At this year’s annual meeting of the Brain Stroke Society in Aarau, Prof. David Werring, UCL, Institute of Neurology, London (UK), provided information on cerebral amyloid angiopathy (CAA). This disease is by no means as rare as was previously thought, and as an important cause of dementia and cerebral hemorrhage, it also has great clinical and prognostic significance.
In cerebral amyloid angiopathy (CAA), β-amyloid is deposited in the walls of small to medium-sized cerebral capillaries and arteries (up to 2 mm in diameter). Amyloid deposits mainly affect cortical and leptomeningeal vessels, less frequently the cerebellum and basal ganglia. The deposits destroy the vessels and trigger endothelial dysfunction and microbleeding. Where the amyloid comes from is currently unknown, but failure of amyloid degradation is suspected.
The consequences of CAA: dementia, cerebral hemorrhages, focal deficits.
The prevalence of CAA is significantly lower in persons without dementia than in persons with dementia. This association between CAA and dementia and of CAA and cerebral hemorrhage has been recognized only in the last 20 years. Risk factors for CAA are primarily age, but also hypertension and genetic factors (ApoE, etc.). Typical signs of a CAA are as follows:
- Cerebral hemorrhages: Large lobar, not infrequently multiple cerebral hemorrhages as well as microhemorrhages are typical. Prof. Werring pointed out that in patients in whom microbleeds are detectable on imaging, the risk for cerebral hemorrhage is significantly greater than for ischemia.
- Transient focal neurologic episodes: These present similarly to a TIA, for example, paresthesia of the hand lasting a few minutes. 27-37% of patients with such an episode suffer a hemorrhagic stroke within the next two months.
- Dementia: This progresses more rapidly than classic Alzheimer’s dementia. On average, CAA patients require assistance with activities of daily living within one year of diagnosis. Imaging reveals typical white matter changes, micro- and/or macrobleeds, or ischemic infarcts.
- Inflammation: rapidly progressive encephalopathy with headache, seizures, and focal deficits. The MRI image is very typical: asymmetric white matter changes with mass effect.
High recurrence risk for cerebral hemorrhage
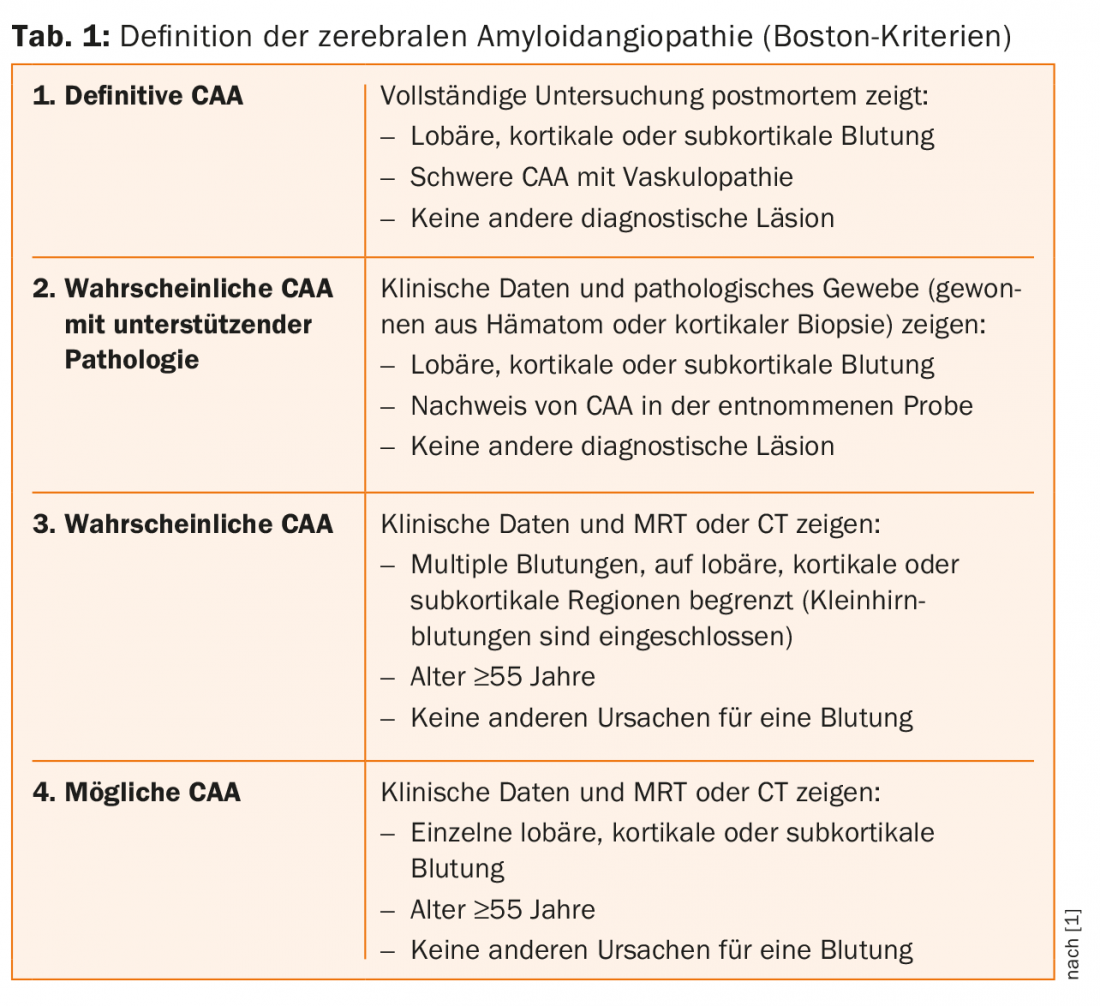
In the presence of CAA, the risk of recurrent cerebral hemorrhage is approximately 9%, and only 1% without CAA. This high risk is therefore an important component of the Boston criteria for the diagnosis of CAA-associated cerebral hemorrhage (Table 1) [1].
Superficial sideroses (CSS) secondary to small subarachnoid hemorrhages are also an important feature of CAA. CSS have prognostic significance: if CSS can be detected on imaging, the risk of recurrent cerebral hemorrhage is significantly greater. In one study, the risk of experiencing a new symptomatic cerebral hemorrhage within the next four years was 24% in patients without CSS and 75% in patients with CSS [2].
Lower blood pressure and avoid anticoagulants
For neurological practice, the importance of CAA is twofold: on the one hand, because of the increased risk of bleeding, e.g., during thrombolysis or prescription of antithrombotic drugs; on the other hand, because of the prevention of recurrent strokes. Because of the risk of bleeding, oral anticoagulants should not be prescribed in patients with CAA unless there is a very important indication. The only evidence-based measure for stroke prevention is blood pressure reduction. “However, at the moment it is still an open question how low blood pressure should or can be lowered,” the speaker noted. Statins should rather be avoided in CAA, but there are no controlled randomized trials on this (yet).
For the treatment of CAA, studies are currently underway with the monoclonal antibody ponezumab, which is directed against the amyloids. First results can hopefully be published this year.
Source: 19th Annual Meeting of the Swiss Brain Stroke Society, January 28, 2016, Aarau.
Literature:
- Knudsen KA, et al: Clinical diagnosis of cerebral amyloid angiopathy: validation of the Boston criteria. Neurology 2001; 56(4): 537-539.
- Charidimou A, et al: Cortical superficial siderosis and intracerebral hemorrhage risk in cerebral amyloid angiopathy. Neurology 2013; 81(19): 1666-1673.
InFo NEUROLOGY & PSYCHIATRY 2016; 14(2): 42-43.