Travel is often accompanied by skin problems that can present diagnostic challenges in the primary care physician’s office. People often take dermatological ailments home with them, especially from trips to the tropics, where the skin is exposed for long periods due to the hot climate and comes into contact with various invaders. This article gives an overview of some important disease patterns that can be caused by the sun, parasites, animals, bacteria, fungi, viruses, and toxins.
Table 1 lists a summary of various home-borne skin diseases. It comes from 50,000 travel patients in 31 centers and shows that one of the most common reasons for consultation was exanthema of undetermined etiology (sometimes associated with pruritus and/or urticaria). So, how can the diagnosis be made and what dermatological changes should be known in this area? A practical checklist is given below.

Fever/exanthema
Dengue fever, which is primarily transmitted by mosquitoes during the day, accounts for 45% of febrile exanthemic illnesses. The disease presents with fever, malaise, retrobulbar headache, and severe musculoskeletal pain after an incubation period of two to eight days. A fine morbilliform exanthema is found on the trunk and face during the first two days. It intensifies over the next three to six days and then flakes off. Diagnosis can be made with the dengue IgM.
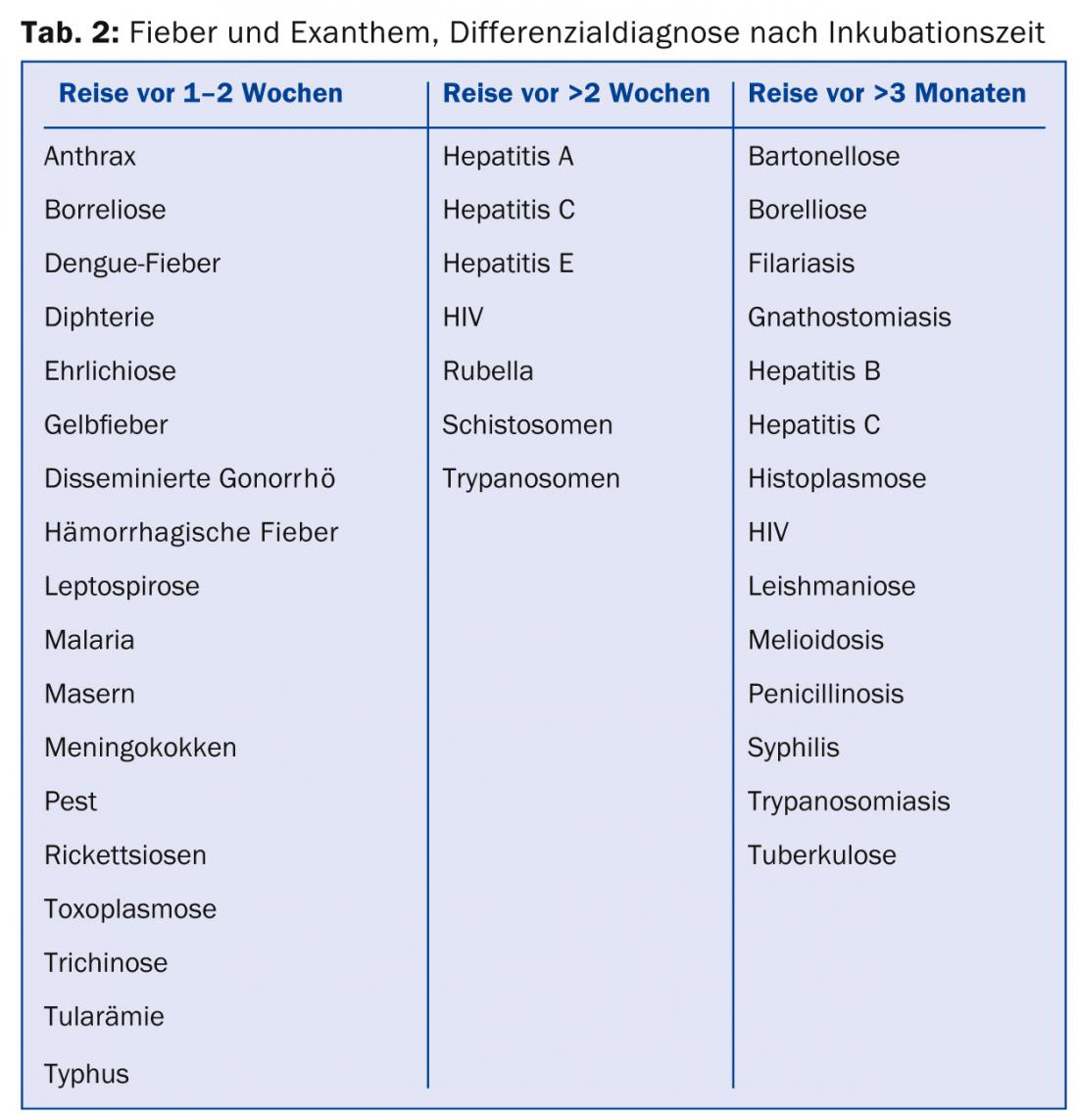
The differential diagnosis of exanthema and fever can be narrowed down by means of the time since the return journey (Tab. 2). Because several of the diagnoses in question can be lethal (e.g., meningitis, viral hemorrhagic fever, and disseminated gonorrhea), diagnostic tests should be performed promptly and tropical medicine-trained physicians should be consulted quickly for nonspecific cases. This means that dangerous diseases such as malaria are less likely to be missed.
Sun-related dermatoses
Dermatitis solaris, colloquially known as sunburn, is the most common skin condition during tropical travel. Especially during the first days of vacation, the danger is great and direct exposure to the sun (especially during the midday hours) should be avoided in any case. Even today’s sunscreens cannot prevent sunburn in many cases, but only delay it. Textiles with built-in UV protection are more efficient. For young children, sun protection measures (staying in the shade, sunblock, possibly UV-proof textiles) must be strictly adhered to.
Also common is the so-called polymorphous light dermatosis. It occurs predominantly with first-time sudden exposure to high amounts of UV and can manifest itself very differently with various efflorescences, but is usually relatively monomorphic in the individual patient. Prevention may be possible with prior “hardening” in UVA/UVB phototherapy (offered by dermatologists).
Infections of the skin
The most common rice diseases include bacterial infections of the skin (primarily insect bites, which can be superinfected by scratching and the mixed flora present). In some cases, complications such as ecthyma (flat purulent ulcers that look like they have been punched out) are also present, Fig. 1) possible.

Therefore, the following basic rule applies: Every ulceration after a stay in the tropics should be considered to be caused by a bacterial (mixed) infection (bacteriological smears are mandatory and antibiotic shielding is often indicated at an early stage). If left untreated and undetected, such infections can cause extensive ulceration and local tissue destruction, sometimes with a fulminant course. Impetiginization of pre-existing dermatoses is also often found. It is therefore essential to disinfect consistently. Impetigo in the tropics is very often bullous and rather rarely honey-crusted as in Switzerland.
Fungal infections occur more frequently in the tropics than in this country due to the warm, humid climate. Mycoses, which develop for example in the intertriginous area, are caused in our latitudes mainly by dermatophytes, in the tropics yeasts and molds are often also responsible. Therefore, a mycological culture should always be performed. Only in this way can a targeted pathogen-specific antifungal therapy be initiated. In these countries, fungal infections also occur in deeper skin layers (e.g. mycetoma, chromoblastomycosis). Compared to the local population, such infections are rare (due to the usually better hygienic conditions and the shorter stay of tourists). Nevertheless, in cases of unclear partly exophytic skin tumors, this mycologic cause should be considered and appropriate cultures and tissue biopsies should be performed.
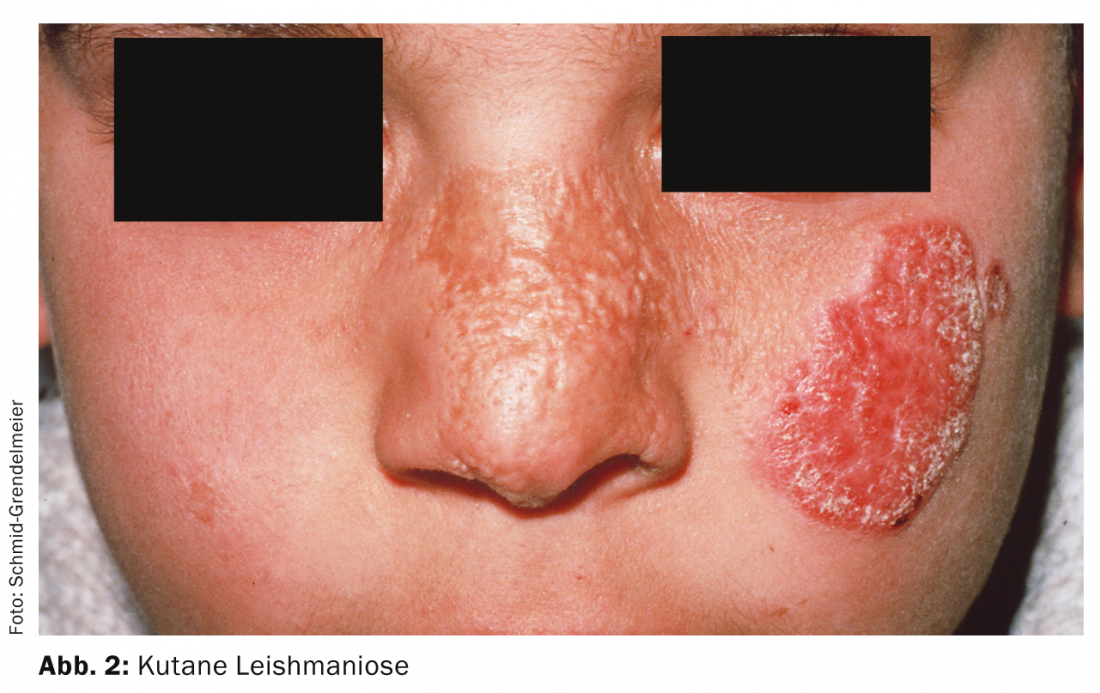
Cutaneous leishmaniasis (Fig. 2) is characterized by single or multiple ulcerations or papular changes, especially on the extremities or face. In the case of a non-healing ulcer, leishmaniasis should be considered in addition to bacterial causes after a stay in the tropics . Biopsy and PCR diagnostics consolidate the diagnosis. Many leishmaniasis lesions heal on their own, but due to possible scarring, treatment (in consultation with a doctor trained in tropical medicine) is usually advisable.
The diagnosis of leprosy (paucibacillary form), although very rare in our country, should nevertheless be considered in patients who have spent prolonged periods in the tropics in hyperpigmented areas with hypaesthesia. Diagnosis can be made by histology (including Ziehl-Nehlsen or Fite-Faraco staining) and PCR.
Epizoonoses
After close physical contact with the local population, scabies (itch mite) may appear in returnees. This is almost endemic in many travel countries, especially among the rural population. Scabies skin lesions develop three to four weeks after physical contact with a person already suffering from scabies. Indications are papular, intensely pruritic changes, especially in the genital area as well as the interdigital spaces. Diagnosis is confirmed by scraping the ink-filled duct onto a microscope slide and microscopically identifying the eggs and mites. Infants often experience palmo-plantar involvement. Especially in case of pustules in this area, scabies should therefore be considered in this age group.
Humans are actually a false host of larva migrans, which is caused by larvae of parasites. Worm larvae deposited in the sand or soil penetrate through the skin. Serbiginous, sometimes pustular skin changes are therefore mainly found plantar and after bathing trips (walking barefoot). In principle, larva migrans usually heals itself after a few days to weeks, but can be additionally accelerated with medication.
Tungiasis is also localized on the feet in the form of wart-like skin lesions with a central opening. It is caused by burrowing of the tunga flea between the toes (egg laying) and can be caused by superinfection resp. secondary eczematization lead to complications. Sterile peeling of the eggs is essential.
In myiasis, the skin or open wounds are invaded by fly larvae. The changes are furunculoid, with the larvae usually visible and palpable. After one to two days, the larvae emerge to the surface, provided that occlusion with oil is performed. The larvae must then be extracted and preserved in alcohol for analysis.
Bites, stings and poison
Without antibiotic prophylaxis, dog bites become infected in about 2% of cases. In cat and human bites, the risk is significantly higher (in 15 -16%). It is imperative to clarify the tetanus vaccination status and the possibility of rabies exposure, which must result in re-immunization with passive and active vaccination.
The tropics harbor significantly more venomous animals than the more northern latitudes. Such contacts are possible both in the water and on land. In the water, jellyfish in particular often cause very painful skin lesions (urticarial, vesicular or even necrotic-toxic depending on the source species). Individual jellyfish species, such as the cube jellyfish (Chironex, can trigger life-threatening reactions through toxins. Rays cause very painful, secondary mostly ulcerative reactions, some of which heal very poorly and not infrequently even require surgical debridement. Stings and bites from scorpions, spiders and a wide variety of insects are a problem, especially on land.
Hymenoptera (bee, wasps) cause allergic reactions, while otherwise mainly toxic reactions are common. For insect venom allergy sufferers, an emergency kit (contains steroid tablets and antihistamines, and for severe reactions, epinephrine auto-injectors, such as EpiPen® or JEXT®) is recommended in travel luggage. If necessary, a specific immunotherapy can also be clarified. Certain beetles (e.g. of the family Meloidae and the species Päderus) or caterpillars cause toxic reactions with redness and blisters (“beetle dermatitis”) even at mere skin contact. This is because they deliver the appropriate toxins (such as cantharidin or paedin) directly through their hairs or chitin shell. Therefore, the skin should be washed with water directly after such contacts.
In principle, the morphology of insect bites is typical (erythematous papule with a centrally hemorrhagic sting). Grouping also has an important meaning:
- Bug bites typically occur on unclothed skin, and as linear groups of three (“breakfast, lunch and dinner sign”).
- Flea bites are located on covered areas of the body and are multiple, usually grouped together.
The tsetse fly is a carrier of trypanosomes (sleeping sickness). It measures about 1 cm and is extremely resistant. Its painful sting also passes through clothing (jeans) and causes a broad (2 cm), indurated papule with, at most, regional lymphadenopathy.
Finally, Table 3 lists various traveler’s dermatoses on a situational basis.

CONCLUSION FOR PRACTICE
- Dermatoses from the tropics are often due to infections. Microbiological examinations are therefore always indicated.
- In cases of unclear lesions, a skin biopsy may provide further useful information.
- In case of fever with exanthema and at most eosinophilia, a tropical medical examination should be performed.
- Good sun protection is important to prevent sunburn and other photodermatoses.
A RETENIR
- Les dermatoses tropicales sont souvent provoquées par des infections. Les analyses microbiologiques sont donc toujours indiquées.
- En cas de lésions douteuses, une biopsie cutanée peut apporter d’autres informations utiles.
- Un examen de médecine tropicale est indispensable en cas de fièvre accompagnée d’exanthème et éventuellement d’éosinophilie.
- Une protection solaire adéquate est importante pour prévenir les coups de soleil et autres photodermatoses.
HAUSARZT PRAXIS 2014; 9(6): 20-23











