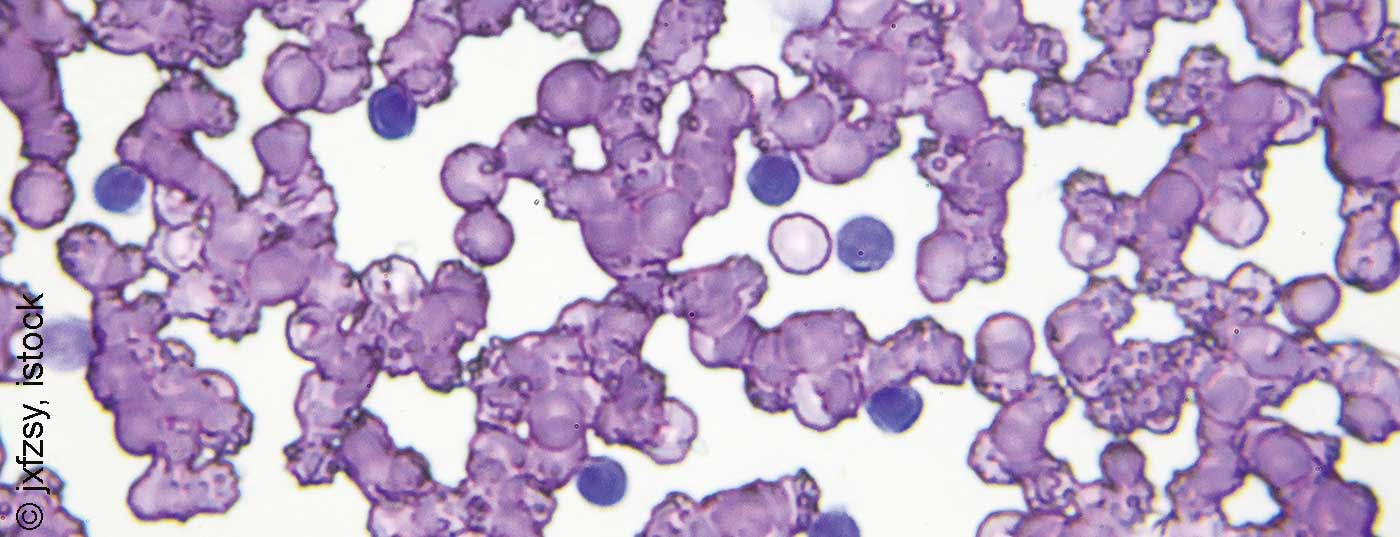
Valid prognostic and especially predictive markers can play a crucial role in the treatment of cancer. With the development of new therapeutic options for the treatment of chronic lymphocytic leukemia (CLL), risk stratification is also in constant flux.
The endeavor to predict our future is probably as old as mankind itself and does not stop at medicine. Thus, meteorologists, astrologers, fortune tellers, scientists and doctors are working all over the world to predict the course of events. In medicine in particular, this is probably also due to the great need to be optimally prepared for dangers. In disease patterns with such heterogeneous courses as in chronic lymphocytic leukemia (CLL), the importance of prognostic and predictive parameters for risk assessment is particularly high. Thus, certain diagnostic markers have a significant impact not only on prognosis but also on treatment. Their knowledge and application are essential for optimal patient management.
Searching for the needle in the haystack
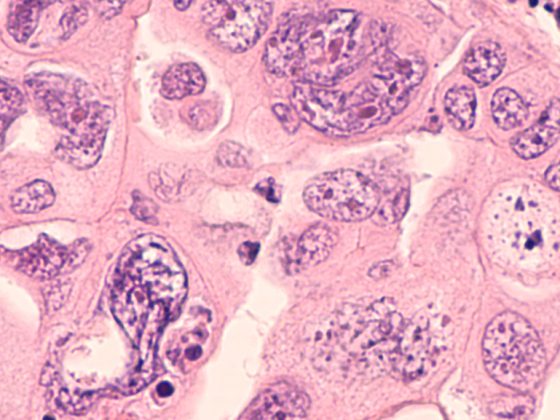
The rapid development of diagnostic and therapeutic options leads on the one hand to many parameters, the detection of which could potentially be useful for risk stratification, and on the other hand to multiple treatment options, which require a selection of suitable patients. Identifying those factors that are actually of clinical relevance concerns researchers more than ever in the era of targeted therapies. Targeted therapies with ibrutinib, idelalisib, and venetoclax have also become established in CLL.
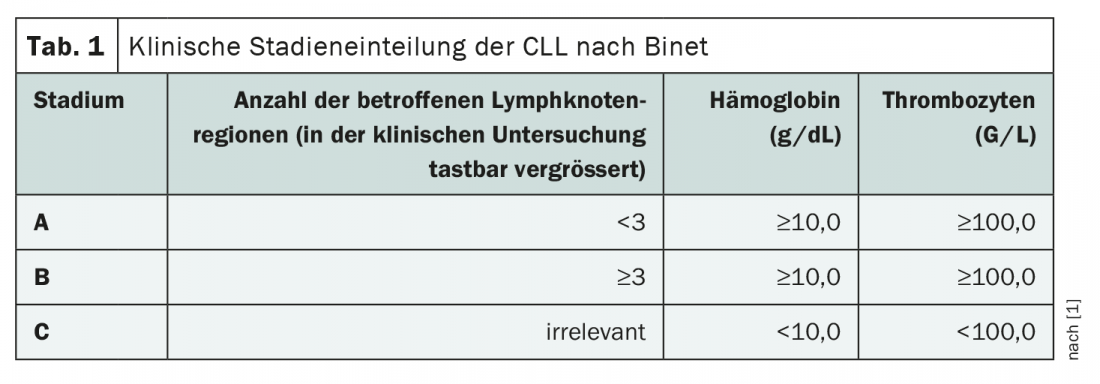
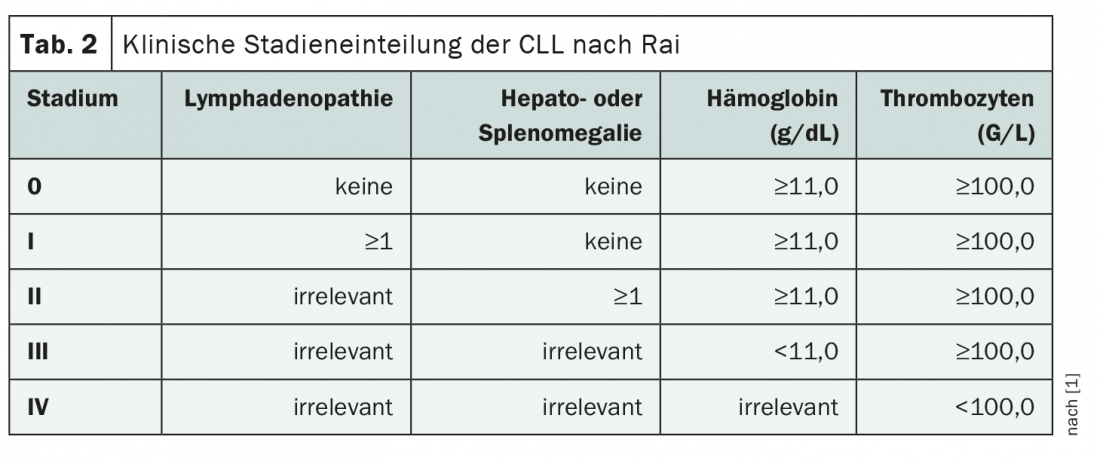
However, the development of prognostic scores and systems for CLL sufferers dates back over 40 years. Thus, in the 1970s and 80s, based on clinical findings, the staging according to Binet and Rai, which is still in use today, was developed [1]. These describe the spread of the disease taking into account lymph node, liver and spleen enlargements as well as blood count changes (Tab. 1 and Tab. 2). While the Binet classification is most commonly used in Europe, the Rai classification is widely used in the USA. In the meantime, numerous other biomarkers have been discovered and prognostic systems have been developed, but all have been validated for sufferers on chemoimmunotherapy (CIT) and must be questioned in the era of targeted treatments.
Identified prognostic biomarkers in recent decades include numerous serologic parameters, immunoglobulin heavy chain (IGHV ) mutation status, chromosomal aberrations, gene mutations, and micro-RNA findings, among others. In particular, a TP53 or NOTCH1 mutation, CD49d expression, IGHV mutation status, complex karyotypes, and certain microRNAs are of clinical relevance today, as these factors have immediate therapeutic consequences (Table 3) . However, the importance of these parameters is also undergoing change in the context of new treatment options for the most common form of leukemia. In an analysis published in 2019, only del17p/TP53 mutation and CD49d expression were still found to be negative prognostic biomarkers in the changing therapeutic landscape [2]. Even the role of minimal residual disease (MRD) as a prognostic parameter after therapy is being questioned in the era of targeted oncologic approaches [3].

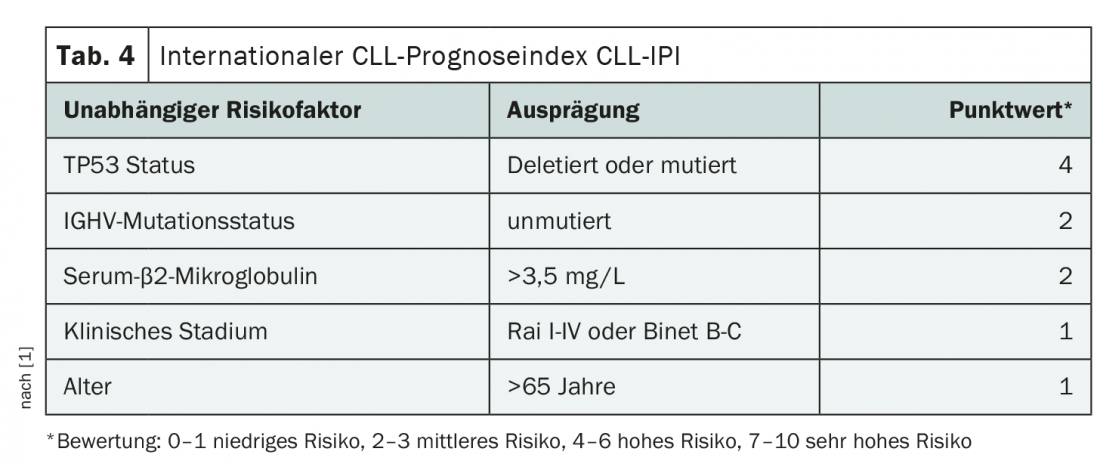
Over the years, prognostic models have also been developed repeatedly, taking into account various factors of clinical, laboratory and cytogenetic nature. Examples include the MDACC nomogram and the GCLLSG model. However, the CLL International Prognosis Index (CLL-IPI), introduced in 2016, has been particularly popular. In addition to TP53 and IGHV mutation status, serum-β2-microglobulin, clinical stage, and patient age are also taken into account in the assessment (Tab. 4) . Since there is often no immediate therapeutic consequence of this score, a rather cautious use is recommended [1].
Everything new?
The validity of many prognostic factors as well as scores identified over the past decades is under attack due to the current rapid introduction of new therapies. Nevertheless, the high relevance of adequate patient selection and thus the need for reliable biomarkers remains. The discovery of ever new, especially cytogenetic, parameters for risk assessment is certainly ongoing and while some established candidates are likely to fall victim to new developments, others will gain importance or be explored first. The clinical classification according to Binet and Rai still serves as a basis today, and there is no replacement of the original rock in sight. As far as more detailed analyses with consideration of cytogenetic factors are concerned, as is often the case in life and in medicine, it is important to remain dynamic!
Source: Yun X, Zhang Y, Wang X: Recent progress of prognostic biomarkers and risk scoring systems in chronic lymphocytic leukemia. Biomark Res 2020; 8: 40.
Literature:
- Oncology guideline program (German Cancer Society, German Cancer Aid, AWMF): S3 guideline on diagnosis, therapy, and follow-up for patients with chronic lymphocytic leukemia, abridged version 1.0, 2018, AWMF registry number: 018-032OL. www.leitlinienprogramm-onkologie.de/leitlinien/chronische-lymphatische-leukaemie-cll/ (last accessed 11/10/2020)
- Kittai AS, Lunning M, Danilov AV: Relevance of Prognostic Factors in the Era of Targeted Therapies in CLL. Curr Hematol Malig Rep 2019; 14(4): 302-309.
- Thompson M, et al: Minimal Residual Disease in Chronic Lymphocytic Leukemia in the Era of Novel Agents: A Review. JAMA Oncol 2018; 4(3): 394-400.
- Yun X, Zhang Y, Wang X: Recent progress of prognostic biomarkers and risk scoring systems in chronic lymphocytic leukemia. Biomark Res 2020; 8: 40.
InFo ONCOLOGY & HEMATOLOGY 2020; 8(6): 22-23.