When caring for drug addicts with somatic illnesses, the issue is often which medical professional should take on which tasks. In principle, the answer is: everyone does what they can. However, the general practitioner has a very central role, as patients often do not keep appointments with specialists and scheduled procedures cannot be performed as a result. If possible, there should be a central reference person who takes care of everything. More important than the diagnosis itself is often the clinical course. Recognizing “red flags” and a prudent watchful-waiting strategy are key here. Caution and restraint during opiate withdrawal: lack of tolerance and sleep will quickly lead to death if relapse occurs.
Drug dependence is frequently accompanied by somatic diseases (Table 1) . Most of the clinical pictures are also known to us from non-drug patients. However, the disease of addiction and often psychological comorbidities pose special challenges, and often, in order to be successful, one must deviate from the usual diagnostic-therapeutic path.
The most important thing is certainly that a patient with a serious somatic problem comes to medical help at all. It is not uncommon for drug patients to shy away from the consulting room, preferring to present findings or symptoms to us at the door. Initial triage with the aim of identifying “red flags” should therefore be carried out as quickly as possible and at low thresholds. When referring to the normal procedure with an appointment, important diagnoses are often missed or made too late (e.g., spondylodiscitis) because patients do not come.
Disease patterns – When does it make sense to involve specialists?
The clinical pictures are very diverse and multimorbidity is the rule. The question “Who does what?” is particularly pressing here. Involving specialists often leads to frustrating experiences on all sides, as deadlines and the proposed procedure cannot be met. In practice, it is best if the patient has a reference person who takes care of all the problems.
In this situation, it is particularly important for the general practitioner to make himself a “specialist” in the clinical pictures presented by the patient as quickly as possible and to try to develop a procedure tailored to the needs and possibilities. Social work skills and their application are also important.
So the question “Who does what?” can be answered with “Everyone does what they can.” It is important to note that the question of “proficiency” is not answered by a certificate of proficiency, but by the question being asked. For example, ultrasonography requires a great deal of expertise when asking about fetal malformations. In a woman with liver disease who complains of a sudden fat belly, the differential diagnosis of ascites, pregnancy, fat belly can also be decided with an old device and by someone with little experience. Similarly, measuring QTc time in a methadone patient with questionable syncope does not require a cardiologist.
Unlike a polyclinic workup, we often don’t have to make a diagnosis; we just can’t miss anything serious. With a watchful-waiting strategy, we can wait for the usually favorable spontaneous course of events. Many examinations can be saved in this way. It is important to know the patient well and to have a relationship of trust. The appropriate distance in the relationship is equally central. Even though it is usually better to stick with the “you”, a good respectful relationship can develop.
Especially in Watchful Waiting, accessibility is central. Pictures sent via smartphone often help as well. When a patient has landed in a clinic on an emergency basis, short phone calls with the clinician are very helpful, especially for complex problems. In my experience, the issuance of the private cell phone number is hardly ever misused.
Although addictive disorders are actually classified as mental illnesses, drug patients receive only limited care from outpatient psychiatrists and are largely treated by general practitioners or, in urban areas, by specialized centers. Regular short talks – e.g. on the occasion of the personal dispensing of substitution medication – are helpful and psychological or somatic problems can be identified at an early stage.
HIV and hepatitis
Treatment for HIV and hepatitis has made huge strides in the last few decades and has become much easier. In particular, continuation of established HIV therapy can be well managed by an experienced general practitioner. The most important thing is that the patient has access to therapy in the first place and takes it.

Because of the high costs, the treatment of HCV infection is currently more of a health policy problem than a medical one. Because drug costs, similar to software, are largely developmental rather than production-related, the approaches of treating all HCV RNA-positive vs. only those at risk of cirrhosis would theoretically be similarly expensive. Treatment of all HCV RNA-positive individuals would have epidemiologic benefits. The new drugs are so effective, convenient to take, and have few side effects that treatment requires little special expertise compared with previous interferon-based therapies.
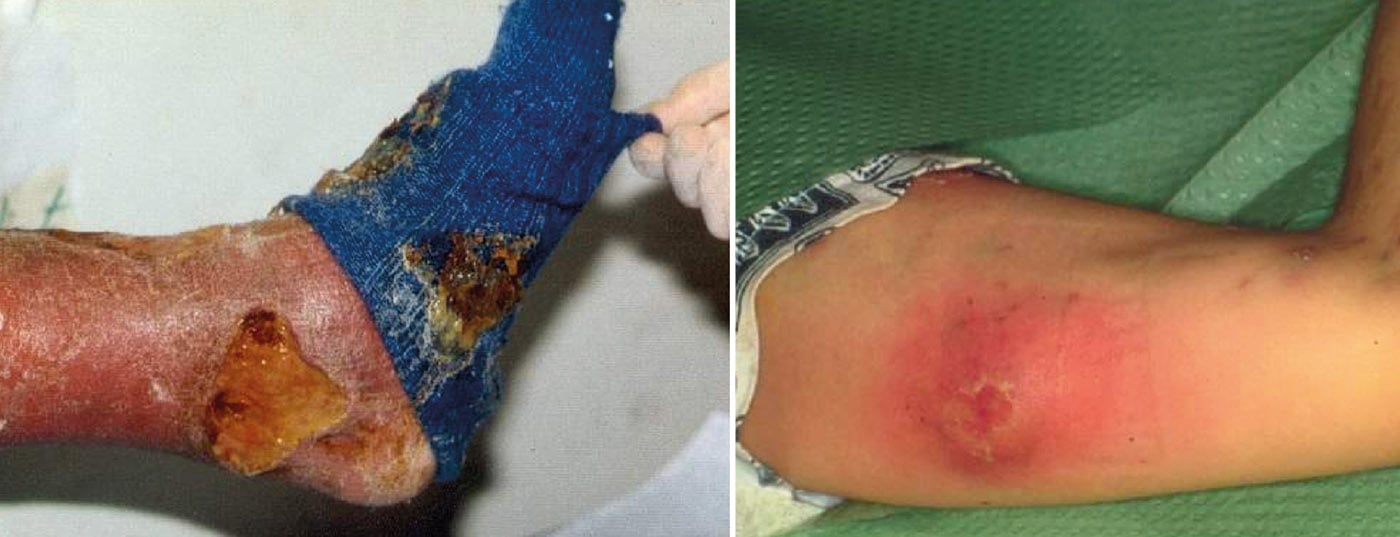
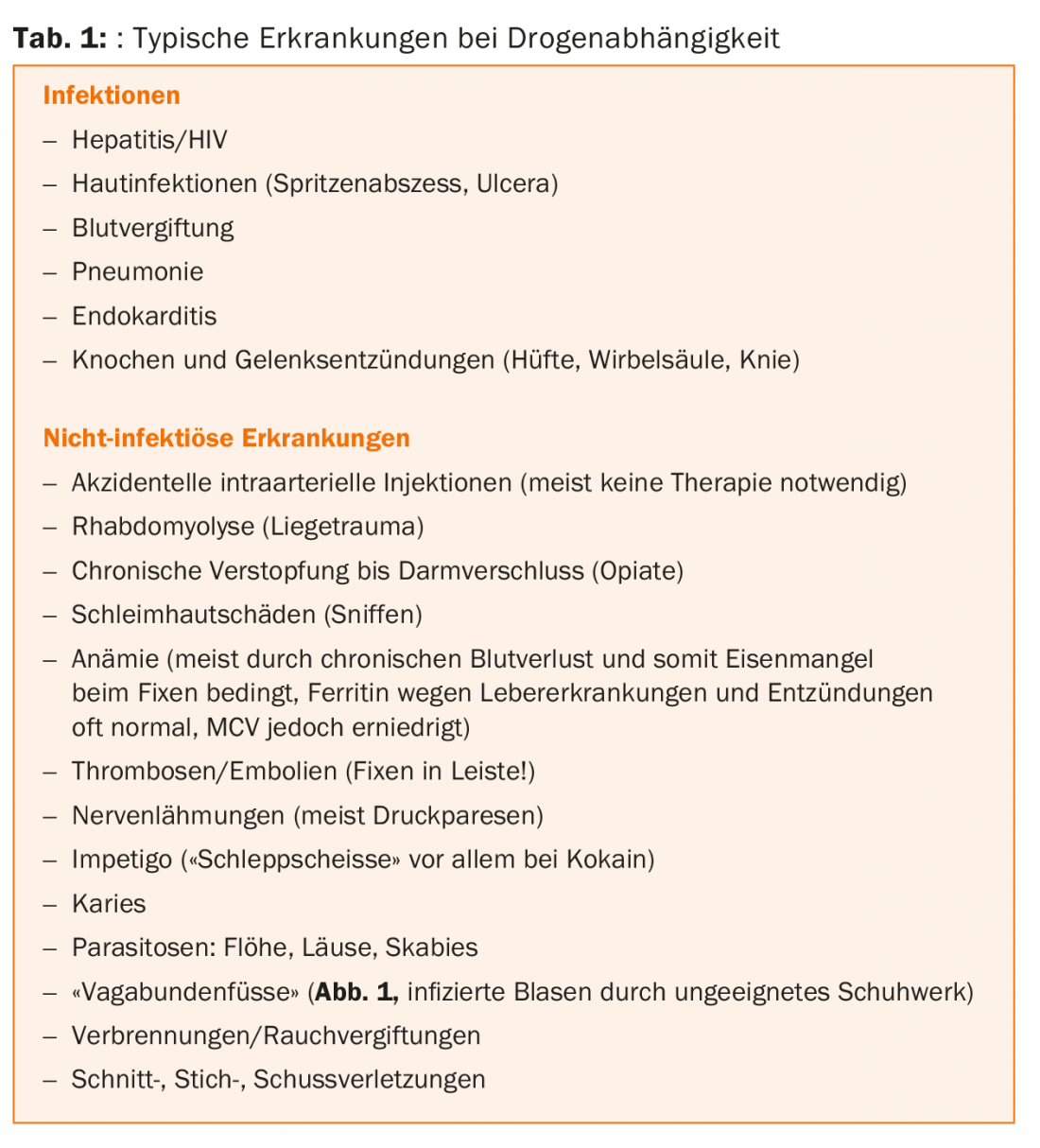
Syringe abscess
In the case of syringe abscess (Fig. 2) , the correct timing of the puncture incision is very important. Fluctuation should already be palpable, but the skin over it should not yet be so thinned that it later develops into an ulcer. Usually a small incision with insertion of a mèche after application of cold spray is sufficient. Prior administration of antibiotics (usually co-amoxicillin 2× 1 g) should be considered, especially in cases of fever and diffuse phlegmonous processes.
Endocarditis
Right ventricular endocarditis should be considered, especially in intravenous cocaine abuse. Reduced general condition, septic fever, elevated CRP/leukosis, and possible new-onset heart murmurs are suggestive. However, it is not uncommon for endocarditis to be discovered only by the appearance of septic metastases on chest x-ray. The risk for recurrence of endocarditis is very high with anamnestic endocarditis. Difficulty often arises with resistance-matched treatment over the time suggested by infectious disease specialists. Interactions with substitution (e.g. Rimactan® – methadone) should be watched for and the dose adjusted.
Osteomyelitis
Purulent septic gonarthritis usually offers no dia-gnostic difficulties due to the classic triad of Rubor- Dolor-Calor. Coxitis is already more discrete and groin pain is sometimes misleading. Typical is the axial shock pain when hitting the sole of the foot.
Spondylodiscitis (Fig. 3) often remains oligosymptomatic for a long time and is sometimes difficult to distinguish from lumbago. Chronic craving for pain medications, localized palpitation/pressure dolence, and elevated CRP are seminal.
Pneumonia
Pneumonia is quite common (chronic bronchitis, non-seasonal clothing, intoxicated lying around). Fever over 38 degrees as well as chest pain and poor general condition lead to the diagnosis. Often pneumonia can be treated on an outpatient basis or inpatient treatment is declined – e.g. because of pets. An x-ray can be helpful, of course, but is not always feasible for a variety of reasons. During antibiotic therapy – especially with azithromycin – attention should be paid to the QTc time, because this is often already greatly increased before the start of therapy (e.g., by methadone plus Quetiapin®).
Civilization diseases
Fortunately, with the average age of drug patients increasing sharply in recent decades, the prevalence of common “civilization diseases” has also increased sharply.
Weight gain with metabolic syndrome is common. Contributory causes are psychotropic drugs and lack of exercise. Due to the – almost obligatory – long-term tobacco use, COPD and, especially in heroin-dependent women due to heroin-induced amenorrhea, osteoporosis are often added. Following all drug and other recommendations of professional societies is hardly possible even in psychologically robust patients.
The main danger is drug polypragmasia, when a new drug is added for each new symptom that occurs (often drug side effects!). It is therefore important to identify and address the main risk factors and to check whether the patient is also able to take all the medications. Often, a “drug reset” with “drug holidays” is also useful in muddled situations.

Intoxications
Fortunately, with the widespread use of substitution therapies, the number of classic “drug deaths” from acute opiate intoxications has declined sharply in recent decades. Nevertheless, among fatal intoxications, acute opiate intoxication is still the most common. The period after opiate withdrawal is very critical in the absence of tolerance, which is why it is only recommended to be phased out very slowly, if at all. In this context, death in opiate relapse often comes insidiously in sleep.
Violence
Violence is unfortunately a common accompanying phenomenon with complex victim-perpetrator situations. Prosecution is often complicated by sociocultural and amnestic problems, e.g., midazolam abuse (Fig. 4).
InFo NEUROLOGY & PSYCHIATRY 2015, 13(5): 4-7.