Joint diagnostics can be covered radiologically with various procedures. In most cases, a reliable diagnosis is also possible.
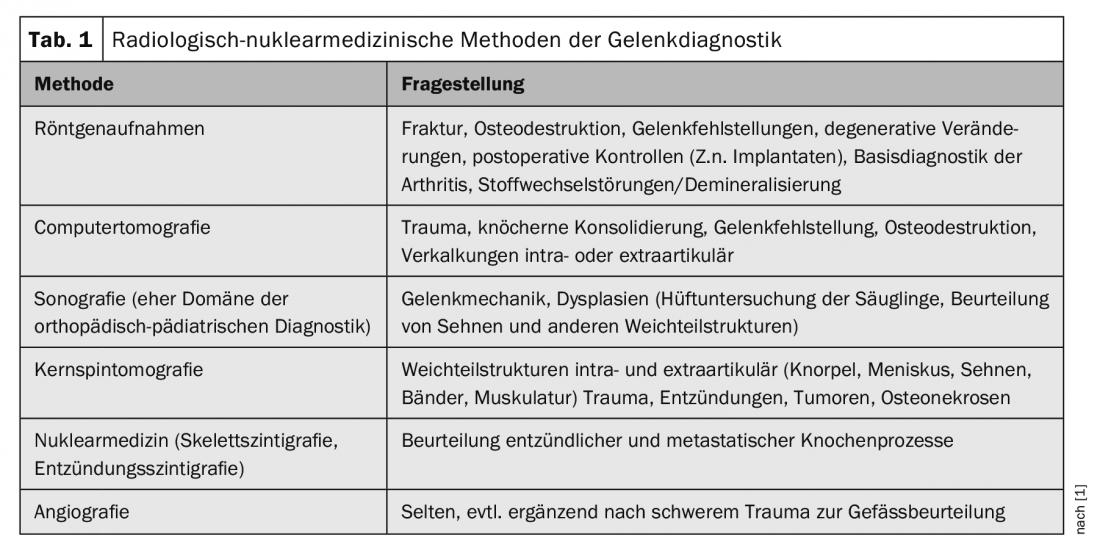
The prerequisite for the selection of the appropriate radiological-nuclear medical procedure is information from the referrer about the existing symptoms, accident mechanism, relevant metabolic diseases (e.g., gout, diabetes mellitus, vitamin changes, hormone disorders), laboratory findings in the case of suspected inflammatory joint changes, previous operations, or genetic diseases. Table 1 shows which diagnostic methods can be used depending on the problem.
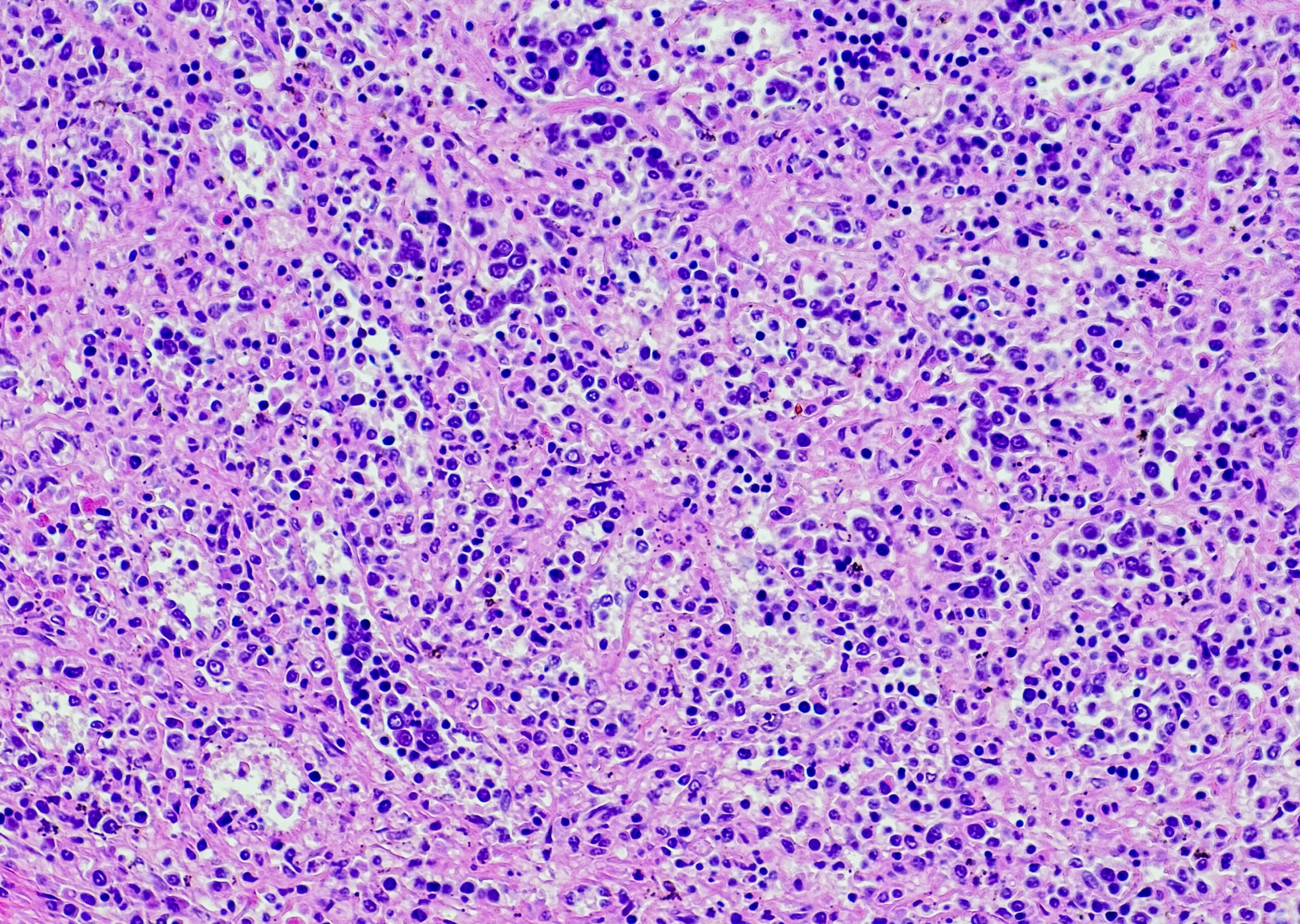
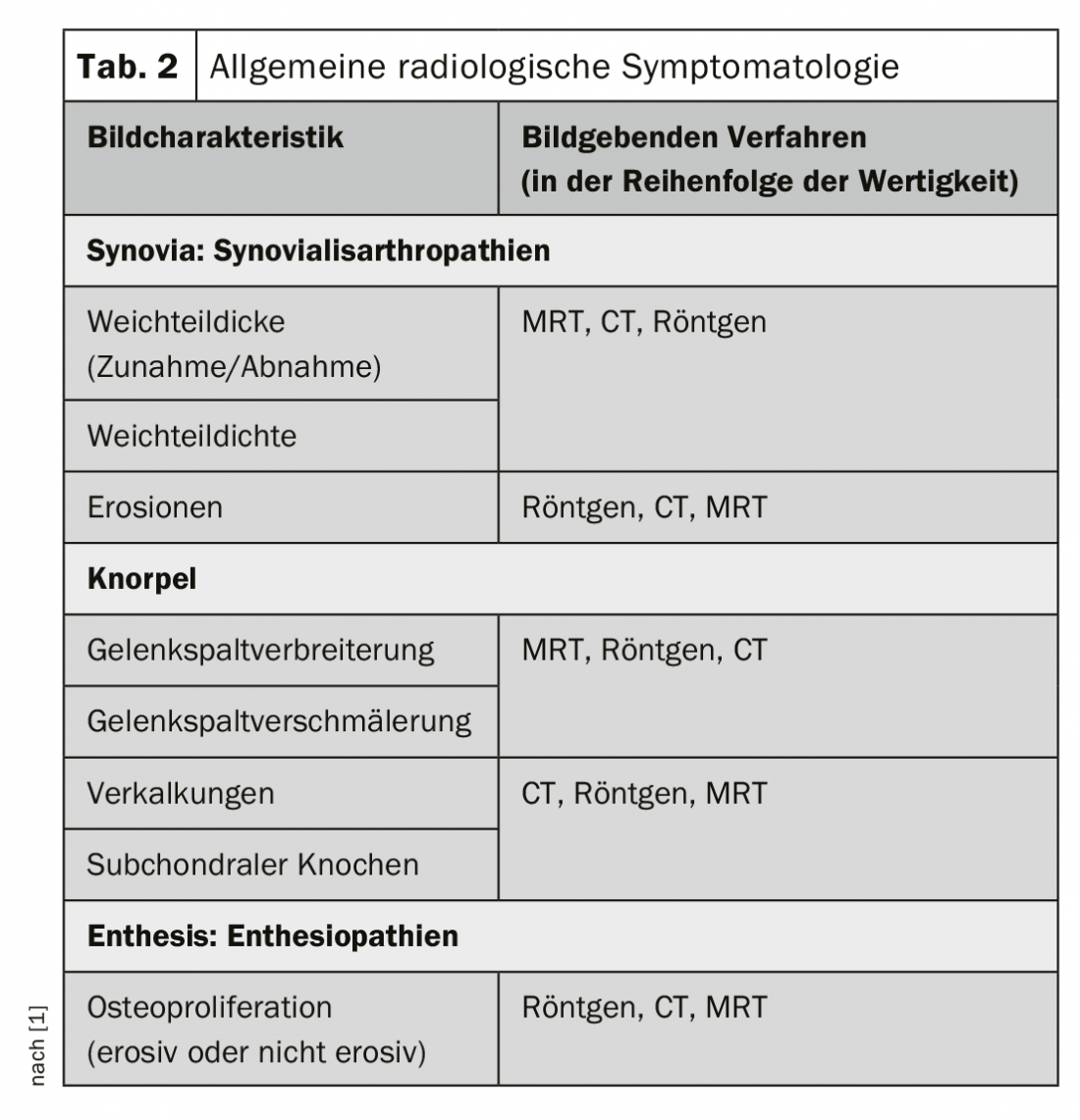
Many joint problems can already be detected by X-rays in two planes. Knowing the symptomatology and paraclinical findings, the general radiological symptomatology can be assigned to the three basic structures of the joints (Table 2) [1].
Sonography and magnetic resonance imaging more sensitive than projection radiography
Inflammatory-degenerative changes can often already be assigned diagnostically by systematic analysis of radiographic findings and knowledge of the symptomatology and laboratory value constellation, if required. However, it is also important to know that sonography and magnetic resonance imaging, for example, detect pathological processes of the joints earlier and more sensitively than projection radiography, and that radiographically negative findings, especially in the presence of an appropriate clinical and paraclinical constellation, do not exclude early disease occurrence and also provide little information about disease activity and concomitant soft tissue pathology in the course [2]. It is the radiologist’s responsibility to point out this special situation and the possibility or the need for target-oriented imaging diagnostics and differential diagnostics.
Avoid overdiagnosis
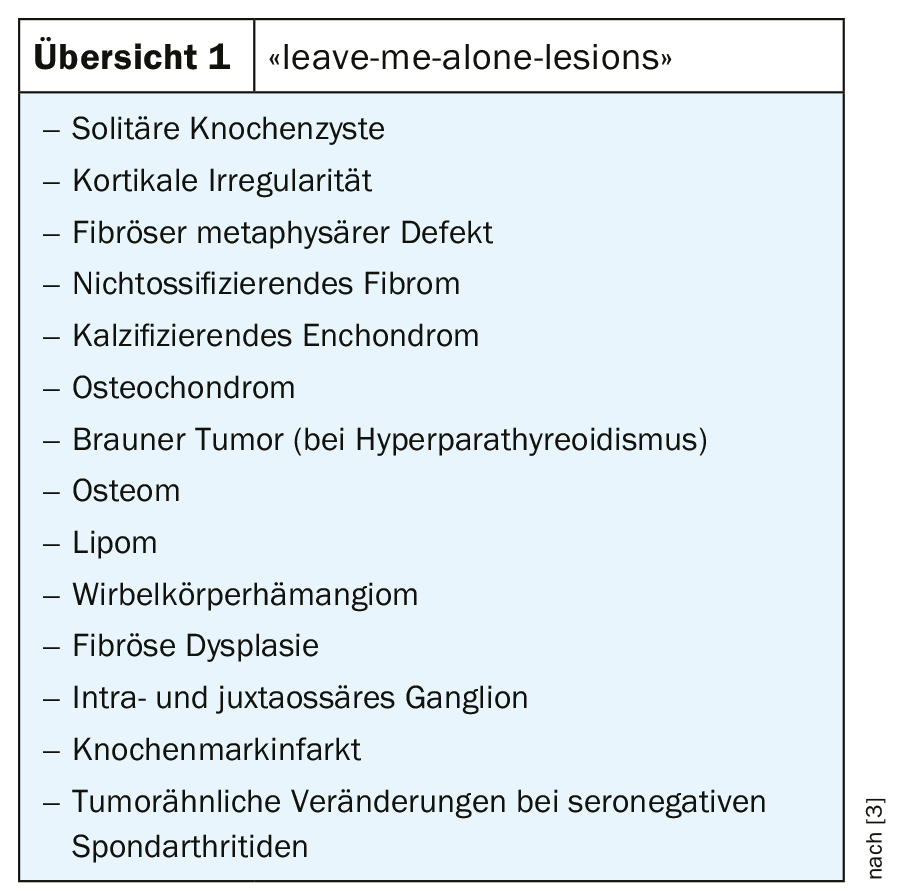
On the other hand, effective radiological diagnostics must also provide the treating colleagues as well as patients with the certainty of the diagnosis and avoid overdiagnosis or overtherapy in certain cases, the “leave me alone lesions” of the bone and joints close to the joints (also called “don’t touch me lesions”). These are reactive, sometimes still physiologic or benign tumorous changes whose image morphology is usually so clear that a diagnosis can be made with certainty in the overall aspect of the anamnestic, clinical, and paraclinical data (review 1) [3].
Advantages and disadvantages of magnetic resonance imaging
Magnetic resonance imaging presents the internal structures of the joints and also paraarticular tissues in an incomparable way like no other imaging procedure. Pathologic changes such as edema, hemorrhage, or inflammation are safely visualized, as is ligamentous, cartilaginous, and meniscal damage. Advantages include high soft tissue contrast, multiplanar visualization of pathologic processes, and lack of radiation exposure [4]. The major disadvantage of the method is the susceptibility to artifacts with implanted joint prostheses or other metallic material in the examination area. Even postoperative conditions can lead to limited assessability of the joint region if microscopic metal debris is present.
Scintigraphy has become less important, except in oncologic patients with the question of skeletal metastasis. Multiphase skeletal scintigraphy, which used to be performed when arthritis was suspected, no longer occurs in practice.
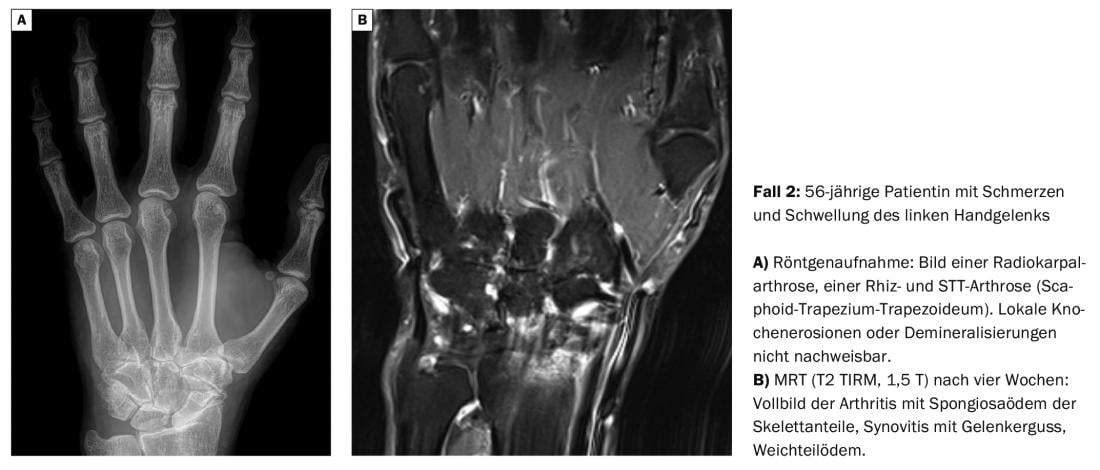
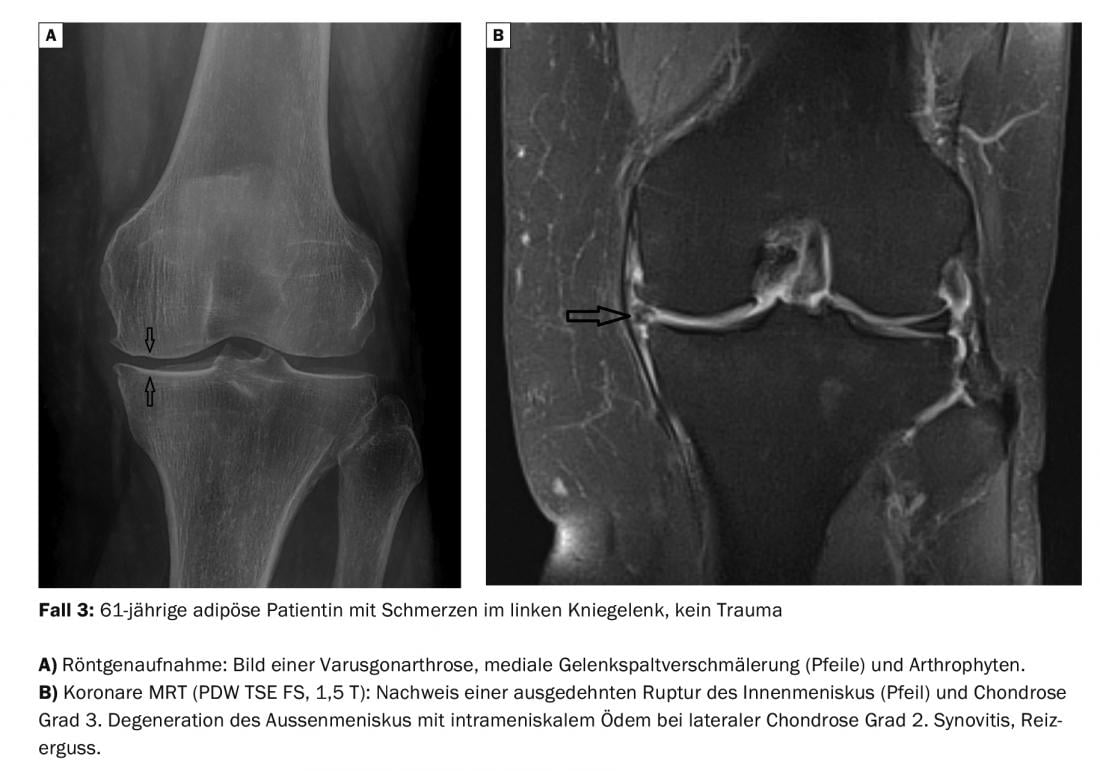
Case studies
In the cases presented here, priority is given to the wide range of information provided by magnetic resonance imaging in joint diagnosis. For this purpose, X-ray images and cross-sectional imaging methods are compared. The information on history and symptoms is limited to a small amount of information in order to focus on the differential image information.
Literature:
- Klauser AS, Wörtler K, Jaschke WR: General radiologic symptomatology of peripheral joints. Radiology up2date ; 3: 211-228.
- Kainberger F: Imaging of inflammatory rheumatic systemic diseases of the musculoskeletal system. Radiology up2date 2004; 4: 395-416.
- Hamers S, Freyschmidt J: “Leave me alone lesions” of bone – part 1. Radiology up2date 2002; 2: 189-214.
- Burgener F, et al: Differential diagnostics in MRI. Georg Thieme Verlag: Stuttgart/New York 2002: 354.
HAUSARZT PRAXIS 2019; 14(9): 40-42