidal anti-inflammatory drugs (NSAIDs) increases the risk of dyspeptic symptoms and ulceration [4]. Paracetamol can lead to gastrointestinal ulcer complications [4] and COX2 inhibitors also carry a risk of adverse gastrointestinal effects.
Interesting facts from psychosomatics
Prof. Dr. med. Stefan Büchi, Medical Director of the Hohenegg Private Clinic, pointed out that abdominal complaints often have a non-organic cause. For the new edition of the ICD (ICD-11), it is therefore planned to introduce a new classification: “Bodily Distress Syndrome”. Stress theories are useful explanatory models for abdominal pain resulting from psychosomatic factors, Prof. Büchi said. Psychological stress can be assessed by the general practitioner, for example, using the PHQ questionnaire (“Patient Health Questionnaire”). If necessary, psychotherapy may be indicated. Research findings show that especially the effect factors plausibility (understanding of connection between stress and reaction), resilience promotion (strengthening of psychological resilience) and patient-therapist relationship can contribute to symptom relief [5]. If necessary, low-dose psychotropic drugs can also be used (e.g., the neuroleptic quethiapine or the antidepressant amitriptyline), the speaker explained.
Source: VZI Symposium, January 31, 2019, Zurich
Literature:
- Andeweg CS, et al: Clin Gastroenterol Hepatol 2016; 14(1): 87-95.e2. Epub 2015 Mar 10. doi: 10.1016/j.cgh.2015.02.040.
- Heinrich H: Slide presentation. Parallel symposium: One symptom – four perspectives. VZI Symposium, 31.01.2019, Zurich.
- Oliver R, Vavricka S: Swiss Review of Medicine 2010; 99(7): 399-408.
- Liechti ME: Switzerland Med Forum 2014; 14(22-23): 437-440.
- Wampold BE: World Psychiatry 2015; 14(3): 270-277.
HAUSARZT PRAXIS 2019; 14(3): 33











