Cutaneous symptoms, along with articular involvement, are among the most common organ involvement of systemic lupus erythematosus (SLE). In addition to positive ANA findings, further antibodies are indicative for laboratory diagnosis. If patients are suspected of having CLE, the CLASI can be used – a validated short test procedure to assess disease activity. Histological detection is obligatory to confirm the suspected clinical diagnosis; direct immunofluorescence or photoprovocation tests are used less frequently.
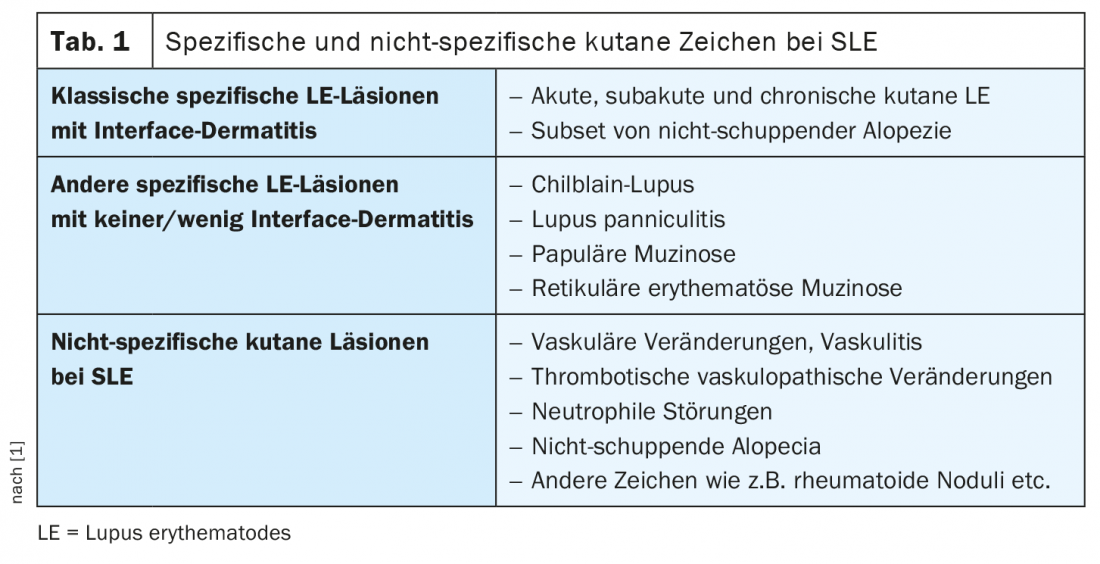
The fact that a variety of specific and non-specific cutaneous changes can be associated with systemic lupus erythematosus (SLE) (Table 1) is a challenge, according to Prof. Luca Borradori, MD, Chief of Medicine, University Department of Dermatology, Inselspital Bern [1]. To rule out extracutaneous involvement, laboratory tests – including antinuclear antibodies (ANA), renal function tests, and antiphospholipid antibodies – are indicated in addition to history and clinical inspection. In about 10-15% of cases, cutaneous lupus erythematosus (CLE) is the first manifestation of SLE. Patients should be educated about this, the speaker emphasized. Patient education is generally important in CLE patients, he said. As a diagnostic tool for the first or second consultation, the test procedure “CLASI” (“The Cutaneous Lupus Erythematosus Disease Area and Severity Index”), which can be performed within a few minutes, is suitable. This validated clinical score captures the presence of erythema, scaling, and hypertrophy on the one hand, and dyspigmentation, scarring, or atrophy on the other.
Histopathological examination – what to consider?
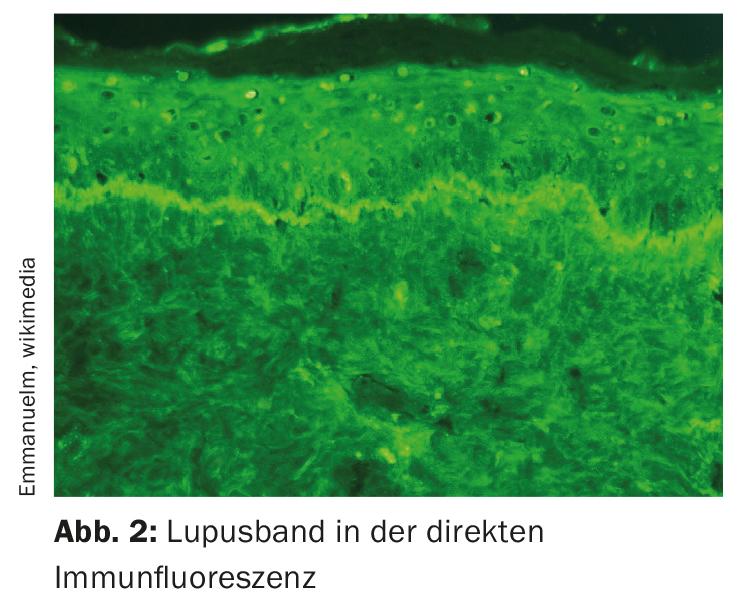
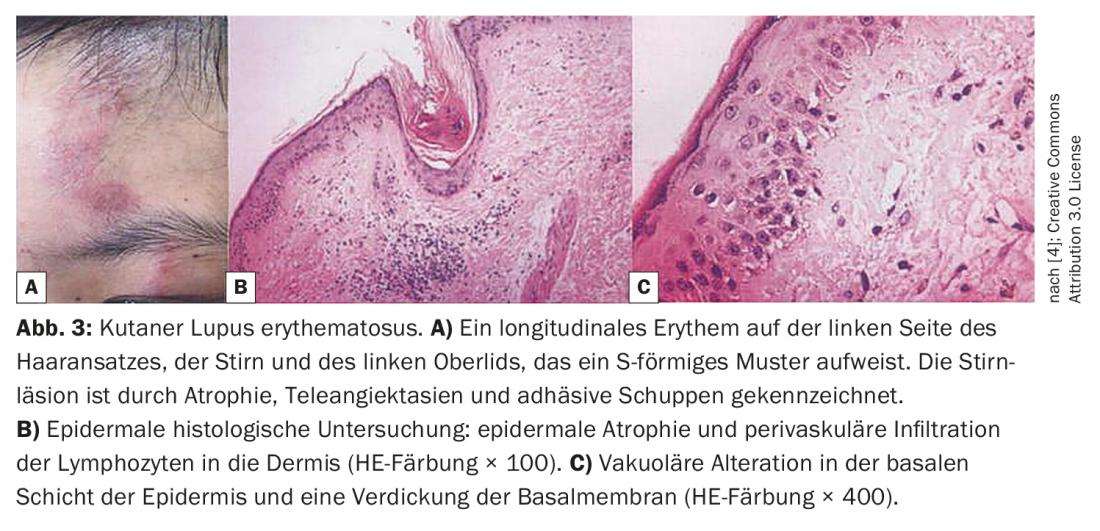
If the clinical workup supports a diagnosis of CLE, histologic evaluation should be performed for confirmation – of both typical and atypical lesions. One finds either interface dermatitis or vacuolar degeneration of the basal cell layer, or lymphocytic and perivascular inflitrate. It should be remembered that there is also CLE without particular involvement of the dermo-epidermal junction zone, respectively without interface dermatitis, explains Prof. Borradori [1]. This applies, for example, to panniculitis or chilblain’s lupus and, of course, also to lupus tumidus, which is accompanied only by lymphocytic infiltrates. Direct immunofluorescence is now only done when the diagnosis of CLE is unclear. As an example, the speaker mentioned certain cases of scarring alopecia in which it is extremely difficult to distinguish between lichen and lupus. For these special cases, immunofluorescence could be very helpful. Photoprovocation testing is another procedure that is occasionally used in diagnostic workups for CLE. In about 60% of cases, this could be used to detect photosensitivity in lupus patients.
Laboratory controls – which parameters to determine and how often?
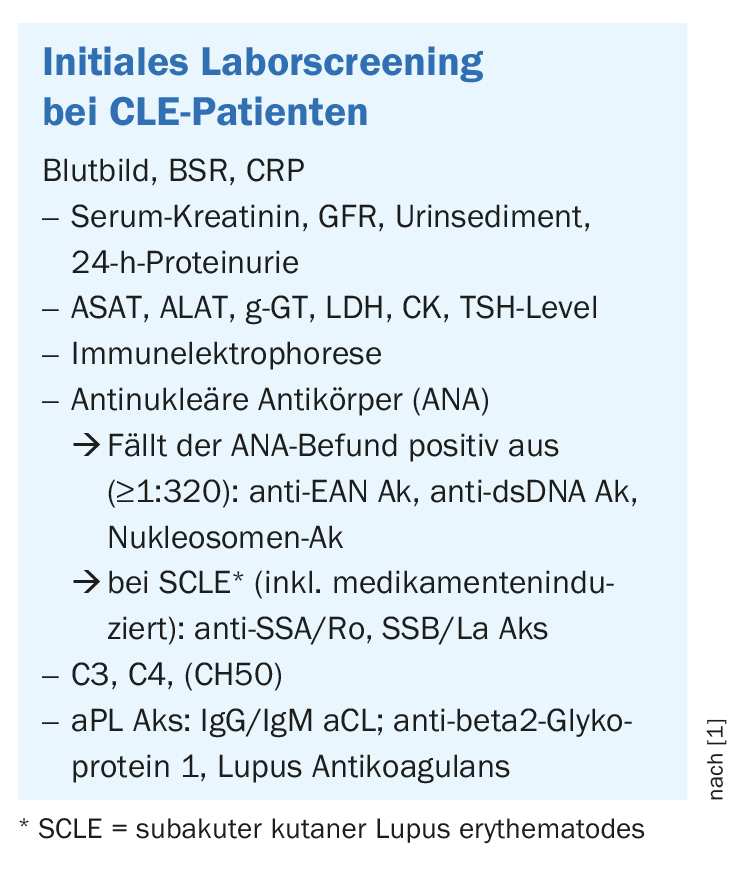
If there is evidence of possible cutaneous lupus erythematosus in patients, the initial laboratory measurements shown in the box are recommended to better assess possible organ involvement and to identify patients at increased risk for developing systemic lupus erythematosus [1]. If the ANA result is positive, the titers are often low (≤1:320). Anti-ds DNA and anti-Sm abs are not characteristic of CLE but are mostly associated with SLE. It is also important to determine the following antiphospholipid antibodies (Ak): Anti-Cardiolipin-Ak IgG/IgM, Beta-2-Glycoprotein-Ak, Lupus Anticoagulans-Ak. These are also mentioned in the SLE classification criteria of the ACR/SLICC/EULAR. In CLE, only about 5% are positive, but it is important to look for these antibodies because these patients are at increased risk for cerebrovascular insults, thrombotic complications, or heart valve problems, the speaker stressed. In addition, patients with CLE/SLE and antiphospholipid antibodies should not take estrogen-containing anticontraceptives. There is no evidence-based recommendation on the frequency of laboratory checks during the course, Prof. Borradori said. His advice on this is to perform laboratory testing at least once a year even in patients with mild and limited CLE symptoms. In those patients with high disease activity and additional symptoms, determination of the following laboratory parameters during the course is generally recommended [1]:
- Small blood count, blood sedimentation, creatinine, glomerular filtration rate (GFR), urinalysis, proteinuria, C3, C4.
- anti-ANA, anti-ds DNA, ENA Screen
- in the case of certain drug therapies: possibly further laboratory tests
- depending on the patient’s history and clinical features: possibly further hemotological, renal, cardiopulmonary, neurological, musculoskeletal investigations
What are warning signs of developing SLE?
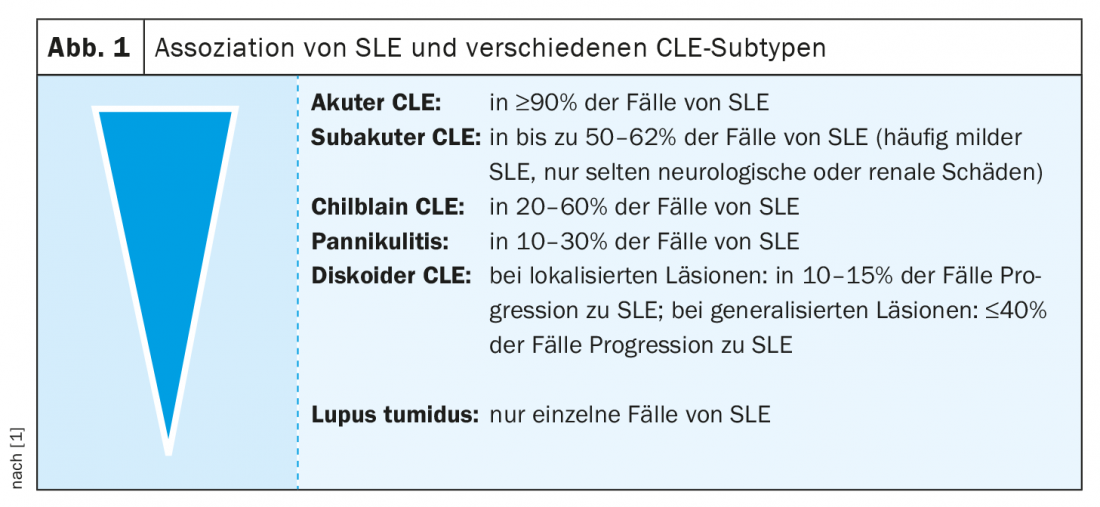
Indications of potential progression toward SLE include CLE patients who have arthralgias/arthritis or when signs of anemia, greatly increased inflammatory parameters, blood count changes, or high ANA titers are present. “These are usually warning signs,” summarizes Prof. Borradori [1]. The risk for SLE depends, among other factors, on the subtype of CLE (Fig. 1). When butterfly erythema is a manifestation of acute CLE, the risk of progression to SLE is relatively high. Panniculitis is diagnosed in 10-30% of cases during the course of SLE. If the skin changes are localized and only one region of the body is affected, for example the face, the risk is relatively low. Thus, in discoid CLE, the probability of developing SLE within the next 5 to 10 years is approximately 10-15%. “Lupus tumidus is virtually never associated with SLE,” the speaker added.
What prophylactic measures are recommended?
UV radiation is considered one of the most important trigger factors of lupus erythematosus [2]. Therefore, lupus patients should protect themselves from the sun, especially during the spring and summer months. This includes the use of sunscreen products with a high sun protection factor. Vitamin D supplementation is recommended for all CLE patients [3]. Since smoking is a risk factor for the development of SLE and aggravation of cutaneous lesions, smoking cessation is advised. Regarding vaccinations, experts suggest that especially elderly patients should be vaccinated against pneumococcus and influenza. Varicella zoster vaccination should also be considered for those over 50 years of age. A medication history is advisable in all patients with subacute or acute lupus. Drug-induced lupus may resolve after discontinuation of the drug.
Congress: SwissDermaDay
Literature:
- Borradori L: Cutaneous lupus erythematosis (CLE): diagnosis and practical monitoring. Prof. Dr. med. Luca Borradori, SwissDermaDays, 13.01.2022.
- Kuhn A, Beissert S. Photosensitivity in lupus erythematosus. Autoimmunity 2005; 38(7): 519-529.
- Cutillas-Marco E, et al: Vitamin D and cutaneous lupus erythematosus: effect of vitamin D replacement on disease severity. Lupus 2014; 23(7): 615-623.
- Xin R, et al: Lupus Erythematosus: Dermatologic Perspectives on the Diversity, August20th, 2019, DOI: 10.5772/intechopen.88446.
DERMATOLOGY PRACTICE 2022; 32(1): 38-39