An international research team involving the University Hospitals of Lausanne and Zurich has compared different diagnostic methods in a large-scale retrospective study. In agreement with previous empirical findings, the conclusion of the study is that molecular methods are superior to conventional fungal diagnosis when onychomycosis is suspected.
With an estimated prevalence of 4-9% in the general population, onychomycoses are the most common cause of abnormal appearance of the nail apparatus [1,2]. Rapid and reliable pathogen identification is crucial to initiate the appropriate therapy as quickly as possible. Compared to conventional diagnostic methods, molecular methods are faster and have higher accuracy in species identification. Currently available molecular diagnostic tools differ mainly in the methods of DNA extraction, PCR primers used, and PCR analysis products [3]. Compared to conventional diagnostic methods, molecular methods are faster (findings within one day) and have higher accuracy, which is very attractive for application in clinical practice [4].

Fluorescence microscopy and fungal culture vs. PCR sequencing
A total of 16 094 nail samples were examined by direct fluorescence microscopy [1]. In addition, two fungal cultures were obtained from each sample using Sabouraud dextrose agar with chloramphenicol (50 μg/mL) and chloramphenicol plus cycloheximide (400 μg/mL). By direct fluorescence microscopy, fungal elements were detected in 68.1% of the nail samples; by fungal culture, the detection rate was 28.7%. The two methods showed an overall concordance of 58.4%. The majority of the discrepant results resulted from samples with positive direct microscopy findings but negative fungal culture. In a total of 59.5% of the samples in which fungal elements were detected by fluorescence microscopy, the fungal culture was negative. Among patients with a positive fungal culture result, dermatophytes accounted for the largest proportion (47.9%), with Trichophyton rubrum being the most common pathogen, followed by “non-dermatophyte molds” (NDMs) (29.1%), yeasts (21.8%), and mixed infections (1.2%). In 1148 cases, conventional fungal diagnosis by fluorescence microscopy and fungal culture proved insufficient, so additional molecular diagnostic workup was used (Table 1) [1].
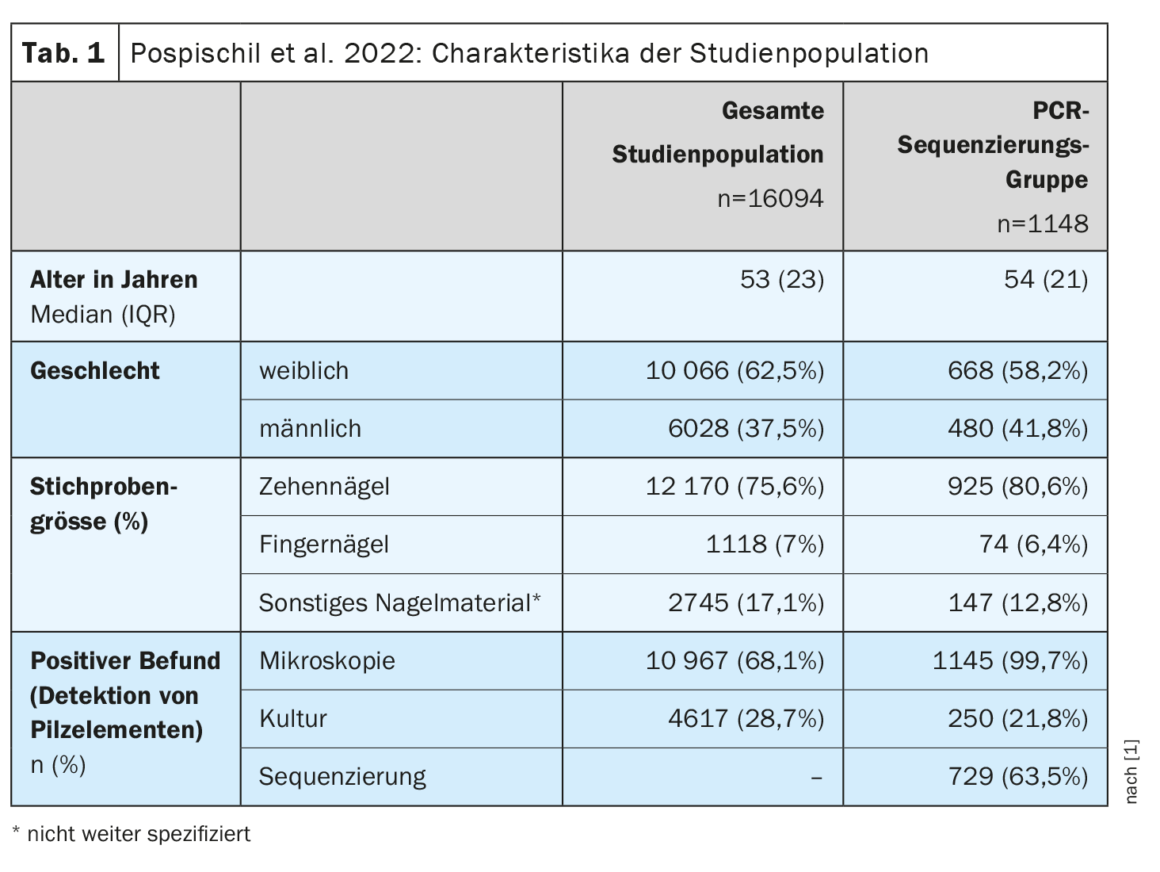
Fungal culture detected fungal pathogens in only 21.8% of cases, showing low sensitivity, while PCR sequencing proved clearly superior with a detection rate of 63.5%. The frequency distribution of the different fungal elements identified by PCR sequencing was as follows: NDMs 67.6%, yeasts 26%, dermatophytes 4.8%, and mixed infections 1.6%.
| The retrospective cohort study included nail samples from patients referred to the specialized dermatomycology laboratory of the Department of Dermatology at the University Hospital of Lausanne (CHUV) in 2013-2018 due to clinical suspicion of onychomycosis. In all cases in which conventional mycological diagnostics did not yield clear findings, PCR sequencing was performed. according to [1] |
Literature:
- Pospischil I, et al: Identification of Dermatophyte and Non-Dermatophyte Agents in Onychomycosis by PCR and DNA Sequencing-A Retrospective Comparison of Diagnostic Tools. Journal of Fungi 2022; 8(10): 1019.
- Sigurgeirsson B, Baran R: The prevalence of onychomycosis in the global population – A literature study. JEADV 2014; 28: 1480-1491.
- Verrier J, Monod M: Diagnosis of Dermatophytosis Using Molecular Biology. Mycopathologia 2017; 182: 193-202.
- Petinataud D, et al: Molecular diagnosis of onychomycosis. J Mycol Med 2014; 24: 287-295.
DERMATOLOGY PRACTICE 2023; 33(1): 39