The updated guideline recommends important innovations in the areas of screening, cardiovascular risk assessment in diabetes mellitus and aspects of evidence-based cardiovascular risk reduction in type 2 diabetes patients with atherosclerotic cardiovascular disease, heart failure and chronic renal insufficiency.
The new European Society of Cardiology (ESC) guidelines for the management of cardiovascular disease in patients with diabetes have been developed to reflect the fact that patients with type 2 diabetes (T2DM) are more than twice as likely to develop cardiovascular disease as patients without diabetes. The guidelines emphasize the importance of prevention and management of cardiovascular disease in patients with diabetes. They recommend systematic screening for diabetes in all patients with cardiovascular disease and vice versa to assess the risk and presence of cardiovascular disease in all patients with diabetes.
Cardiovascular risk assessment and –
categorization
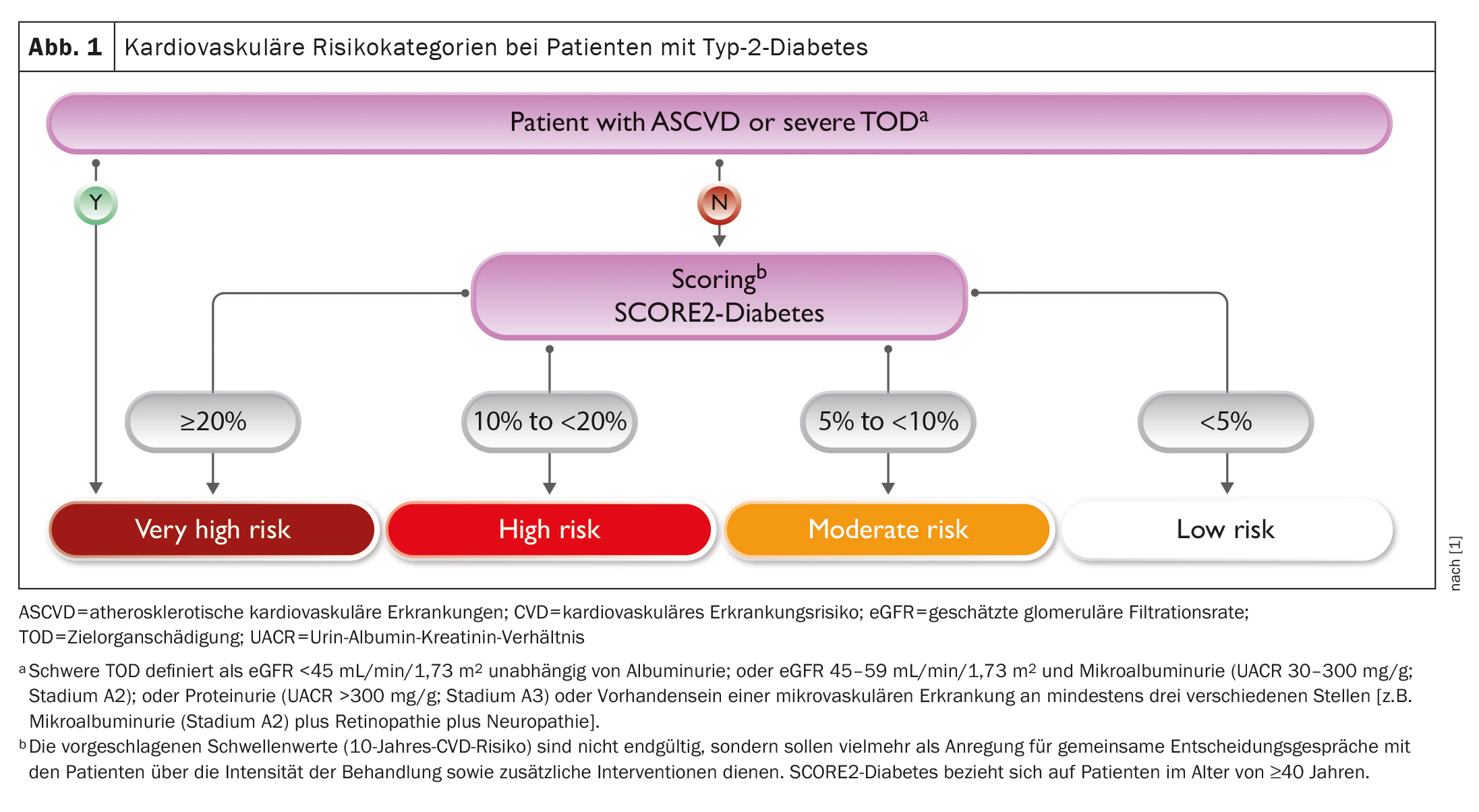
The presence of cardiovascular disease and severe end organ damage should be evaluated in all patients with diabetes. Severe end organ damage is defined by estimated glomerular filtration rate (eGFR), albumin-to-creatinine ratio in spontaneous urine (UACR) or the presence of microvascular disease at at least three different sites (e.g. microalbuminuria plus retinopathy plus neuropathy). Patients with T2DM and cardiovascular disease or severe end organ damage are categorized as having very high cardiovascular risk.
SCORE2: New 10-year risk score
For patients with T2DM without atherosclerotic cardiovascular disease or severe end-organ damage, the new guidelines introduce a new 10-year cardiovascular risk score (SCORE2-Diabetes). SCORE2-Diabetes integrates information on conventional cardiovascular risk factors (age, smoking status, systolic blood pressure, total and high-density lipoprotein cholesterol) with diabetes-related information (age at diabetes diagnosis, HbA1c and eGFR) to categorize patients into low, moderate, high or very high cardiovascular risk (without manifest cardiovascular disease) (Fig. 1 ) [1].
Lifestyle changes including weight reduction
In patients with obesity and T2DM, weight reduction is one of the cornerstones of treatment. Weight loss of >5% improves glycemic control, lipid levels and blood pressure in overweight and obese adults with T2DM. These effects can be achieved by improving the energy balance and/or introducing obesity medication. Orlistat, naltrexone/bupropion and phentermine/topiramate are each associated with a weight loss of more than 5% at 52 weeks compared to placebo. However, glucose-lowering agents such as GLP-1 RAs, the dual agonist tirzepatide and SGLT2 inhibitors also significantly reduce body weight. Exercise in addition to a GLP-1 RA (liraglutide) had a greater effect on weight loss and maintenance.
Regular moderate to vigorous physical activity has a beneficial effect on metabolic control and cardiovascular disease risk factors in T2DM. Intervention programs reduce HbA1c by 0.6% in patients with T2DM, with the combination of endurance and resistance training having the most beneficial effects. In addition, high physical activity is associated with a lower risk of cardiovascular mortality and a reduction in all-cause mortality compared to low physical activity (all-cause mortality: HR 0.60 [95% CI, 0.49-0.73]).
Smoking cessation is an equally important lifestyle intervention in patients with T2DM with or without CVD. There is evidence that mortality in CVD patients can be reduced by 36%. If counseling, encouragement and motivation are not enough, drug therapies should be considered early on, including nicotine replacement therapy (gum, transdermal nicotine patches, nasal spray, inhaler, sublingual tablets) followed by bupropion. Electronic cigarettes (e-cigarettes) have been considered as a potential smoking cessation aid to bridge the transition from smoking to abstinence, but should only be used for a short period of time.
Reducing the risk of atherosclerotic cardiovascular disease in diabetes
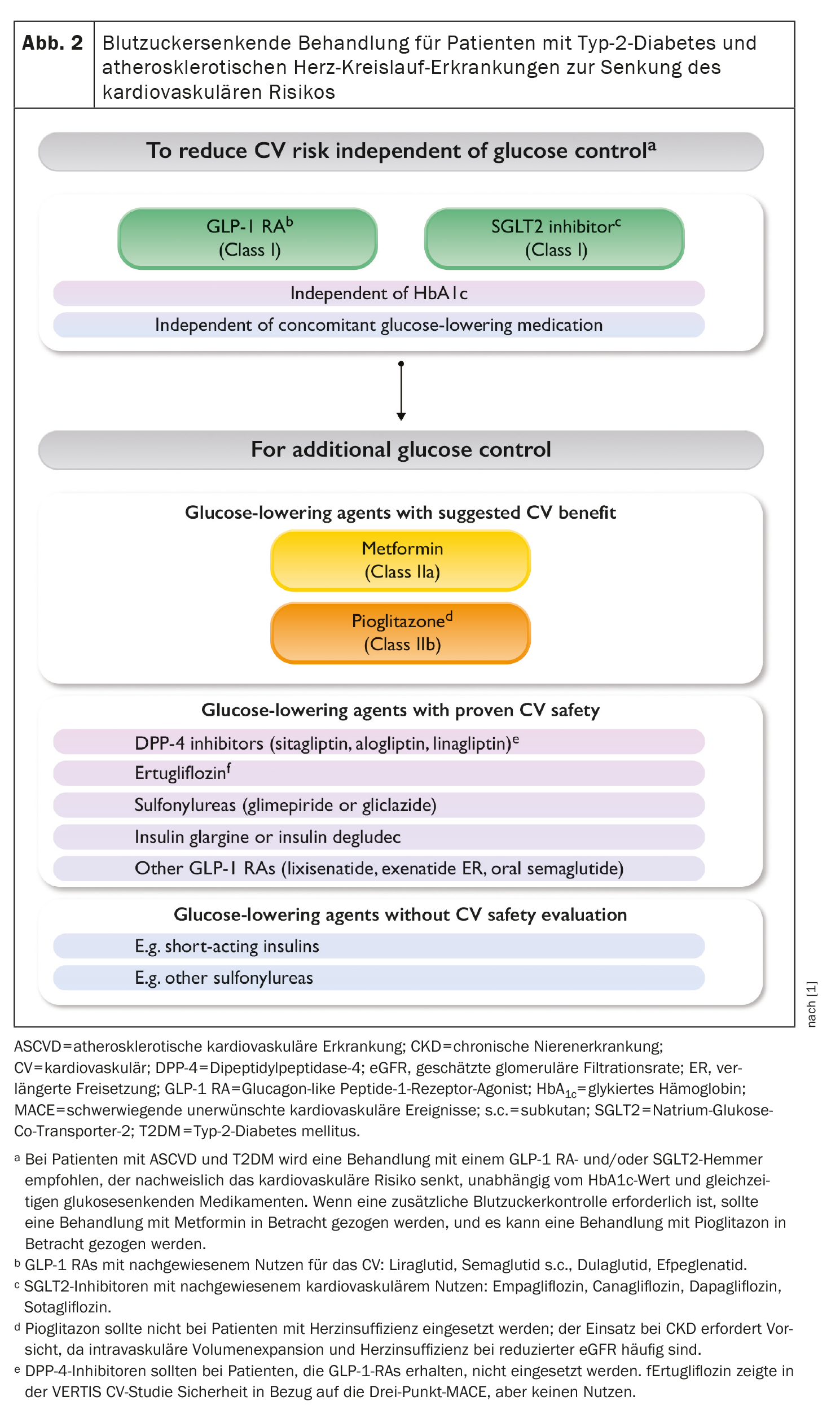
T2DM is common in patients with atherosclerotic cardiovascular disease (ASCVD) or at the highest risk of CVD. The reverse is also true: ASCVD often occurs in patients with T2DM. Given these relationships, it is critical to consider the presence of T2DM when deciding on strategies to mitigate CV risk. The first step in this process must be to screen all patients with CVD for T2DM. Many decisions are independent of glucose management, so T2DM status can inform clinical decision making to reduce cardiovascular risk. Based on the results of several dedicated cardiovascular outcomes trials (CVOTs) regarding glucose-lowering medications in patients with diabetes and ASCVD or high cardiovascular risk, there is now a wealth of data to support the preferential use of selected glucose-lowering medications to reduce cardiovascular risk independent of glucose management considerations.
It is recommended to prioritize the use of antihyperglycemic agents with proven cardiovascular benefits, followed by agents with proven cardiovascular safety (such as empagliflozin, canagliflozin, dapagliflozin, sotagliflozin, liraglutide, semaglutide s.c., dulaglutide, efpeglenatide) versus agents with no proven CV benefit (such as metformin, pioglitazone, DPP-4 inhibitors, glimepiride, gliclazide, insulin glargine, insulin degludec, ertugliflozin, lixisenatide, exenatide, oral semaglutide) or proven CV safety. If additional glycemic control is required, metformin should be considered in patients with T2DM and ASCVD. Pioglitazone can be considered in patients with T2DM and ASCVD without HF (Fig. 2) [1].
Blood pressure and diabetes
Regular blood pressure measurements are recommended for all patients with diabetes to detect and treat high blood pressure and reduce cardiovascular risk (Class IA recommendation).
Lipids and diabetes
A PCSK9 inhibitor is recommended in patients at very high cardiovascular risk whose LDL-C levels remain above target despite treatment with a maximum tolerated statin dose in combination with ezetimibe, or in patients with statin intolerance (class IA recommendation). If the target LDL-C value is not achieved with statins, combination therapy with ezetimibe is recommended. If statin treatment is not tolerated at any dose (even after repeated treatment), a PCSK9 inhibitor should be considered in addition to ezetimibe. If a statin-based regimen is not tolerated at any dose (even after retreatment), ezetimibe should be considered. In patients with hypertriglyceridemia, high-dose icosapent ethyl (2 g b.i.d.) in combination with a statin may be considered.
Antithrombotic therapy and diabetes
Clopidogrel 75 mg o.d. after appropriate loading (e.g. 600 mg or at least five days already on maintenance therapy) is recommended in addition to ASA for six months after coronary stenting in patients with CCS, regardless of stent type, unless a shorter duration is indicated due to the risk or occurrence of life-threatening bleeding (Class IA recommendation). In patients with diabetes and ACS treated with DAPT who undergo CABG and do not require long-term OAC therapy, it is recommended to restart a P2/12 receptor inhibitor as soon as deemed safe after surgery and continue for up to 12 months. In addition, the addition of very low-dose rivaroxaban to low-dose ASA should be considered for the long-term prevention of serious vascular events in patients with diabetes and CCS or symptomatic PAD without a high risk of bleeding.
In patients with ACS or CCS and diabetes undergoing coronary stent implantation who have an indication for anticoagulant prolonged triple therapy with low-dose ASA, clopidogrel and an OAC, up to 1 month of use should be considered if the risk of thrombosis outweighs the patient’s risk of bleeding. In patients with ACS or CCS and diabetes who are undergoing coronary stent implantation and for whom there is an indication for anticoagulation, an extension of triple therapy with low-dose ASA, clopidogrel and an OAC for up to three months may be considered if the risk of thrombosis outweighs the patient’s risk of bleeding. When using clopidogrel, omeprazole and esomeprazole are not recommended to protect the stomach.
Multifactorial approach to risk factor management in diabetes
Early detection and treatment of risk factors and comorbidities is recommended at an early stage (Class IA recommendation). Multidisciplinary behavioral approaches that combine the knowledge and skills of different caregivers are recommended. The principles of motivational interviewing should be taken into account in order to bring about changes in behavior. Telemedicine can be considered to improve the risk profile.
Treatment of coronary heart disease in diabetes
Myocardial revascularization in CCS is recommended if angina persists despite treatment with antianginal drugs or in patients with documented large area ischemia (>10% LV). In patients with STEM without cardiogenic shock and with multivessel CHD, complete revascularization is recommended (Class IA recommendation). Furthermore, it is recommended that the glycemic status of all patients with ACS be determined during the initial examination. In patients with NSTE-ACS without cardiogenic shock and with multivessel CHD, complete revascularization should be considered. In ACS patients with persistent hyperglycemia, blood glucose-lowering therapy should be considered, while episodes of hypoglycemia should be avoided. Routine immediate revascularization of non-main lesions in patients with MI and multivessel disease who have cardiogenic shock is not recommended.
Heart failure and diabetes
If heart failure (HF) is suspected, the measurement of BNP/NT-proBNP is recommended. In principle, systematic screening for HF symptoms and/or signs of HF is recommended at every clinical encounter in all patients with diabetes.
The following diagnostic tests are recommended in all patients with suspected heart failure: 12-lead ECG, transthoracic echocardiography, chest X-ray and routine blood tests for comorbidities, including full blood count, urea, creatinine and electrolytes, thyroid function, lipids and iron status (ferritin and TSAT).
Pharmacological treatment is indicated in patients with HFrEF (NYHA class II-IV) and diabetes: SGLT2 inhibitors (dapagliflozin, empagliflozin or sotagliflozin) are recommended in all patients with HFrEF and TDM to reduce the risk of heart failure hospitalization and cardiovascular death (class IA recommendation). An intensive strategy of early initiation of evidence-based treatment (SGLT2 inhibitors, ARNI/ACE-Is, beta-blockers and MRAs) with rapid up-dosing to study-defined target doses prior to discharge and with frequent follow-up in the first six weeks after HF hospitalization is recommended to reduce readmissions or mortality.
Further treatment is indicated in selected patients with HFrEF (NYHA class II-IV) and diabetes: Hydralazine and isosorbide dinitrate should be considered in “person of color” with diabetes and an LVEF ≤35% or with an LVEF <45% in combination with a dilated LV in NYHA class II-IV despite treatment with an ACE-I (or ARNI), a beta-blocker, and an MRA to reduce the risk of HF hospitalization and death. Digoxin may be considered in patients with symptomatic HFrEF in sinus rhythm despite treatment with sacubitril/valsartan or an ACE-I, a beta-blocker and an MRA to reduce the risk of hospitalization.
Treatment of heart failure in patients with diabetes and LVEF >40%: Empagliflozin or dapagliflozin are recommended in patients with T2DM and LVEF >40% (HFmrEF and HFpEF) to reduce the risk of HF hospitalization or CV death (Class IA recommendations).
Special considerations for glucose-lowering medications in patients with T2DM with and without HF: It is recommended that treatment to lower blood glucose levels be switched from agents with no proven cardiovascular benefit or safety to agents with proven quality of life benefits.
| The care of patients with diabetes and cardiovascular disease requires an interdisciplinary approach that should involve healthcare professionals from different disciplines and specialties. The aim is to support joint decision-making processes and implement a patient-centered and personalized treatment strategy in order to reduce the disease burden of each individual patient and improve prognosis. |
Atrial fibrillation and diabetes
Opportunistic screening for atrial fibrillation by pulse measurement or ECG is recommended in patients with diabetes under the age of 65 (especially if other risk factors are present), as patients with diabetes are more likely to have atrial fibrillation at a younger age. Systematic ECG screening should be considered to detect atrial fibrillation in patients aged ≥75 years or at high risk of stroke.
Chronic kidney disease and diabetes
Intensive LDL-C lowering with statins or a combination of statin and ezetimibe combination is recommended. An SGLT2 inhibitor (canagliflozin, empagliflozin or dapagliflozin) is recommended in patients with T2DM and CKD with an eGFR ≥20 mL/min/1.73m2 to reduce the risk of CVD and renal failure. Finerenone is recommended in addition to an ACE-I or ARB in patients with T2DM and an eGFR >60 mL/ min/1.73m2 with a UAC ≥30 mg/mmol (≥2300 mg g) or eGFR 25-60 mL/min/1.73m2 and UACR ≥3 mg/mmol (≥30 mg/g) to reduce cardiovascular events and renal failure. Low-dose ASA (75-100 mg per day) is recommended for patients with CKD and ASCVD (class IA recommendation).
Based on similar results, intensive medical treatment or an initial invasive strategy is recommended for people with CKD, diabetes and stable moderate or severe CHD. The advice of a renal specialist may be considered for the treatment of elevated serum phosphate levels, other evidence of CKD-MBD and renal anemia. However, the combined use of an ARB with an ACE-I is not recommended.
Aortic and peripheral arterial diseases and diabetes
In patients with diabetes and aortic aneurysm, it is recommended to apply the same diagnostic measures and therapeutic strategies (medical, surgical or endovascular) as in patients without diabetes.
Type 1 diabetes (T1DM) and cardiovascular disease
For patients with T1DM, it is recommended that the adjustment of blood glucose-lowering medication follows the principles of patient self-management under the guidance of the multidisciplinary diabetes health team. It is recommended to avoid hypoglycemic episodes, especially in patients with existing cardiovascular disease. Statins should be considered for LDL-C lowering in adults over 40 years of age with T1DM without a history of cardiovascular disease to reduce cardiovascular risk. In adults under 40 years of age with T1DM, statins and other risk factors for cardiovascular disease or microvascular end-organ damage or a 10-year CVD risk of ≥10% should be considered to reduce cardiovascular risk. Similarly, the use of the Scottish-Swedish risk prediction model can be considered to estimate the 10-year CVD risk in patients with T1DM.
Source:
- Marx N, et al: 2023 ESC Guidelines for the management of cardiovascular disease in patients with diabetes: Developed by the task force on the management of cardiovascular disease in patients with diabetes of the European Society of Cardiology (ESC). European Heart Journal, Volume 44, Issue 39, October 14, 2023, Pages 4043-4140; https://doi.org/10.1093/eurheartj/ehad192.
CARDIOVASC 2023, 22(4): 52-55 (published on 28.11.23, ahead of print)