In the SYNTAX study, a total of 1800 patients were randomized in 85 hospitals in the United States and Europe. The two treatment groups were one interventional and the other surgical. The so-called SYNTAX score was used to assess the complexity of the coronary lesion. In this article, read the presentation of the study design and the presentation of the results of the SYNTAX study, as well as comments and assessments of the results.
In the treatment of coronary artery disease, a deep chasm remains between the recommendations of professional societies and daily practice, although the merits of percutaneous intervention (dilatation and stent implantation) and surgical revascularization (bypass grafting) have been verified by more than 20 randomized clinical trials over the past two decades.
Study design
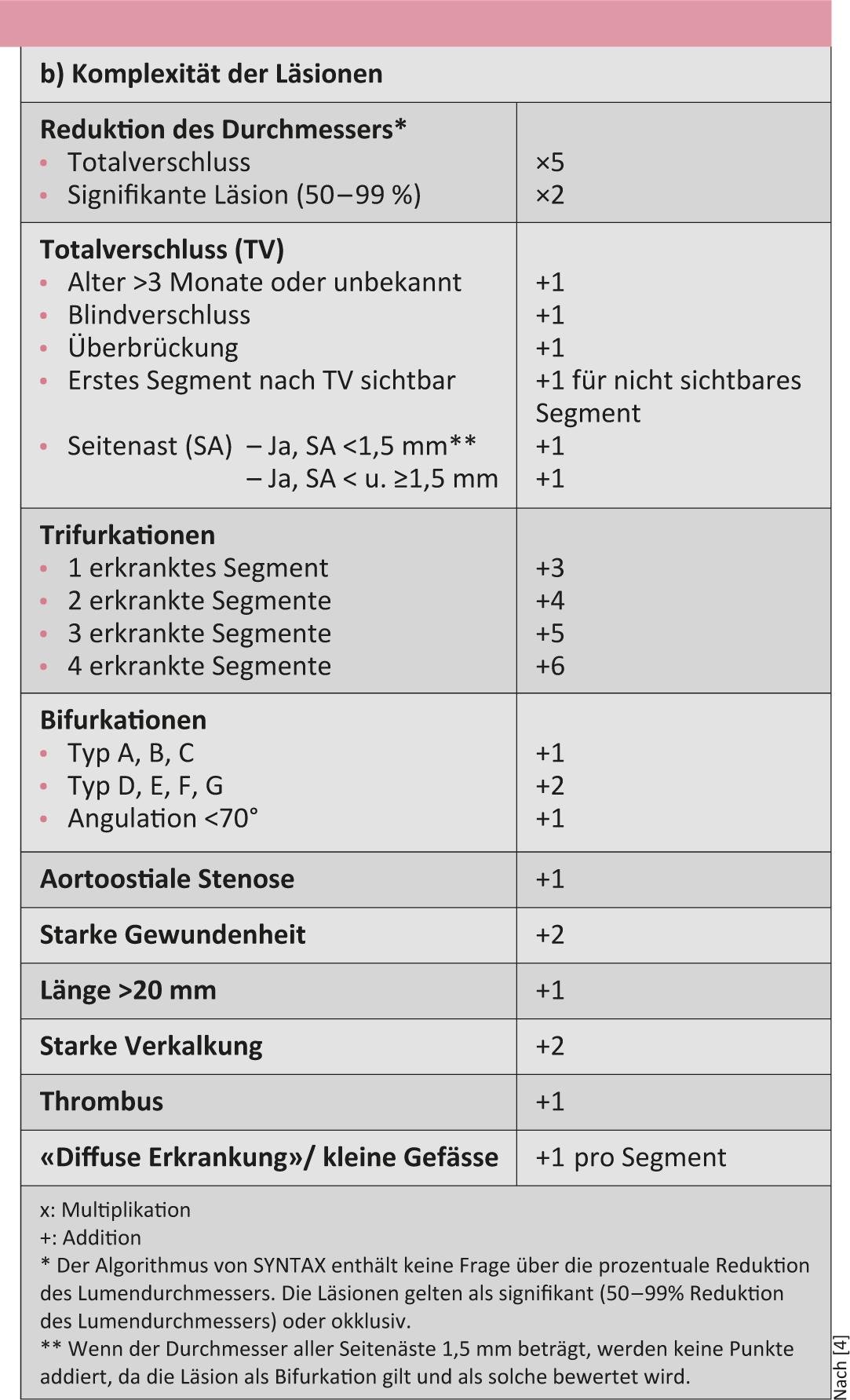
In the SYNTAX trial, 1800 patients in 85 hospitals in Europe and the United States were randomized to either an interventional treatment group (n=903) with insertion of paclitaxel-eluting stents or to a surgical group. Recruitment for this study occurred after each patient with de novo coronary three-vessel disease and/or main stem stenosis was evaluated at the centers by a cardiologist and a surgeon as a candidate for both treatment options. Patients in whom both therapeutic options could be recommended were randomized. Both groups (interventional and surgical) had comparable SYNTAX scores (28.4 vs. 29.1). Patients who qualified for PCI only were placed in the PCI registry, and patients who qualified for surgical treatment only were placed in the bypass registry. The complexity of coronary lesions was assessed in all patients using the so-called SYNTAX score(Table 1). This score is expected to predict outcome after revascularization.

For the primary end point at one year (major cardiac and cerebrovascular events), percutaneous interventional therapy surprisingly failed to meet the criteria of “not inferiority” due to higher rates of repeat revascularization after PCI compared with surgical treatment [1]. After three years, rates of myocardial infarction and repeat revascularization were significantly higher after PCI than after bypass surgery [2].
Results of the SYNTAX study
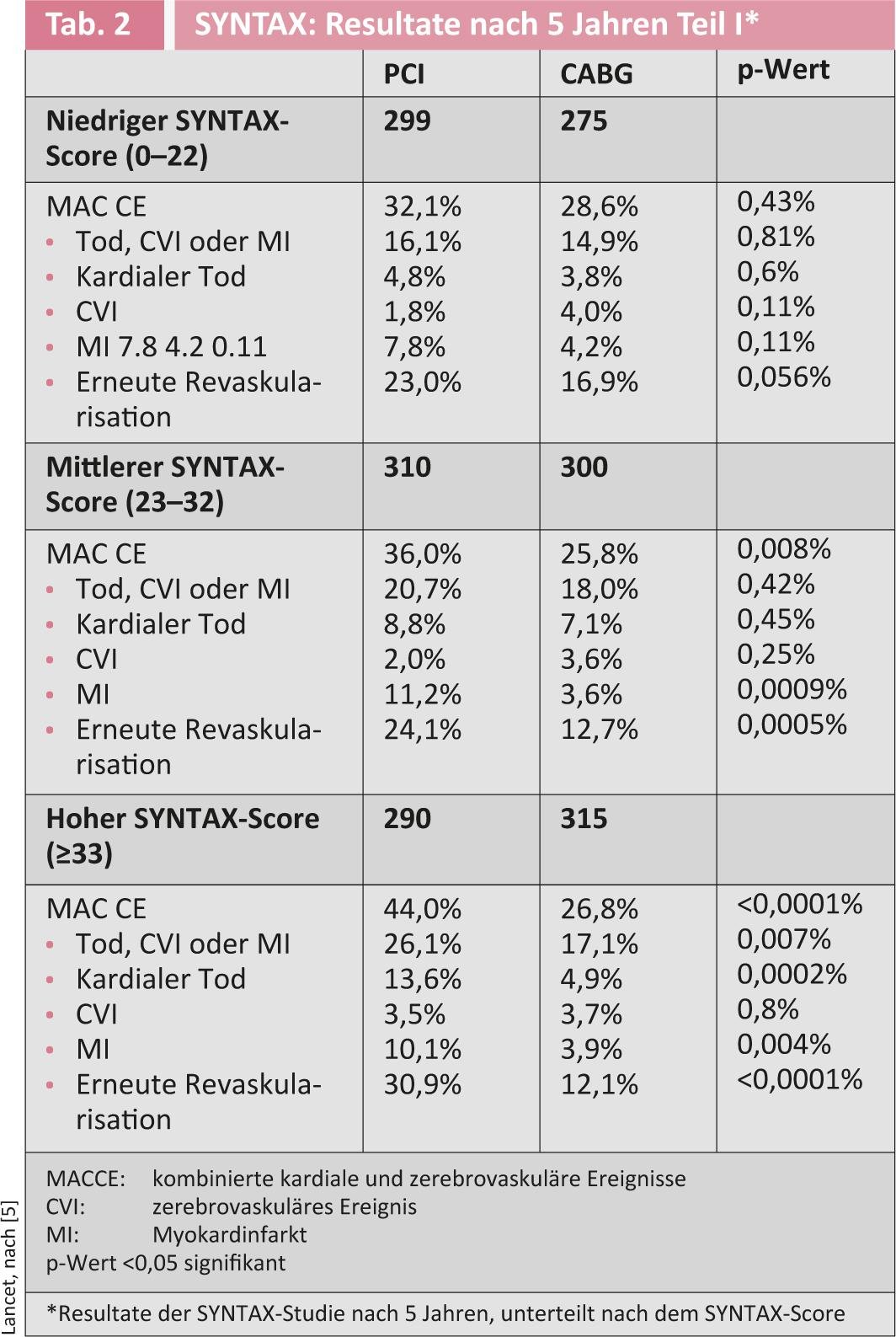
After five years, the rate of significant cardiac and cerebral events determined by Kaplan-Meier analysis was 26.9% in the bypass group and 37.3% in the interventional group (p<0.0001) [3]. The probability of myocardial infarction and repeat revascularization was 3.9% in the surgical group vs. 9.7% in the interventional group, respectively. 13.7% vs. 25.9%. Kaplan-Meier analysis for cardiac mortality showed 5.3% in the bypass group vs. 9% in the stent group (p=0.003). The same end points are shown for the groups with different SYNTAX scores (0-22, 23-32, ≥33). The higher the SYNTAX score, the better surgery performed (Table 2).
Interestingly, in the first year after treatment, antiplatelet agents were used significantly more frequently after percutaneous than after surgical revascularization. After five years, the incidence was comparable, but patients after percutaneous intervention were more likely to receive dual antiaggregation therapy.
The authors summarized that surgical revascularization for coronary three-vessel disease and/or main-stem stenosis is the standard approach for complex anatomy (defined using the SYNTAX scoring system). For patients with simpler coronary anatomy, percutaneous intervention can be performed with acceptable results. All patients with complex coronary artery disease (including small vessels, bifurcation stenosis, long stenosis, etc.) must be carefully and individually discussed by a joint cardiac team consisting of cardiologists and cardiac surgeons to ensure optimal treatment.
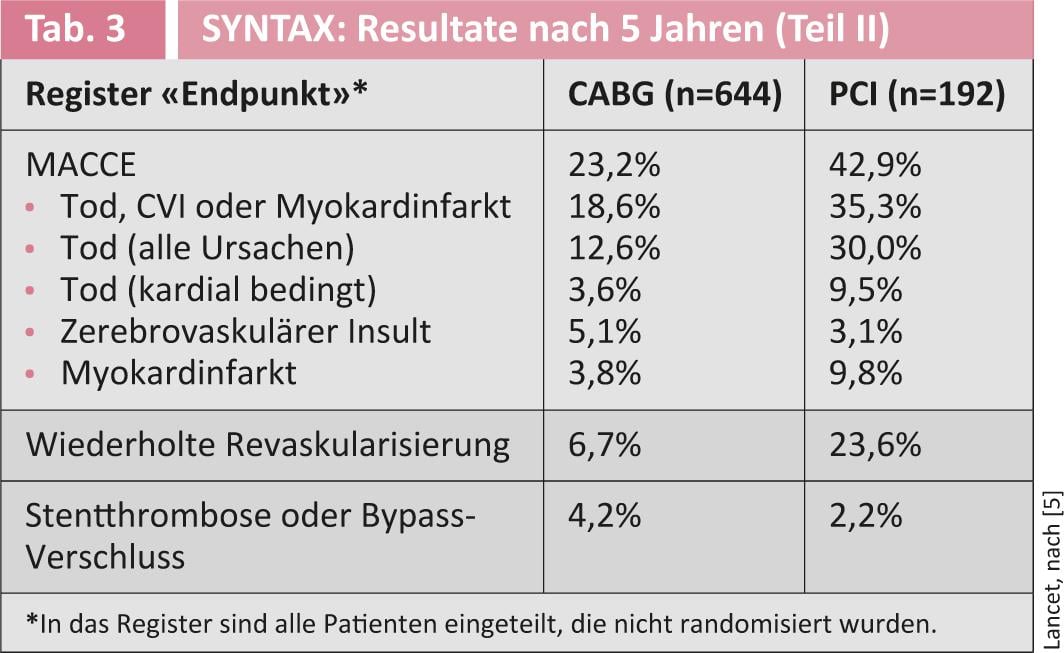
However, not only the results of the randomized trial are interesting, but also those of the respective registries (percutaneous or surgical). Table 3 summarizes these results.
Comment
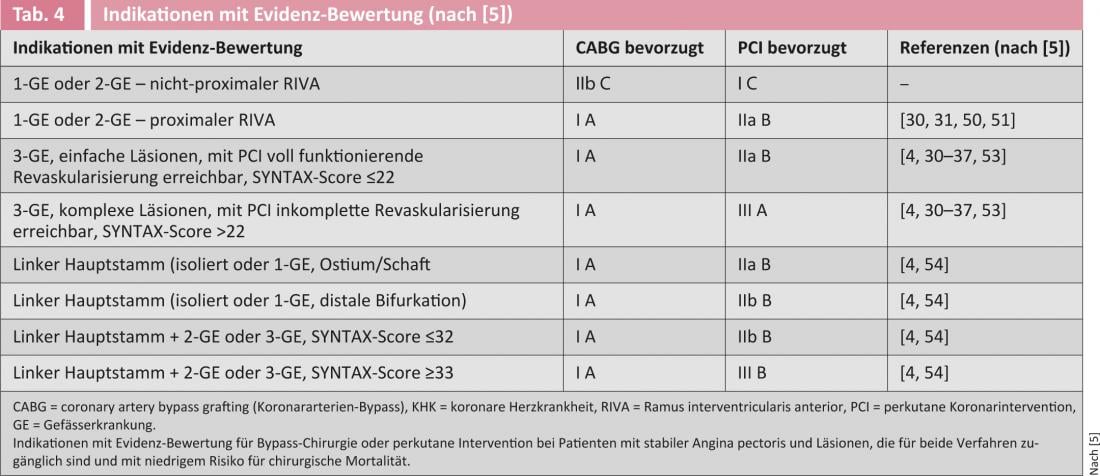
In the most recent recommendations of both European professional societies, all accepted indications for surgery are listed with evidence level IA, and for all situations involving the left main stem, the evidence for surgery is clearer than for percutaneous intervention. Only in simple 1- or 2-vessel disease is the indication for percutaneous intervention rated higher than surgical treatment. However, many institutions often place themselves above these “evidence-based” indications, for whatever reason(Table 4).
Thus, it remains questionable whether the SYNTAX study could represent daily clinical situations. The inclusion criteria were very restrictive, so that hardly more than 5% of all treated patients were included. With a total of 1800 patients from 85 centers, an average of 20-25 patients per center were randomized, although many of these centers perform over 500 bypass surgeries and over 1500-2000 coronary interventions annually. Why? Many patients are led to believe that stents are gentler and less dangerous than bypass surgery because access to the diseased coronary artery involves only a femoral artery puncture and no sternotomy is required. Rather less frequently, side effects of stent placement are discussed: for example, the need for more complex platelet aggregation inhibition with the potential disadvantages for patients who need to undergo another procedure following coronary intervention. There is also a perception in the lay world that since the introduction of drug-eluting stents, the incidence of recurrence has disappeared. Cardiac surgery cannot confirm this impression; on the contrary, patients who have received multiple catheter interventions in their history are very often treated surgically today.
The formation of cardiac teams is now a must for every cardiovascular disease reference center, and not only for patients suffering from severe aortic stenosis. Coronary findings must also be discussed on an interdisciplinary basis. This means that when indications are debatable, diagnostic coronary angiography should not occur in the same session as interventional treatment. The patient must be able to decide calmly and after considering all the facts that were discussed during the information session. If the findings are severe, a decision on the catheter table seems obsolete to us.
Actually, in addition to the isolated view of the discovered coronary lesion, other factors should also be increasingly taken into account when determining the indication: Benefit, risk, consequences, patient wishes and, last but not least, costs. The KVG has defined this with the WZW criteria.
A second study recently confirmed the positive results of bypass surgery. The objective of the FREEDOM trial was the following: Can aggressive drug treatment in combination with percutaneous interventions using drug-eluting stents change the strategy of treating diabetic patients with multivessel coronary artery disease?
1900 diabetic patients were randomized between 2005 and 2010 [6]. The study was designed as a “superiority trial”, with an average observation period of approximately four years. All patients received optimal management of cholesterol levels, systolic blood pressure levels, and serum glucose. The following factors were analyzed: Death (all causes) and nonfatal myocardial infarction and cerebrovascular insult. The 5-year mortality was 26.6% in the intervention group versus 18.7% in the bypass group (p=0.049). The advantage of surgical bypass was confirmed in the lower rate of myocardial infarction (p<0.001). A cerebrovascular event was slightly more common at five years after bypass surgery (5.2%) than after percutaneous intervention (2.4%). These results were also confirmed according to angiographic complexity (syntax score), left ventricular ejection fraction, and renal function. There is no doubt, even after this study, that bypass surgery remains the best therapeutic option in diabetic patients with advanced coronary artery disease.
Such results were already published in the mid-1990s (BARI study) and later confirmed with the ARTS, CARDia and SYNTAX studies. Despite these clear results, clinical practice has not changed significantly. The reason for this is that the higher rate of cardiovascular events was mainly due to a higher need for repeat revascularizations in the group initially treated with stenting [7].
This was different in the FREEDOM trial, where the benefit of surgical revascularization was predominantly explained by a reduction in the rate of myocardial infarction and death (all causes). The results of this study correlate with the clinical observation that patients after stent placement not infrequently show a significant decrease in pump performance over the long-term course due to repeated minor infarcts. Concomitant drug treatment is of great importance in all patients with diabetes and coronary artery disease. In contrast to the SYNTAX trial, patients in both groups (PCI or bypass) were followed up with antiplatelet agents with comparable frequency in the FREEDOM trial.
Conclusion
Highly specialized cardiovascular medicine must increasingly address the evidence of different treatment strategies. With the ever faster introduction of innovations (procedures but also implants) and depending on technological progress, it has become increasingly difficult in certain medical specialties to accept the established evidence or to practice according to this evidence.
- New technologies are introduced more and more quickly on the occasion of studies, approved for the market and also replaced by newer ones more and more quickly. At the same time, the cost of certain questionably proven technologies is very expensive and not socio-economically justifiable for much longer in a health care system facing increasing austerity.
- There is pressure to innovate in many institutions; industry partners are increasingly interfering in the definition of treatment indications and designing study protocols that should be used to test their products.
- The criteria for the approval of new technologies (e.g. implants) on the European market are relatively easy to fulfill. Many new products are introduced without thorough scientific testing. Evidence runs after practice.
- High-quality, prospective randomized trials are not infrequently useless in this area because new technological advances have been made before the high-quality trials can be assessed with a midterm view or are even completed.
- Specialties that use complex technologies are also often the first point of contact for patients and perform a “gate keeper” function. Providers who offer only interventional therapies often no longer even consider surgical treatment options.
- Patients are persuaded with arguments such as ‘rapid therapy’ and ‘puncture instead of incision’. For patients and their relatives, the sustainability and uniqueness of a treatment are often of far greater interest.
- It is false that patients treated primarily by catheterization can still be treated surgically if they fail with equal risk. The surgical risk is greater for many procedures when primarily interventional rather than surgical treatment is used.
Literature:
- Serruys PW, et al: N Engl J Med 2009; 360: 961-972.
- Kappetein AP, et al: Eur Heart J 2011; 32: 2125-2134.
- Mohr FW, et al: Lancet 2013; 381: 629-638.
- Sianos G, et al: EuroIntervention 2005; 1: 219-227.
- Guidelines on myocardial revascularization. The Task Force on Myocardial Revascularization of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS). Eur J Cardio-thoracic Surg 2010; 38: S1-S52.
- Farkouh ME, et al: N Engl J Med 2012; Nov 4, (Epub ahead of print).
- Farooq V, et al: Incidence and multivariable correlates of longterm mortality in patients treated with surgical or percutaneous revascularization in the Synergy between PCI with Taxus and Cardiac surgery (SYNTAX) trial. Eur Heart J 2012; Oct 26, (Epub ahead of print).
- Hlatky M.: Compelling Evidence for Coronary-Bypass Surgery in Patients with Diabetes. N Engl J Med 2012, Nov 4, 2012, (Epub ahead of print).