In countries with regular screening, colorectal cancer is becoming increasingly rare. While colonoscopy can reduce mortality rates and prevent many carcinomas. However, the new quantitative immunological stool tests are better accepted by the population.
In the United States, where colorectal cancer screening has been intensively practiced for years, the number of new colon cancers in people over 55 years of age has approximately halved over the past 40 years [1]. In Switzerland, only a trend towards a decrease in colorectal cancer has been observed so far (NICER 2016). Every year, 4100 people in Switzerland develop colorectal cancer and 1600 die from it. A good 5% of Swiss people meet this fate. As the incidence rate increases with age, colorectal cancer and its prevention are of growing importance in our aging society. Treatment of colorectal cancer is burdensome and expensive. However, if colorectal cancer is detected early, before lymph nodes are affected or distant metastases have occurred, it can be cured without chemotherapy in over 90%. Without screening, less than 20%, but with screening, about 70% of detected carcinomas are at such an early curable stage [2].
Colorectal cancer is one of the few tumors for which effective screening options have been established. Randomized controlled trials [3–5] demonstrated that mortality from colorectal cancer can be reduced by stool testing for hidden blood. The non-specific haemoccult was later replaced by specific immunological stool tests. The benefit of endoscopic screening has also been demonstrated in randomized prospective population studies using sigmoidoscopy. Results of such studies with colonoscopy are not yet available. However, numerous cohort studies underscore that the benefits of colonoscopy are likely to be even greater. In 2013, the FOPH declared colorectal cancer screening by stool occult blood test and colonoscopy to be mandatory for people aged 50-69. These precautionary methods will be discussed here.
Are the new stool tests better?
Numerous immunological stool tests are offered in Switzerland. In contrast to Haemoccult, these have mostly been poorly validated or not validated at all in the population eligible for colorectal cancer screening. Hundt [4] showed that the sensitivity of these tests varies enormously regardless of the reported sensitivity to blood. In part, almost every second test is positive (often falsely) and only a few have acceptable specificity.
In contrast, the quantitative immunological stool tests (qFIT), OC Sensor and GOLD test, have been well validated in the screening setting [6–8] (the OC Sensor is increasingly available in Switzerland in various laboratories, currently to my knowledge in Laboratoires Clinique de La Source de Lausanne, Laboratory of the Cantonal Hospital Lucerne, ZetLab AG Zurich, labormedical Center Risch in Bern – in addition, the test can be obtained directly from the company MAST in Germany). They were also more efficient than the qualitative tests in a direct comparison. Even with a single stool sample, qFIT can detect colorectal cancer in about 80%; 70% of these are in a mostly curable early stage I [8,9]. With a “cut off” of 100 ng blood/ml buffer, less than 5% were false positives – i.e., neither carcinoma nor significant adenoma was found endoscopically. Less than 5% false positive also means that a positive test must be clarified endoscopically! Deeper “cut off” limits have improved the detection of large adenomas. The benefit of screening with repetitive qFIT over ten years is currently unclear. In the now six-year study in Holland (“cut off” 50 ng Hb/ml = 10 ug Hb/g stool) [3], extrapolated to 10,000 people, 86 carcinomas (52% stage I, 3% IV with distant metastases) occurred during this time with qFIT, but 109 carcinomas (16% stage I, 21% IV with distant metastases) occurred without screening. Individuals with screening were significantly more likely to survive than those without screening (79/86 [93%] vs. 44/109 [40%]).
What is secured during colonoscopy?
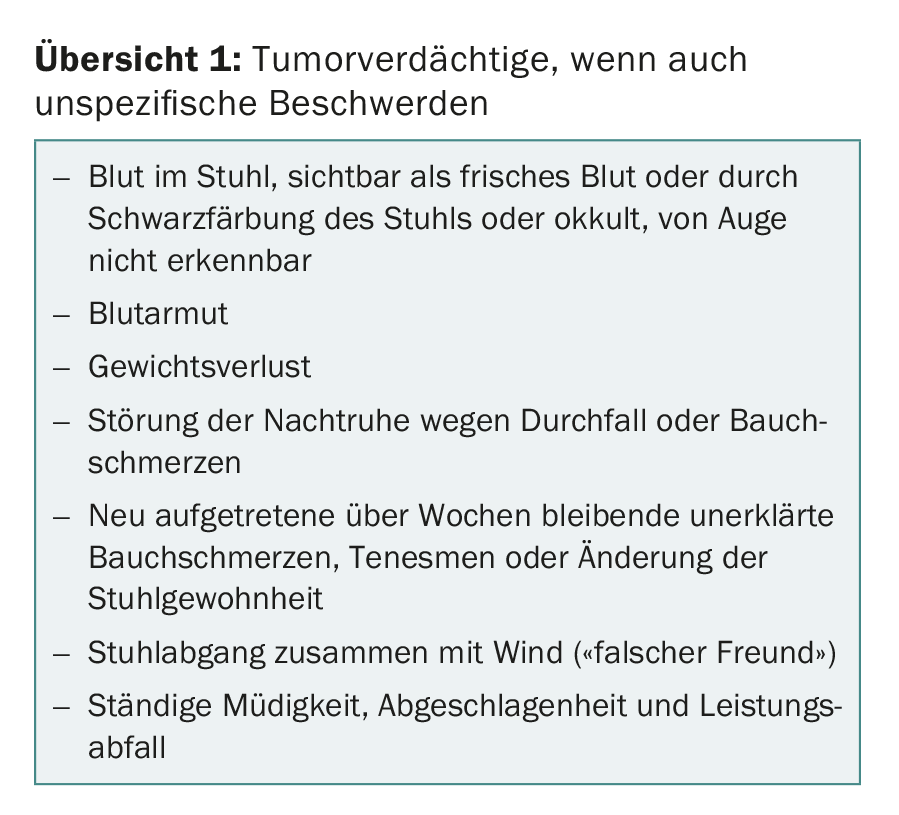
Colonoscopy extremely rarely misses colorectal cancer (better than qFIT). Therefore, suspicious tumor complaints (overview 1) must also be clarified endoscopically.
The prognosis of colorectal cancer depends primarily on the tumor stage at detection. By screening colonoscopy in symptom-free individuals over 50 years of age, colorectal cancer is found at an early stage in 70%.
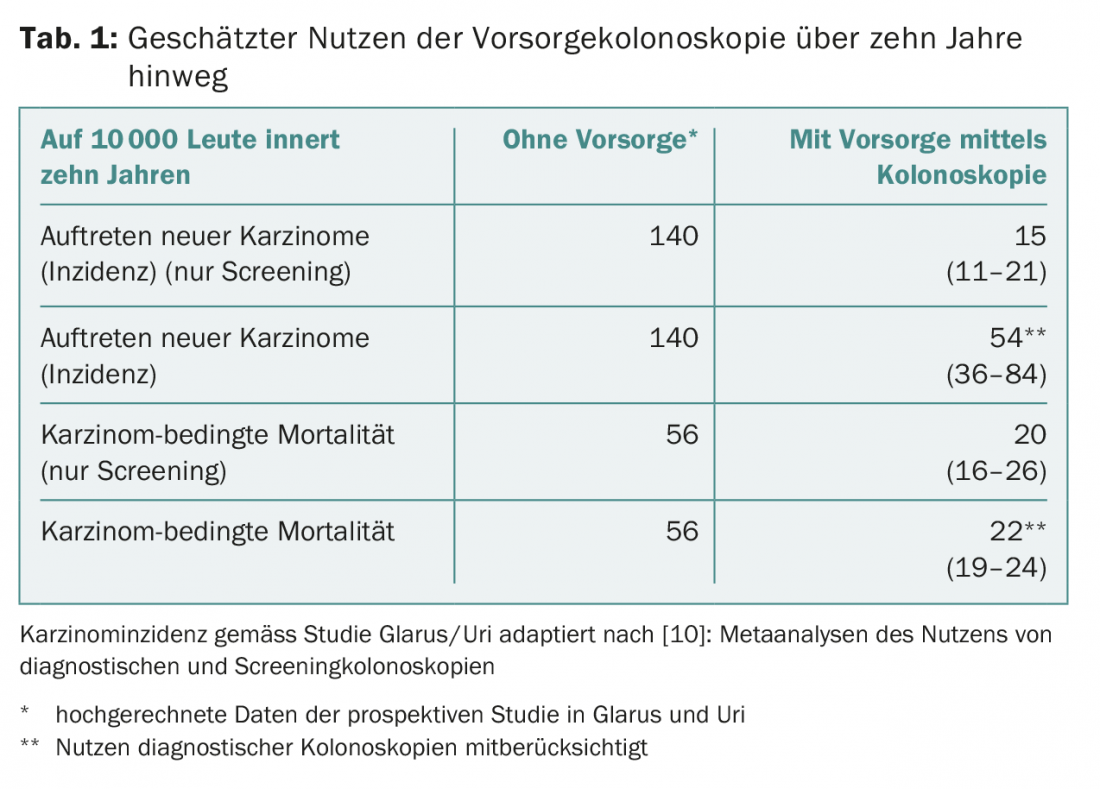
Randomized controlled population studies exist only for sigmoidoscopy [5]. However, at least one-third of colorectal cancers arise in the proximal colon. The potential additional benefit of screening by colonoscopy must be estimated from the numerous cohort studies. Table 1 shows an estimate based on a meta-analysis [10] with a total of 1,499,521 individuals. In part, diagnostic colonoscopies were included. The results fit well with our own prospective screening study. In the cohort study in Glarus and Uri [2], 22,818 individuals are prospectively followed. 1912 had a screening colonoscopy. In these, 70% fewer colorectal cancers occurred after six years (odds ratio 0.31, 95% CI 0.16-0.59; p<0.001) and colorectal cancer-related mortality was reduced over 80% (odds ratio 0.12, 95% CI 0.01-0.93; p<0.04). The data after 15 years underline these positive results (publication in preparation).
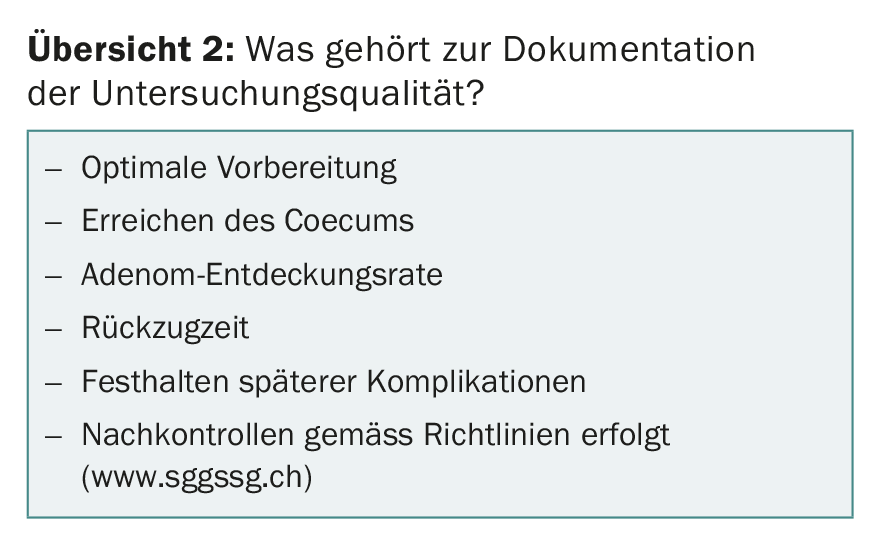
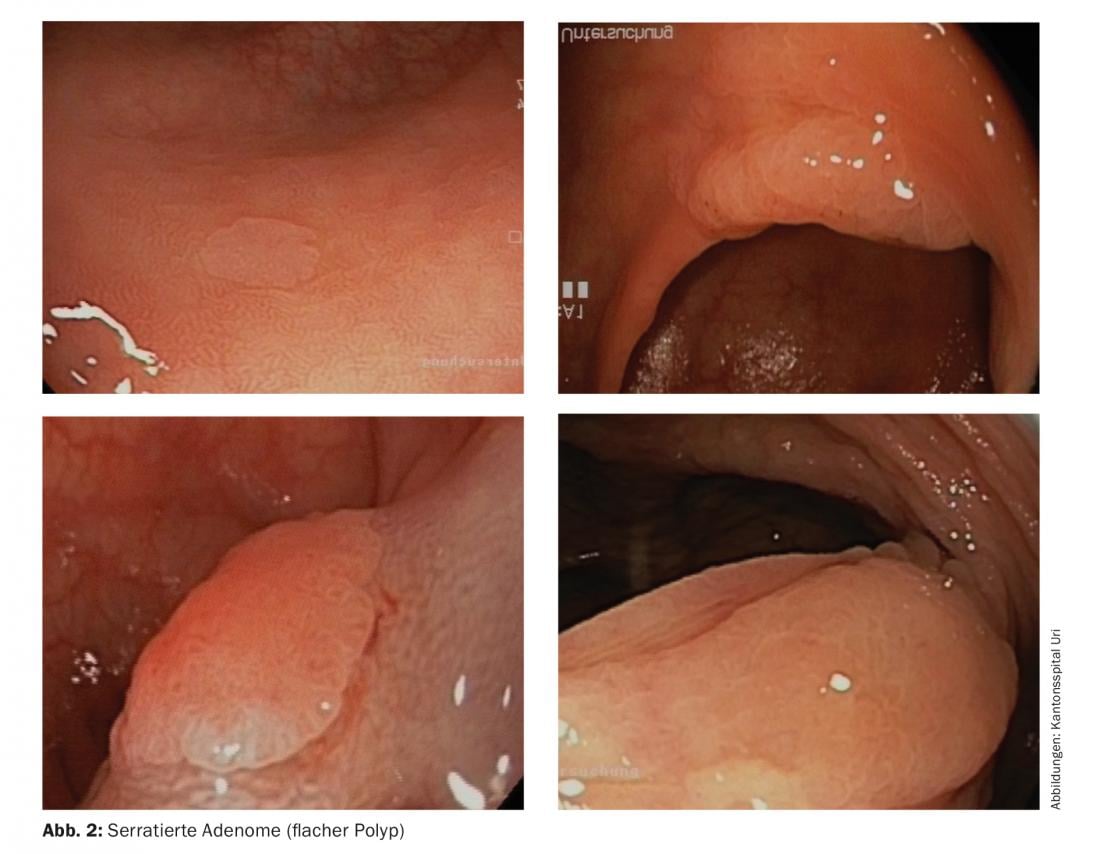
Despite these encouraging data, we know that even screening with colonoscopy every ten years cannot always prevent colorectal cancer. 5-10% of individuals with colorectal cancer had colonoscopy during the past decade (so-called interval cancers) [11,12]. 2.5% may even have been missed during colonoscopy. Possible reasons are insufficient bowel cleansing or insufficient care during endoscopy [11]. The more adenomas are found during endoscopy, the less frequently interval carcinomas occur later. This requires care and a sufficiently long examination time. Increasingly, it is required that the quality of the examination be documented (Overview 2) . In addition, not all adenomas have the same genetics and grow at different rates [13]. The classic fungus-like growing adenomas (Fig. 1) degenerate at the earliest after 10-20 years.
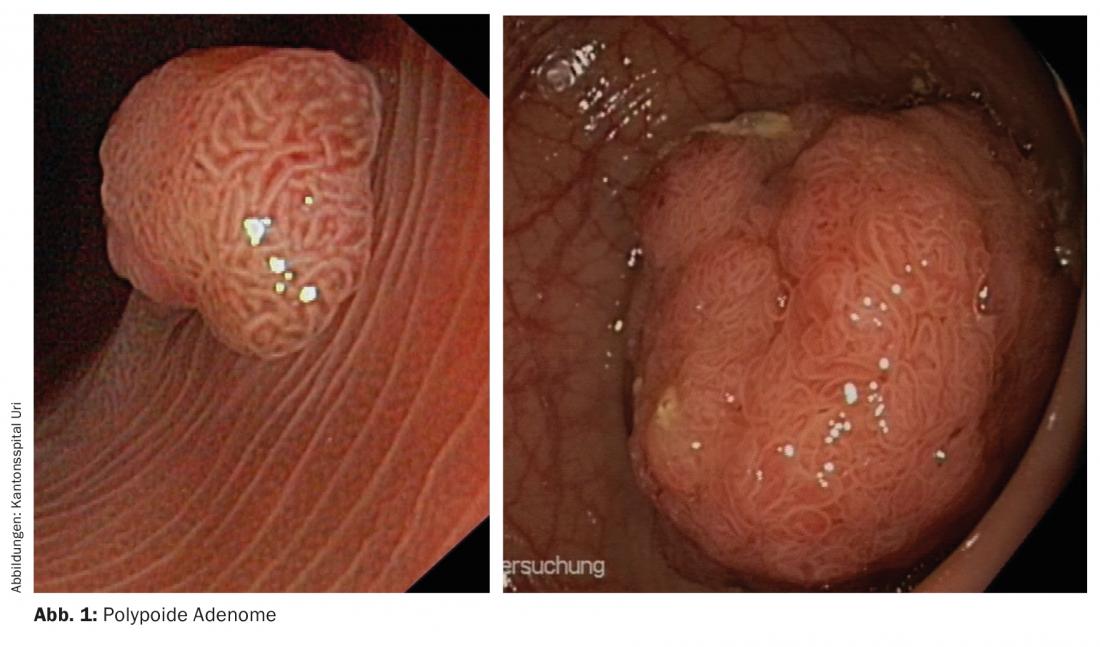
Flat serrated adenomas, on the other hand (Fig. 2), sometimes require only one to five years. These insidious serrated adenomas are clustered in familial tumor burden. They occur mainly in the proximal part of the colon, where they are also readily overlooked. This is a key reason why colonoscopy is less protective in the proximal colon. Another reason is that people are not followed up after adenomas are found. However, these individuals often grow new adenomas, which can then also degenerate. The necessary controls vary according to risk factors, number of adenomas found and histology (see guidelines of the Swiss Society of Gastroenterology at www.sggssg.ch).
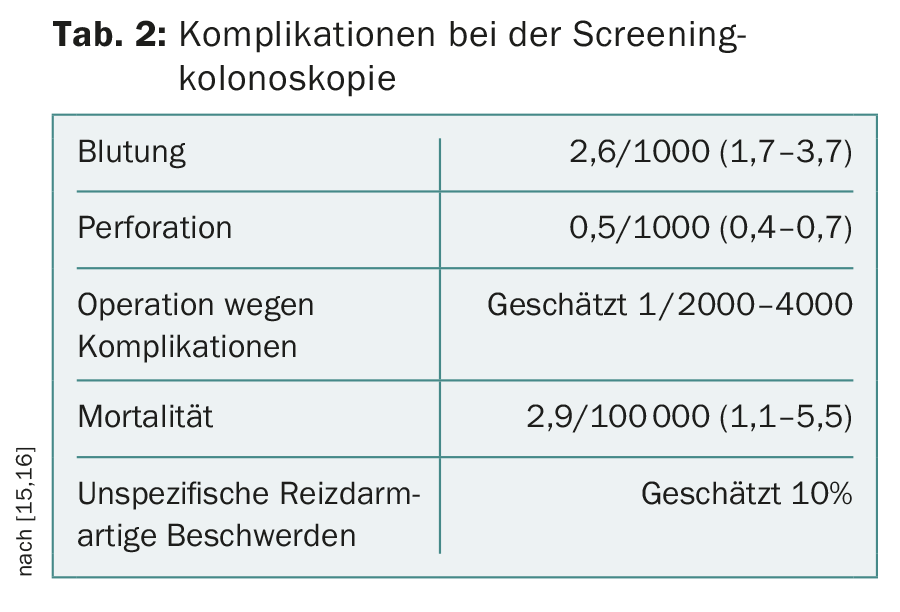
Colonoscopy is an invasive examination during which, although rare, complications can occur, especially when polyps are ablated (Tab. 2). Today, the examination itself can usually be performed with little pain thanks to sedative medication. But the preparation is tedious. For optimal preparation, a portion of the laxative should be drunk the day before and a portion on the day of the examination.
Prostate cancer and breast cancer screening also detects carcinomas that would never have led to symptoms (“lead time bias”). This is rare in colorectal cancer. According to a study from Germany [5], “insignificant” carcinoma is detected in one out of 1089 colonoscopies, especially in persons older than 75 years. On the other hand, however, numerous adenomas are unnecessarily ablated that would never have malignant degeneration.
qFIT or colonoscopy:To whom should what be recommended?
Since colorectal cancer predominantly occurs after the age of 50, colorectal cancer screening is recommended from then on. Recent data suggest that colorectal cancer is increasingly occurring in younger people, so that this recommendation may have to be corrected.
qFIT and colonoscopy are now established colorectal cancer screening methods. However, any precaution is only of use if people participate. Main advantages of qFIT are its ease of use and better acceptance. In Holland, 73% participated in screening with qFIT [3]. In southern Spain, more carcinomas were found in the group with qFIT than in the group with colonoscopy already at initial screening due to better acceptance [9]. In order for people to participate regularly in qFIT, they need to be personally invited back. The test material must be delivered immediately [3,6]. Thus, an adherence of up to more than 80% can be achieved. The second advantage of qFIT is that manpower is saved. With positive qFIT, it takes only 18 colonoscopies [9] to find carcinoma, whereas screening by colonoscopy requires 190.
Better detection of adenomas, potential colorectal cancer precursors, is the main advantage of colonoscopy. Therefore, colonoscopy is more suitable for colorectal cancer prevention. Colonoscopy detects more than twice as many adenomas as a single qFIT [9]. However, we will not know how this will look after ten years with qFIT repeated every two years and which method will ultimately result in fewer deaths from colorectal cancer until around 2022, when the results of the ongoing randomized screening trials will be available.
The choice of screening method depending on the risk of colorectal cancer?
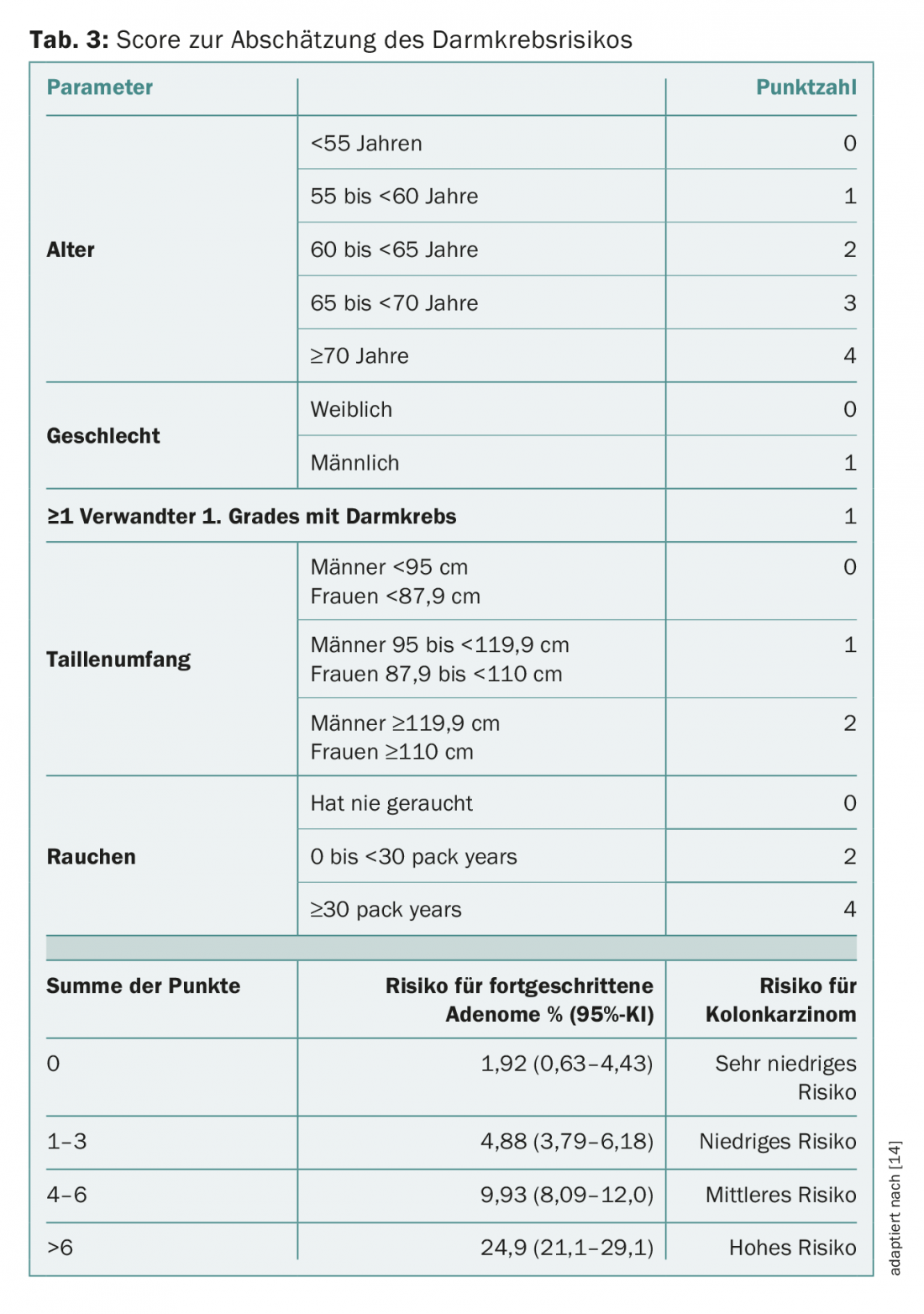
The cost of a screening program depends largely on the incidence of colorectal cancer and its precursors. There are people who have a very low risk of having a large adenoma or carcinoma. In these, it takes over 500 endoscopies to find a carcinoma, and probably over 2000 colonoscopies to find a carcinoma that would be missed with qFIT. This costs. Endoscopy is far more effective in people who have risk factors such as smoking, massive obesity, or a family history of tumors. In these, it takes only a few examinations to discover an important finding [14]. Imperiale developed a validated risk score for this purpose (Tab. 3). Especially people with a high risk of colorectal cancer benefit from endoscopic screening, while those with a very low risk could well choose qFIT as a preventive measure. This score was also recently used in an app (Gut Check) to help decide if and what preventive care makes sense.
Finally, there is a small group of people (<5%) who have a very high risk of colorectal cancer. These include familial tumor syndromes such as familial polyposis coli syndrome (FAP) and hereditary non-polyposis colon cancer syndrome (HNPCC). Preventive care protects these as well, but it must begin much earlier and be performed more frequently. The optimal precaution here must be discussed with the family doctor and the specialist. Inflammatory bowel diseases such as Crohn’s disease and ulcerative colitis also need a special screening program.
What does the future hold for us?
Significantly more sensitive than qFIT and almost as sensitive as colonoscopy is stool examination for a panel of genetic tumor markers together with qFIT [9]. This test has been approved by the FDA in the USA, but is not yet available in Switzerland. At the moment, this test is still very expensive and often false positive, resulting in unnecessary colonoscopies. Moreover, it is hardly practicable, since whole portions of stool have to be sent in. However, these genetic stool tests are very promising for the future. Blood tests for tumor markers are already offered in Switzerland. However, these tests are still insufficiently validated in the screening population. In the few screening studies, they were no better than the old qualitative stool tests. Even the expensive capsule endoscopy is not yet sufficiently validated. Colonoscopy by computed tomography is not considered for population screening simply because of radiation exposure and poor sensitivity for flat adenomas.
It is estimated that the treatment of colorectal cancer today costs CHF 100,000. The new immunotherapies will make treatment even more expensive. Today, colorectal cancer screening not only enables more patients to be cured and chemotherapy and radiation to be avoided, but increasingly even saves costs. It is encouraging that more and more cantons are planning colorectal cancer screening programs with colonoscopy and/or qFIT.
Take-Home Messages
- Colorectal cancer screening is now well established and efficient. In countries with regular screening, colorectal cancer is becoming increasingly rare.
- Colonoscopy can massively reduce mortality from colorectal cancer and prevent the formation of many carcinomas.
- The new quantitative immunological stool tests are far better accepted by the population and detect many carcinomas at potentially curable early stages.
- Individuals with an increased risk of colorectal cancer are recommended to undergo screening by colonoscopy.
- Complaints must be clarified correctly. A stool test is not sufficient here.
Literature:
- Siegel RL, et al: Colorectal cancer CRC incidence in the USA 1974-2013. J Natl Cancer Instit 2017; 109: djw322.
- Manser CN, et al: Colonoscopy screening markedly reduces the occurrence of colon carcinomas and carcinoma-related death: a closed cohort study. Gastrointest Endoscopy 2012; 76: 110-117.
- Van der Vlugt M, et al: Interval colorectal cancer incidence among subjects undergoing multiple rounds of fecal immunochemical testing. Gastroenterology 2017; 153: 439-447.
- Hundt S, Haug U, Brenner H: Comparative evaluation of immunochemical fecal occult blood tests for colorectal adenoma detection. Annals Intern Med 2009; 150: 162-169.
- Brenner H, et al: Prevention, early detection and overdiagnosis of colorectal cancer within 10 years of screening colonoscopy in Germany. Clinical Gastroenterol Hepatol 2015; 13: 717-723.
- Jensen CD, et al: Fecal immunochemical test program performance over 4 rounds of annual screening. A retrospective cohort study. Ann Intern Med 2016; 164(7): 456-463.
- Lee JK, et al: Accuracy of fecal immunochemical tests for colorectal cancer: systematic review and meta-analysis. Ann Intern Med 2014; 160: 171.
- Imperiale TF, et al: Multitarget stool DNA testing for colorectal-cancer screening: New Engl J Med 2014; 370: 1287-1297.
- Quintero E, et al: Colonoscopy versus fecal immunochemical testing in colorectal-cancer screening. New Engl J Med 2012; 366: 697-706.
- Pan J, et al: Colonoscopy reduces colorectal cancer incidence and mortality in patients with non-malignant findings: a meta-analysis. Am J Gastroenterol 2016; 111(3): 355-365.
- Corley DA, et al: Adenoma detection rate and risk of colorectal cancer and death. New Engl J Med 2014; 370: 1298-1306.
- Samadder NJ, et al: Characteristics of missed or interval colorectal cancer and patient survival: a population-based study. Gastroenterology 2014; 146: 950-960.
- Carethers JM, Jung BH: Genetics and genetic biomarkers in sporadic colorectal cancer. Gastroenterology 2015; 149: 1177-1190.
- Imperiale TF, et al: Derivation and validation of a scoring system to stratify risk for advanced colorectal neoplasia in asymptomatic adults. Ann Intern Med 2015; 163: 339-346.
- Reumkens A, et al: Post-colonoscopy complications: a systematic review, time trends, and meta-analysis of population-based studies. Am J Gastroenterol 2016; 111(8): 1092-1101.
- Lin JS, et al: Screening for colorectal cancer: updated evidence report and systematic review for the US Preventive Services Task Force. JAMA 2016; 315: 2576-2594.
InFo ONCOLOGY & HEMATOLOGY 2018; 6(2): 6-10.