Coronary CT allows direct visualization and assessment of the coronaries after i.v. contrast administration and can exclude CAD in symptomatic patients with high negative predictive value. It takes little time and can be performed with a very low dose of radiation. In the future, coronary CT will certainly become even more important.
Various noninvasive cardiac imaging modalities are available for diagnostic workup of possible coronary artery disease (CAD). In addition to functional tests such as stress echocardiography, stress magnetic resonance imaging (MRI), or nuclear cardiological methods (myocardial single-photon emission computed tomography [SPECT]; myocardial positron emission tomography [PET], [1]), coronary computed tomography (CT) as an anatomic noninvasive examination is an established method in clinical routine [2]. Coronary CT allows direct visualization and assessment of the coronaries after intravenous contrast administration and can exclude CAD in symptomatic patients with high negative predictive value. The examination takes little time and, thanks to advances in recent decades, can be performed with a very low dose of radiation. In asymptomatic patients, calcium score (based on native cardiac CT without administration of contrast) is an important tool for risk stratification.
Coronary CT for clarification of CHD in symptomatic patients.
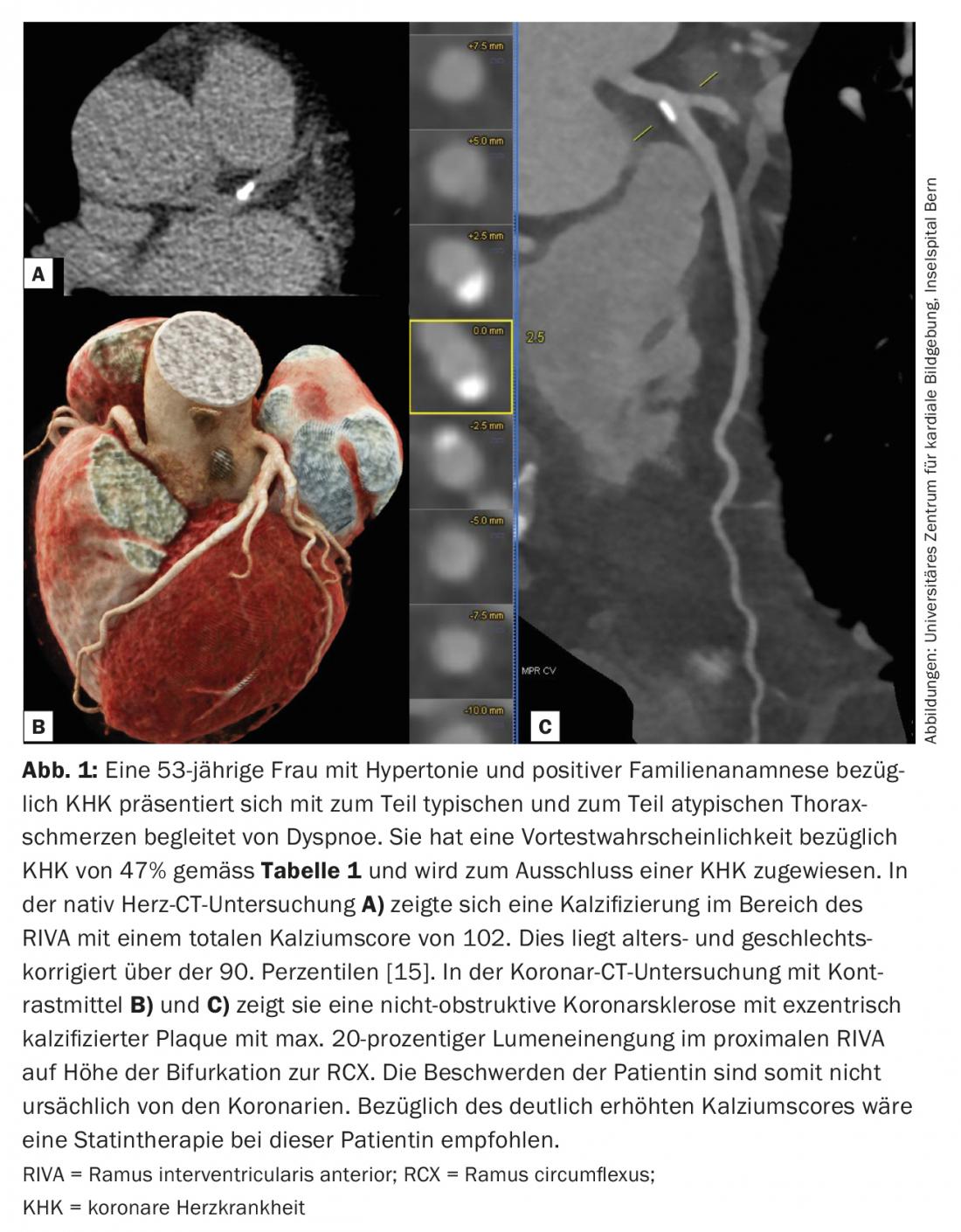
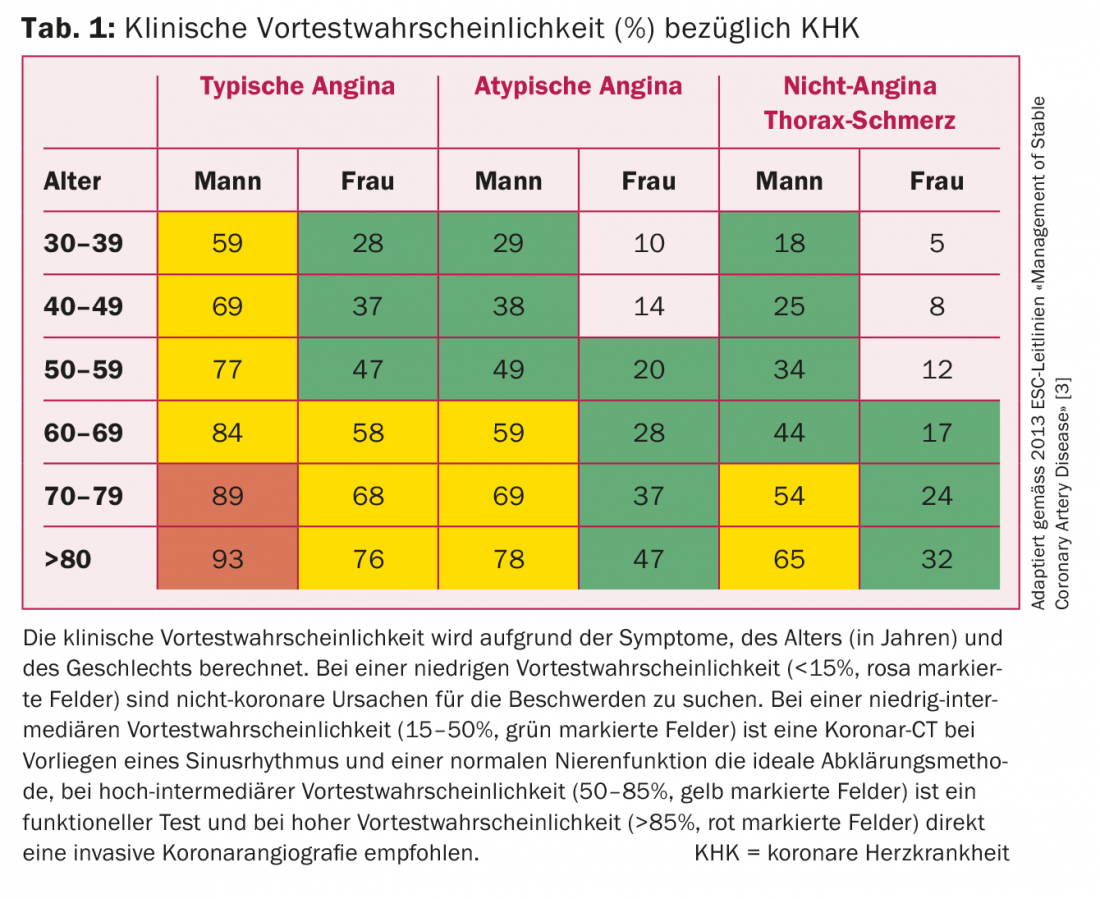
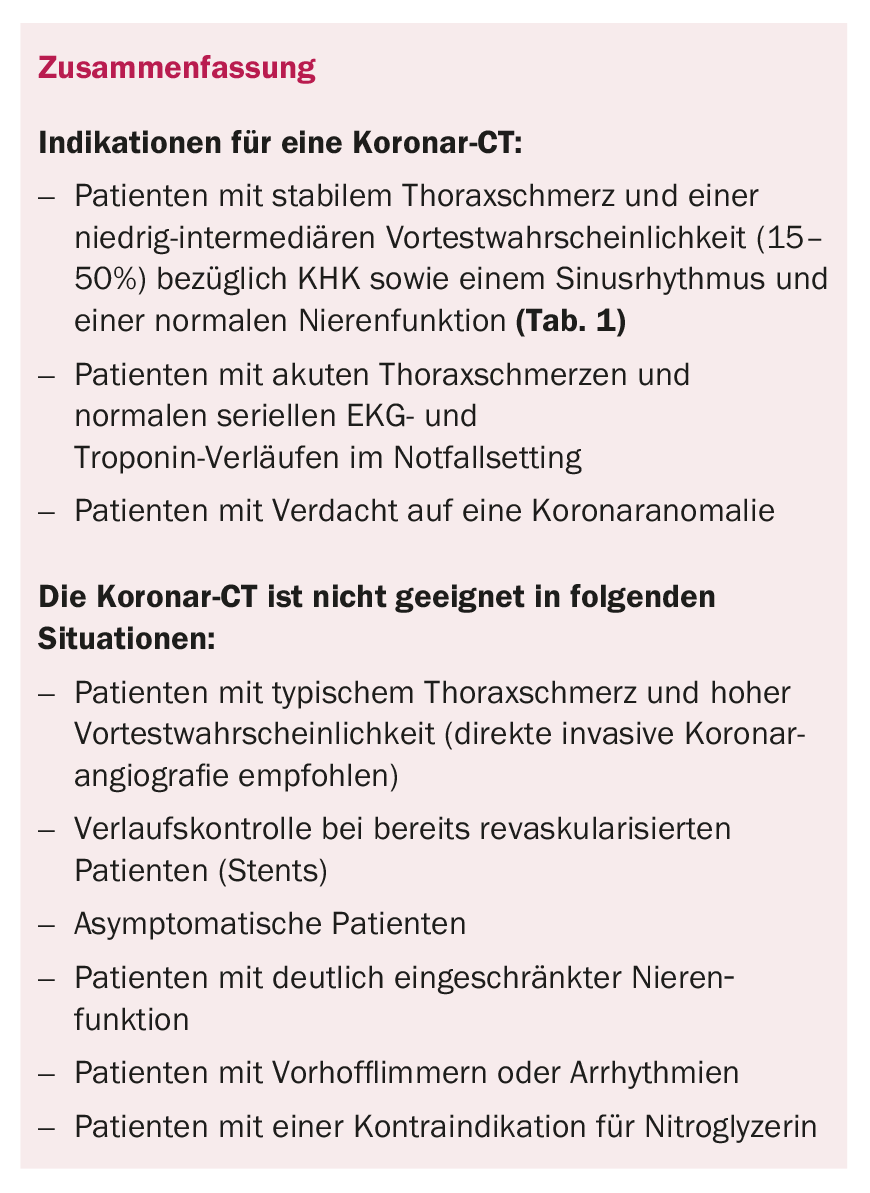
Coronary CT, with contrast of the coronary vessels, is indicated in symptomatic patients with low-intermediate pretest probability (15-50% pretest probability regarding CHD) as well as sinus rhythm and normal renal function (Fig. 1). The pretest probability can be calculated based on the patient’s symptoms, age, and gender (Table 1) [3]. According to current studies, coronary CT is considered useful in the above-mentioned patient group, which is a IIa indication according to the ESC guidelines “Management of Stable Coronary Artery Disease” published in 2013. Furthermore, in patients with nonconclusive ergometry or in patients with a contraindication regarding a stress test, coronary CT is an ideal examination method (also class IIa indication) [3]. The NICE (National Institute for Health and Care Excellences) guidelines from England go even further and recommend coronary CT as the initial test for all chest pain. The aim is to ensure that invasive coronary angiography is not used primarily for diagnostic purposes, but only in patients with a high probability of intervention. In contrast, the European guidelines recommend performing a functional test if the pretest probability is high intermediate (50-85%) and directly invasive coronary angiography if the pretest probability is high (>85%) [3]. Coronary CT has very high sensitivity (95-99%) and intermediate specificity (64-83%) with respect to obstructive coronaryopathy (≥50% stenosis), resulting in a high negative predictive value, and thus is primarily used to exclude CAD (Fig. 2) [3]. In addition to patients with stable chest pain, coronary CT also has value in patients with acute chest pain. If a patient presents with acute typical chest pain but initially with a normal ECG and negative cardiac enzymes, the likelihood of acute coronary syndrome is low. However, the consequences of missing the diagnosis are devastating. For this reason, these patients are followed up with serial ECGs and cardiac enzyme testing. If these follow-up controls remain normal in the emergency department, further investigation is often performed by means of ergometry. However, ergometry has a very low sensitivity (approximately 50%) and thus coronary CT is an ideal method to rule out CAD even in these patients with acute chest pain.
Thanks to constant technological progress and the latest computer tomographs (“scanners”), the method has not only become faster and more accurate, but it has been possible to reduce the radiation exposure from 25 mSv to currently about 1 mSv in routine clinical practice [4]. This corresponds to a significantly lower radiation dose compared to SPECT, PET, or diagnostic invasive coronary angiography.
When a stenosis of 50% or more is detected by coronary CT, patients should undergo subsequent functional stress testing (SPECT, PET, stress echo, or MRI) to clarify the hemodynamic relevance of the stenosis. If invasive coronary angiography is preferred for further evaluation, fractional flow reserve (FFR) can also be used to assess hemodynamic relevance.
In addition to the advantages of coronary CT with noninvasive anatomic imaging of vessels, rapid feasibility, and cost-effectiveness, the method allows plaque characterization (calcified plaques, soft plaques, mixed plaques). This information also helps in non-obstructive CAD (<50% stenosis) for further treatment decision [5]. Intensified statin therapy is particularly recommended in the presence of so-called “vulnerable” plaques (soft plaques or mixed plaques with soft and calcified portions).
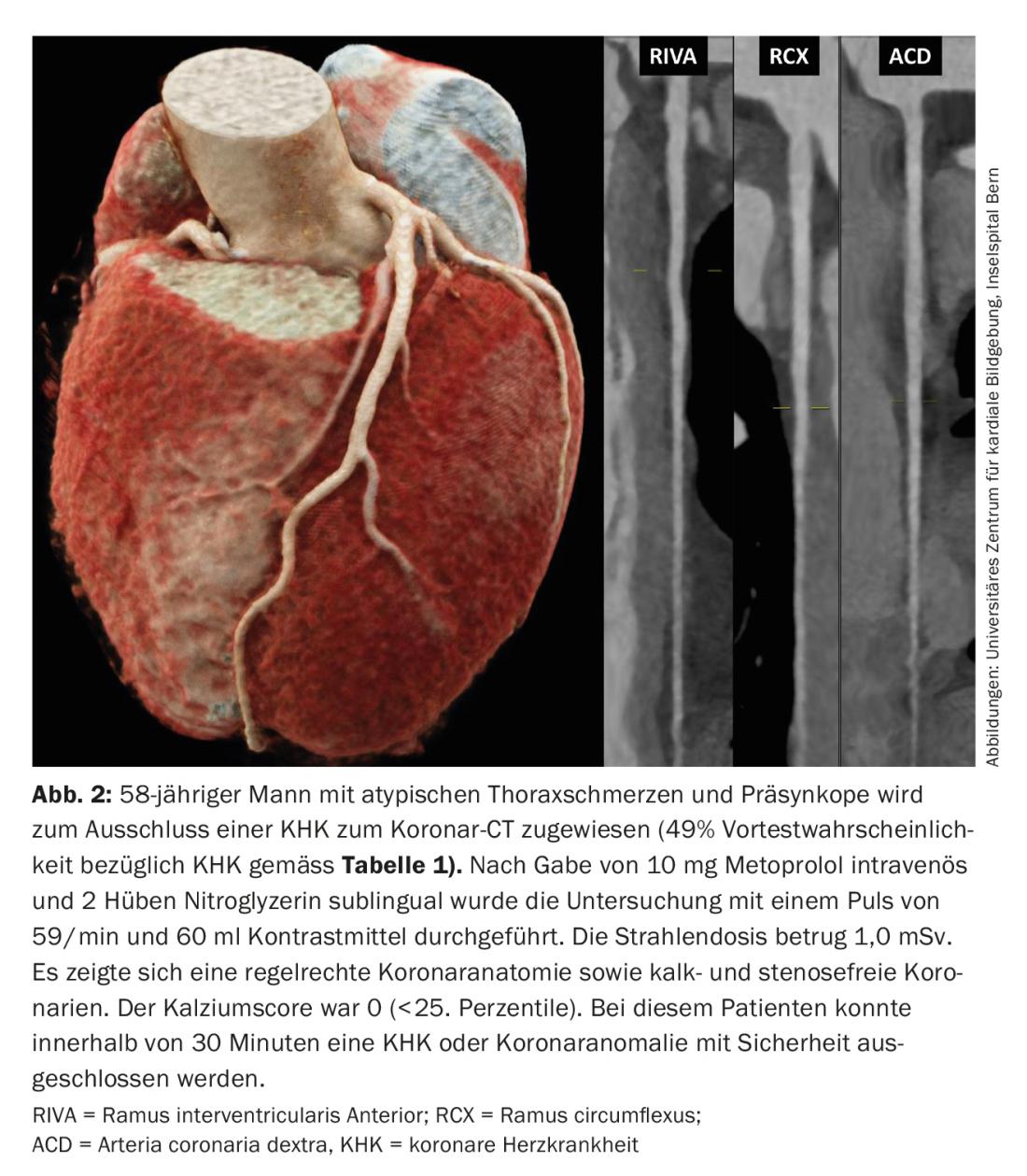
Procedure of the examination: In terms of procedure, the coronary CT examination is relatively simple. Since a low heart rate significantly improves image quality and thus the radiation dose can be kept low, a beta blocker is administered either orally (about 1 hr before the examination) or intravenously (directly before the examination). Nitroglycerin (usually two strokes sublingually) is used for coronary dilatation. The lying time in the scanner is about 10-15 min and several short breath-holding maneuvers (10-15 sec each) are necessary. A total of between 30-90 ml of contrast medium is administered i.v.. Patients should be urged to discontinue potency-enhancing agents such as sildenafil, tadalafil, or vardenafil before the study because of possible hypotension from nitroglycerin administration. To plan the coronary CT scan with contrast, a native cardiac CT is performed beforehand, which additionally allows the information regarding the calcium score.
Limitations: Limitations include the need for higher radiation doses at higher heart rates that cannot be lowered with beta blockers (>70 beats per minute). Arrhythmias (atrial fibrillation, extrasystoles, bigeminy) may cause motion artifacts of the coronary vessels and significantly limit the assessment. In patients with status post revascularization (stents), perfusion of the stents can be assessed, but assessment of the degrees of stenosis within the stents is difficult. Because vasodilation of the coronary vessels is essential as a preparatory step, patients with a contraindication to nitroglycerin (e.g., severe aortic valve stenosis) are not appropriate patients for coronary CT.
Risk stratification with els calcium score of asymptomatic patients
In contrast to symptomatic patients, coronary CT is not recommended in asymptomatic patients according to ESC guidelines (class III) [3]. In contrast, the calcium score, which can be calculated on native cardiac CT (without contrast), is an ideal tool for risk stratification in asymptomatic patients [6,7]. The calcium score is clearly superior to the intima-media thickness measurement, ankle-brachial index, high-sensitivity C-reactive protein, or Framingham risk score in terms of predictive power of a cardiovascular event or mortality [7,8] and is certainly warranted in selected patients. It is a decision aid in patients with a cardiovascular risk profile that is difficult to assess clinically (for example, in patients with a high family burden but normal cholesterol levels, or in patients with elevated cholesterol levels but few risk factors, or in patients who are statin intolerant and want to be sure that a statin is indeed indicated). Advantages are the non-invasive clarification, i.e. neither blood sampling nor needle puncture are necessary, high availability, low radiation dose and cost efficiency [9]. For these reasons, the American guidelines (ACCF/AHA) recommend the determination of a calcium score in patients at intermediate risk (i.e., 10-year risk of myocardial infarction between 10 and 20%) for possible reclassification and possible concomitant modification of the therapeutic regimen [10]. The NCEP-ATP III (National Cholesterol Education Programme Adult Treatment Panel III) guidelines recommend establishing intensified statin therapy in patients with multiple risk factors and a calcium score above the 75th percentile (according to age and sex).
In symptomatic patients, calcium score alone is not the appropriate test because the degree of stenosis of calcified plaques cannot be assessed and possible stenosing soft plaques may also be missed. Therefore, an additional coronary CT scan with contrast should always be performed in symptomatic patients in addition to the calcium score [11].
Other applications of coronary CT and its future prospects.
In addition to ruling out CAD, coronary CT is the ideal modality to visualize a coronary anomaly [12]. Coronary CT provides important information about the high-risk anatomy (origin, course, and termination of the coronary anomaly) and thus can distinguish “malignant” (interarterial course of the anomalous vessel between the aorta and the truncus pulmonalis) from “benign” anomalies with high resolution [12,13].
Coronary CT will certainly become more important in the future. Recently published data show that one can noninvasively simulate FFR on CT (similar to invasive coronary angiography) by complex postprocessing of the image material [14]. This would allow, without further investigation, to determine the hemodynamic relevance of each plaque. Furthermore, research is currently underway that quantifies the perfusion behavior of the contrast agent in the myocardium by means of dynamic perfusion measurement during sequential recordings of the myocardium under adenosine stress. This method can detect a hemodynamically relevant stenosis. Thus, a “one-stop store” with visualization of anatomy and simultaneous assessment of myocardial perfusion would be possible.
Take-Home Messages
- Coronary CT is an established method to exclude CAD in symptomatic patients with low-intermediate pretest probability (15-50%) regarding CAD as well as sinus rhythm and normal renal function.
- Coronary CT is performed quickly, is cost-effective, and can be performed with a low radiation dose.
- Coronary CT is an ideal method for evaluating coronary abnormalities.
- The calcium score helps to stratify risk in selected asymptomatic patients with difficult-to-estimate cardiovascular risk profiles.
Literature:
- Acampa W, et al: Role of risk stratification by SPECT, PET, and hybrid imaging in guiding management of stable patients with ischaemic heart disease: expert panel of the EANM cardiovascular committee and EACVI. Eur Heart J Cardiovasc Imaging 2015; 16(12): 1289-1298.
- Clerc OF, et al: Long-term prognostic performance of low-dose coronary computed tomography angiography with prospective electrocardiogram triggering. Eur Radiol 2017; 27(11): 4650-4660.
- Montalescot G, et al: 2013 ESC guidelines on the management of stable coronary artery disease: the Task Force on the management of stable coronary artery disease of the European Society of Cardiology. Eur Heart J 2013; 34(38): 2949-3003.
- Benz DC, et al: Minimized Radiation and Contrast Agent Exposure for Coronary Computed Tomography Angiography: First Clinical Experience on a Latest Generation 256-slice Scanner. Acad Radiol 2016; 23(8): 1008-1014.
- Motoyama S, et al: Plaque Characterization by Coronary Computed Tomography Angiography and the Likelihood of Acute Coronary Events in Mid-Term Follow-Up. J Am Coll Cardiol 2015; 66(4): 337-346.
- Shaw LJ, et al: Prognostic value of cardiac risk factors and coronary artery calcium screening for all-cause mortality. Radiology 2003; 228(3): 826-833.
- Budoff MJ, et al: Long-term prognosis associated with coronary calcification: observations from a registry of 25,253 patients. J Am Coll Cardiol 2007; 49(18): 1860-1870.
- Yeboah J, et al: Utility of Nontraditional Risk Markers in Atherosclerotic Cardiovascular Disease Risk Assessment. J Am Coll Cardiol 2016; 67(2): 139-147.
- van Kempen BJ, et al: Comparative effectiveness and cost-effectiveness of computed tomography screening for coronary artery calcium in asymptomatic individuals. J Am Coll Cardiol 2011; 58(16): 1690-1701.
- Greenland P, et al:. 2010 ACCF/AHA guideline for assessment of cardiovascular risk in asymptomatic adults: executive summary: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation 2010; 122(25): 2748-2764.
- Al-Mallah MH, et al: Does coronary CT angiography improve risk stratification over coronary calcium scoring in symptomatic patients with suspected coronary artery disease? Results from the prospective multicenter international CONFIRM registry. Eur Heart J Cardiovasc Imaging 2014; 15(3): 267-274.
- Gräni C, et al: Multimodality Imaging in Individuals With Anomalous Coronary Arteries. JACC Cardiovasc Imaging 2017; 10(4): 471-481.
- Gräni C, et al: Outcome in middle-aged individuals with anomalous origin of the coronary artery from the opposite sinus: a matched cohort study. Eur Heart J 2017; 38(25): 2009-2016.
- Douglas PS, et al: Clinical outcomes of fractional flow reserve by computed tomographic angiography-guided diagnostic strategies vs. usual care in patients with suspected coronary artery disease: the prospective longitudinal trial of FFR(CT): outcome and resource impacts study. Eur Heart J 2015; 36(47): 3359-3367.
- Hoff JA, et al: Age and gender distributions of coronary artery calcium detected by electron beam tomography in 35,246 adults. Am J Cardiol 2001; 87(12): 1335-1339.
CARDIOVASC 2018; 17(2): 10-14