Carpal tunnel syndrome is the most common nerve constriction syndrome. The diagnosis can often be made clinically with a focused history and neurologic examination. To assess nerve function as well as the extent of nerve damage, electrophysiology is the gold standard in the diagnosis of CTS. Nerve ultrasound is an excellent complementary technique to visualize morphologic changes of the median nerve in the carpal tunnel region. Various sonographic parameters, such as nerve cross-sectional area, nerve structure, vascularization, and mobility of the median nerve, can be used to support the diagnosis of CTS. In addition, nerve ultrasound can provide important additional information about compression localization and causes.
Carpal tunnel syndrome (CTS) is the most common nerve constriction syndrome in clinical practice. The lifetime prevalence of developing CTS is 1-3% and peaks around the age of 50, with women being ten times more likely to develop the disease than men. Early diagnosis is important because effective treatment options are available to prevent permanent nerve damage.
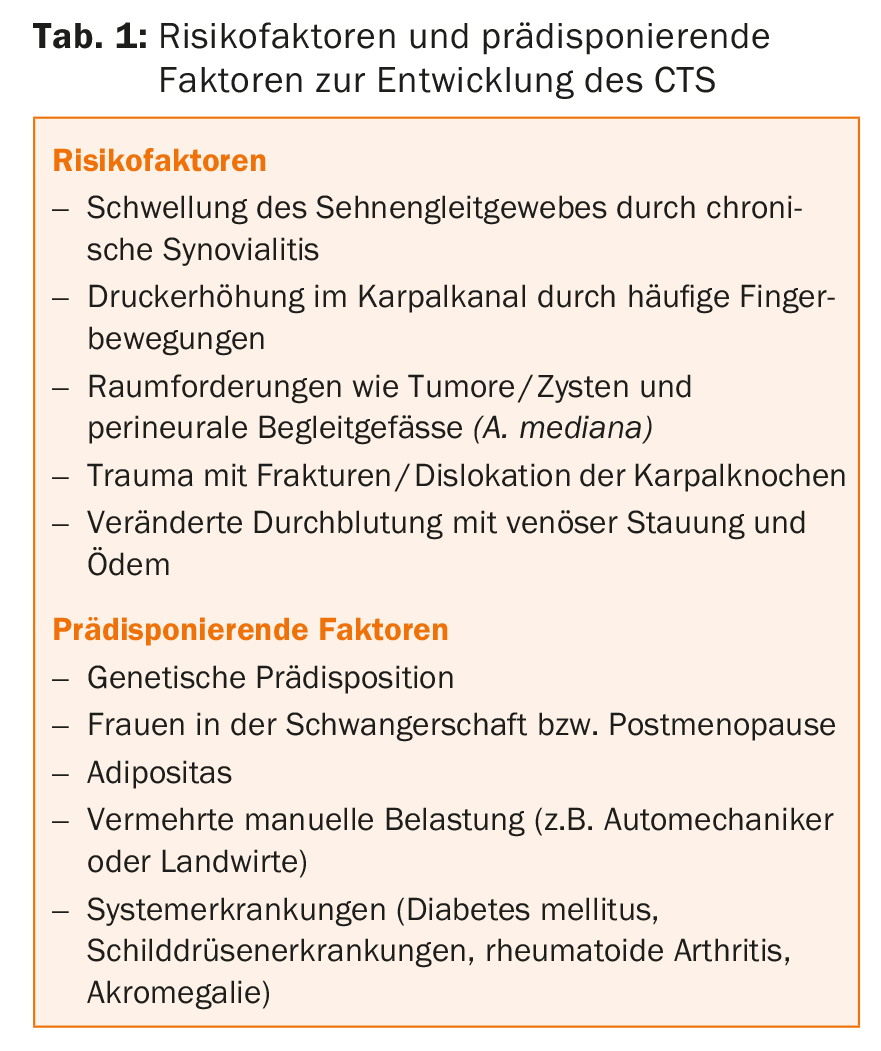
The median nerve lies in the carpal canal between the retinaculum flexorum, the tendons of the hand flexors and the carpal bones. Because of its close proximity, the median nerve is highly susceptible to acute and chronic compression. The exact pathomechanism for the development of classic CTS is unknown, but many promoting factors and risk factors are discussed (Tab. 1) . The common hypothesis describes a combination of ischemic changes and mechanical compression with damage to the myelin sheath and ultimately the axon.
Symptoms of carpal tunnel syndrome
The diagnosis of CTS can often be made clinically based on history and neurologic examination. In the foreground are paresthesias of the thumb, index and middle finger (brachialgia paraesthetica nocturna) and pain radiating into the fingers as well as a feeling of swelling. Especially at the beginning of the disease, the extent of the symptoms does not correlate with the nerve damage, since initially the sensory and autonomic fibers are impaired. As the disease progresses, permanent sensory disturbances and paresis of the muscle groups supplied by the median nerve occur. Thenaratrophy in the final stage is an expression of severe axonal nerve damage. Clinical provocation tests such as the phalen test or Hoffmann-Tinel sign can help confirm the diagnosis of carpal tunnel syndrome, but are neither very sensitive nor specific.
Electrophysiology – the gold standard in the diagnosis of CTS
Electrophysiology can confirm the suspected clinical diagnosis of CTS, objectify the extent of nerve damage, and exclude some, although not all, differential diagnoses. It is the gold standard in the diagnosis of CTS. The motor conduction time (“distal motor latency” [DML]) of the median nerve during stimulation of the nerve at the wrist and conduction via the abductor pollicis brevis muscle is sensitive in this regard. A DML >4.2 ms is considered pathological, with normal values varying with respect to age, weight, and sex. Comparative motor and sensory measurements across the wrist of the median nerve to a nerve that does not pass through the carpal tunnel-most commonly the ulnar nerve-can be helpful, especially in mild clinical courses. In the diagnosis of CTS, electrophysiology has a specificity up to 98%, with a sensitivity around 85% [1]. However, in 10-20% of patients with clinically definite symptoms of CTS, electrophysiology may be unremarkable. Therefore, normal electroneurography cannot exclude the presence of CTS.
The role of nerve ultrasound
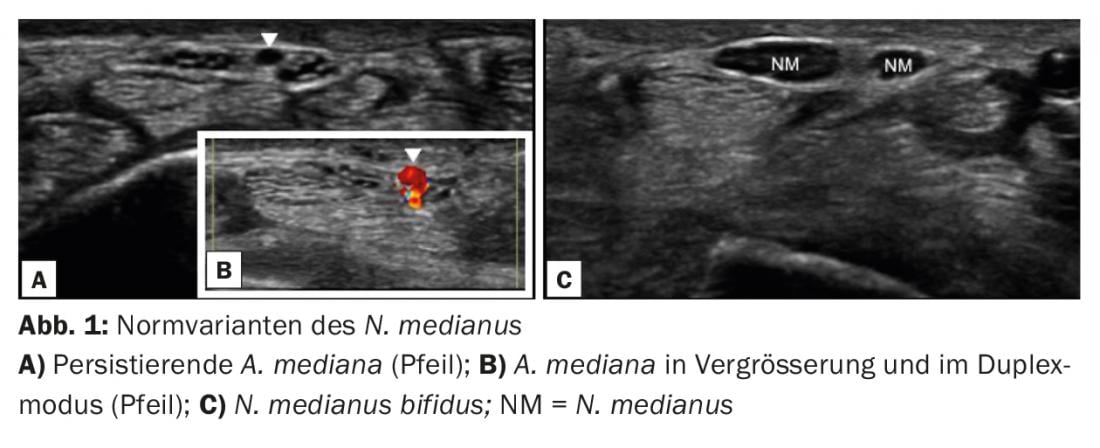
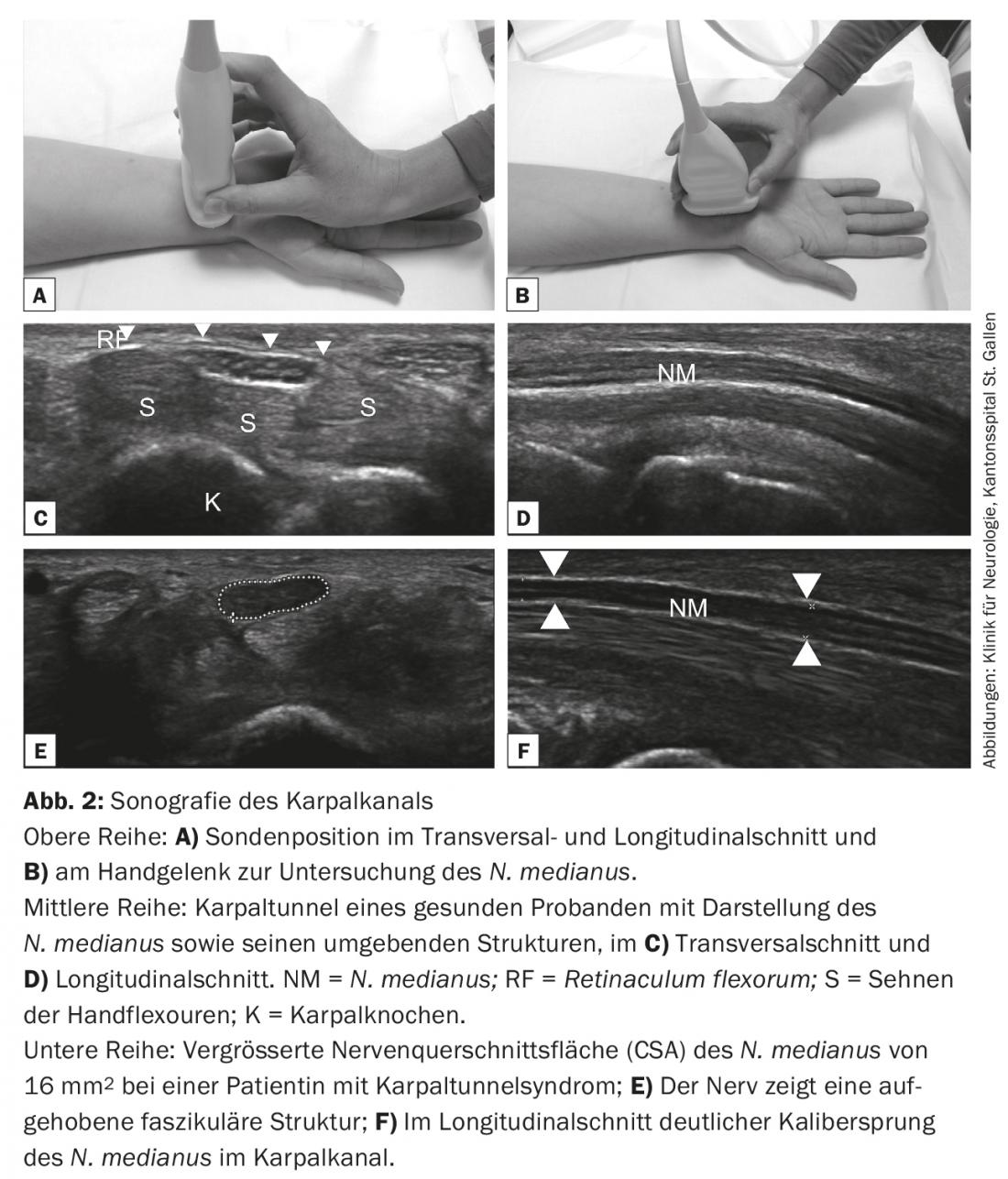
As an important noninvasive procedure, nevenultrasound is an excellent complementary method to visualize morphologic changes of the median nerve in the carpal tunnel region. A high-resolution “linear array” probe with a transmission frequency of 12 MHz or higher (16-18 MHz is better) is suitable for this purpose in order to be able to optimally visualize the nerve structures. Nerve ultrasound offers many complementary advantages as a brief, painless examination and can visualize a variety of median n erve parameters such as size, vascularization (in duplex mode), and mobility (dynamic examination/film). It can provide important additional information about compression localization and causes. Anatomic variants (bifid median nerve, accompanying median artery, Fig. 1) as well as surrounding tissue (ganglia, cysts, tumors, aberrant muscles, inflammation) can also be visualized. Electrophysiology as a functional examination method does not provide this information.
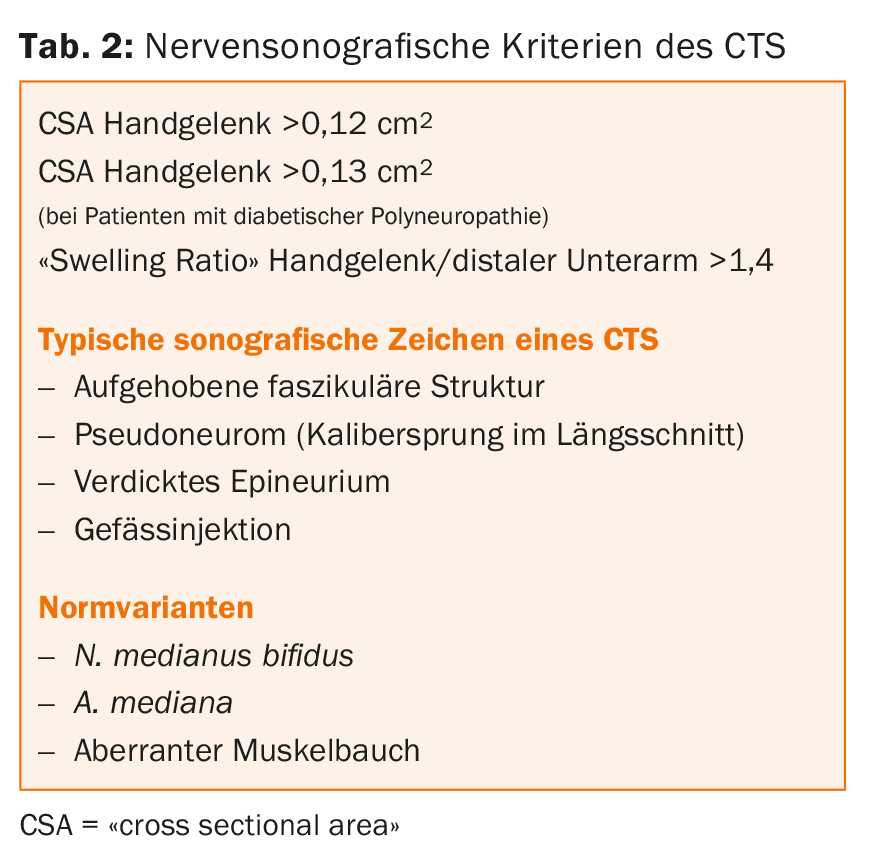
Sonographic criteria of carpal tunnel syndrome
On nerve ultrasound of the wrist, the median nerve can be easily visualized in transverse section: it appears honeycombed with hypoechogenic nerve fibers surrounded by a hyperechogenic epineurium. Here, it lies superficially over the tendons of the hand flexors; the retinaculum flexorum as a hyperechogenic structure above it. In longitudinal section, the nerve can be imaged in its entire course through the carpal tunnel. When using a high-resolution probe, it can be followed deep into the palm (Fig. 2A-D) . There are now a large number of studies that have investigated suitable parameters for the diagnosis of CTS. It has been shown that the transverse nerve sectional area (“cross sectional area” [CSA]) of the median nerve is significantly larger in patients with clinical symptoms of CTS compared to healthy controls [2]. The nerve also appears hypoechogenic due to the swelling and loses its honeycomb fascicular structure (Fig. 2E) [3]. There is no agreement in the literature about the CSA reference values and the localization of the most suitable measurement site. This is due to the use of different ultrasound transmission frequencies and devices. Recommended reference values vary between 6.5 and 15 mm2. Most studies showed the best sensitivity and specificity of CSA measurement at the level of the os pisiforme, or the carpal tunnel inlet. In clinical practice, from our experience, measuring the maximum CSA of >12 mm2 in the course of the carpal tunnel has proven to be a good parameter to reliably diagnose CTS. In various studies, this parameter has both a specificity of 100% and a good sensitivity [4,5]. On the other hand, a CSA <9.0 mm2 excludes a CTS with high probability [6]. The CSA is measured within the hyperechogenic epineurium. If the CSA is borderline elevated, the swelling ratio may be helpful by a comparative measurement between the wrist and distal forearm. A ratio above >1.4 is considered pathological here [7]. This relative measurement method is also suitable for validating the absolute measured values. Other parameters such as a thickened epineurium or increased vascular injections may be helpful; however, the relevance and sensitivity of these abnormalities have not been clarified [8]. In longitudinal section, a clear caliber jump (pseudoneuroma) can be seen in compression of the nerve as an expression of intraneural edema proximal to the compression zone (Fig. 2F) . The combination of different nerve sonographic parameters improves the diagnostic certainty for the presence of CTS. The probability of CTS increases from 35 to up to 90% when three parameters (CSA, hypoechogenicity, hypervascularization) are combined for assessment [9]. Furthermore, the continuous increase in CSA correlates well with the clinical severity of CTS [10]. Table 2 summarizes the sonographic criteria of CTS.
Correlation of nerve ultrasound to electrophysiology.
Different studies have investigated the diagnostic acuity of nerve ultrasound compared with electrophysiology of CTS. Here, CSA in particular shows good correlation with electrophysiology for assessing severity [11]. However, patients with pathologic electrophysiology may have unremarkable nerve ultrasound findings, as well as vice versa. Especially in patients with a short duration of CTS symptoms and only mild compression, nerve ultrasound may be unremarkable [12].
Carpal tunnel syndrome in patients with diabetes mellitus
CTS occurs more frequently in patients with diabetes mellitus. Due to impaired glucose metabolism, peripheral nerves are particularly vulnerable to compression at physiological constriction sites. About 14% of patients with diabetes mellitus and about 30% of patients who also have diabetic polyneuropathy develop CTS [13]. Because of an underlying polyneuropathy, clinical as well as electrophysiologic diagnosis of CTS can be difficult. Nerve ultrasound, with an enlargement of the CSA of the median nerve in the wrist of >13 mm2, indicates CTS in patients with diabetes mellitus with good sensitivity and specificity [14].
Strengths and weaknesses of nerve ultrasound
Nerve ultrasound offers the possibility of easily and quickly visualizing morphological changes as well as normal variants of the nerve and compressive structures. On the one hand, this is helpful for the etiological classification of CTS, and on the other hand, it also provides valuable information for the surgeon. Generalized pathologic nerve changes, such as those seen in hereditary or acquired demyelinating neuropathies, can be visualized and contribute to differential diagnosis. Furthermore, nerve ultrasound can be very useful in complicated therapy and in recurrences of CTS. Sonographically, incomplete transection of the retinaculum flexorum as well as proliferating scar tissue can be demonstrated as the cause of persistent symptoms [15]. However, the electrophysiological parameters as well as the CSA normalize postoperatively only slowly [16]. Nerve ultrasonography is also suitable for the examination of children or other groups of patients who do not tolerate the painful examination in electrophysiology, as well as in mutilated extremities, such as those found in rheumatologic diseases, and where the differentiation between compression and inflammation in the context of tendinitis is important (Fig. 3).

However, a statement about nerve function and the extent of nerve damage, as well as the differential diagnosis of C6/C7 radiculopathy, underlying polyneuropathy, or a proximal lesion of the median nerve, remains the domain of electrophysiology. Thus, in summary, both examination methods provide important, complementary information in the evaluation and diagnosis of CTS, in addition to history and clinical information.
Literature:
- American Association of Electrodiagnostic Medicine, American Academy of Neurology, and American Academy of Physical Medicine and Rehabilitation: Practice parameter for electrodiagnostic studies in carpal tunnel syndrome: summary statement. Muscle Nerve 2002; 25(6): 918-922.
- Sernik RA, et al: Ultrasound features of carpal tunnel syndrome: a prospective case-control study. Skeletal Radiol 2008; 37(1): 49-53.
- Cartwright MS, et al: Neuromuscular ultrasound in common entrapment neuropathies. Muscle Nerve 2013; 48(5): 696-704.
- Ziswiler HR, et al: Diagnostic value of sonography in patients with suspected carpal tunnel syndrome: a prospective study. Arthritis Rheum 2005; 52(1): 304-311.
- Nakamichi KI, et al: Enlarged median nerve in idiopathic carpal tunnel syndrome. Muscle Nerve 2000; 23(11): 1713-1718.
- Mhoon JT, et al: Median nerve ultrasound as a screening tool in carpal tunnel syndrome: Correlation of cross-sectional area measures with electrodiagnostic abnormality. Muscle Nerve 2012; 46(6): 861-870.
- Hobson-Webb LD, et al: The ultrasonographic wrist-to-forearm median nerve area ratio in carpal tunnel syndrome. Clinical Neurophysiology 2008; 119(6): 1353-1357.
- Vanderschueren GAKB, et al: Doppler sonography for the diagnosis of carpal tunnel syndrome: A critical review. Muscle Nerve 2014; 50(2): 159-163.
- Rahmani M, et al: The ultrasonographic correlates of carpal tunnel syndrome in patients with normal electrodiagnostic tests. Radiol Med 2011; 116(3): 489-496.
- Roll SC, et al: Carpal tunnel syndrome severity staging using sonographic and clinical measures. Muscle Nerve 2015; 51(6): 838-845.
- Visser LH, et al: High-resolution sonography versus EMG in the diagnosis of carpal tunnel syndrome. Journal of Neurology, Neurosurgery & Psychiatry 2008; 79(1): 63-67.
- Chen SF, et al: Ultrasonographic median nerve cross-section areas measured by 8-point “inching test” for idiopathic carpal tunnel syndrome: a correlation of nerve conduction study severity and duration of clinical symptoms. BMC Med Imaging 2011; 11(1): 22.
- Perkins BA, et al: Carpal tunnel syndrome in patients with diabetic polyneuropathy. Diabetes Care 2002; 25(3): 565-569.
- Tsai NW, et al: The diagnostic value of ultrasonography in carpal tunnel syndrome: a comparison between diabetic and non-diabetic patients. BMC Neurol 2013; 13(1): 1373.
- Kapuścińska K, et al: Efficacy of high frequency ultrasound in postoperative evaluation of carpal tunnel syndrome treatment. J Ultrason 2016; 16(64): 16-24.
- Lee CH, et al: Postoperative morphologic analysis of carpal tunnel syndrome using high-resolution ultrasonography. Ann Plast Surg 2005; 54(2): 143-146.
InFo NEUROLOGY & PSYCHIATRY 2016; 14(6): 12-15.