At the Update Refresher General Internal Medicine, Michael Andor, MD, Center for Spine Medicine PRODORSO, Zurich, gave an overview of the most important diseases in rheumatology. When a patient complains of joint pain, it is important to distinguish between inflammatory and degenerative causes – resp. between diseases that require emergency treatment and those for which one can take some time – not always easy in practice. This makes it all the more crucial to memorize the most important engrams.
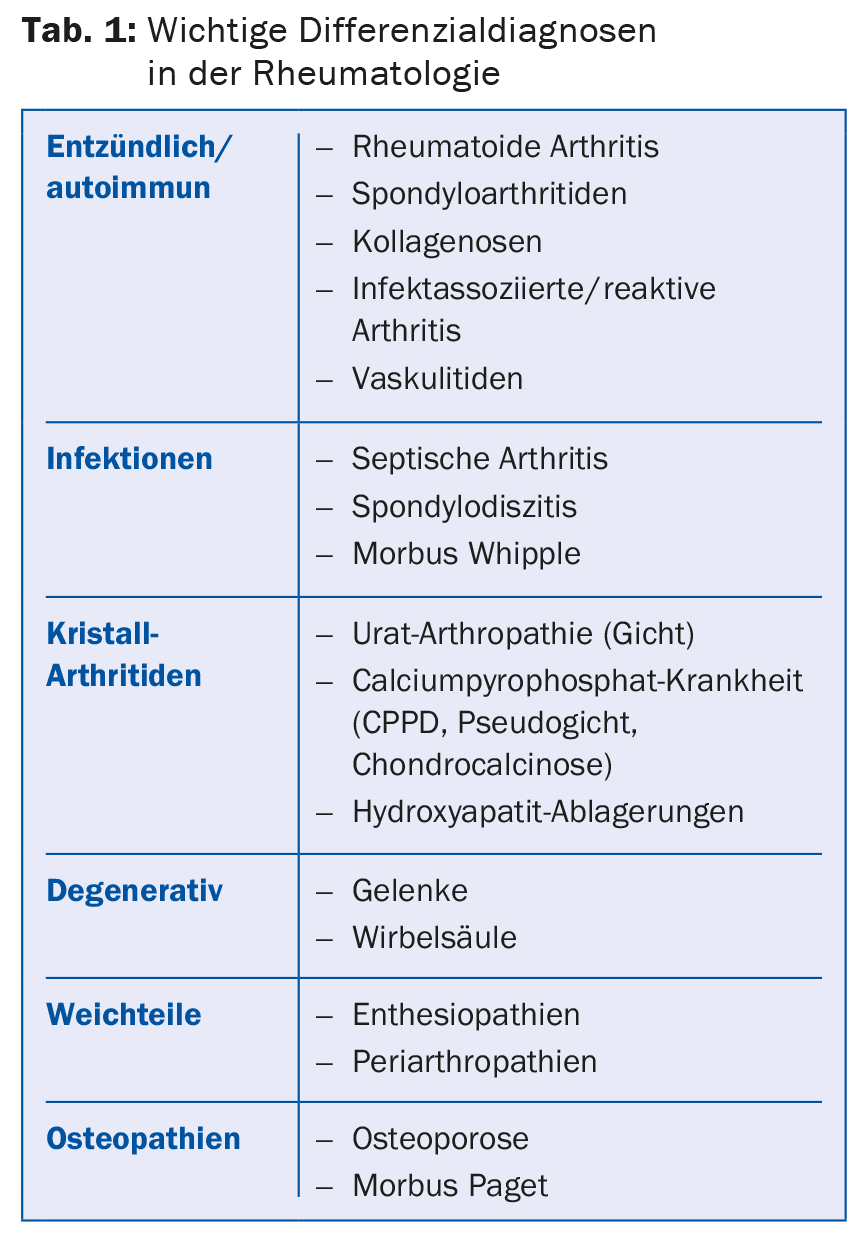
“Fortunately, many diagnoses in rheumatology are not emergencies,” Michael Andor, MD, said at the kickoff. “However, there are few conditions that should definitely not be missed because they are life-threatening, can lead to rapid joint destruction, or can affect organ function.” These important diagnoses include (Table 1):
- Septic arthritis: very rapid joint destruction, potentially lethal, high morbidity, difficult situation for later arthroplasty.
- Large vessel vasculitis (giant cell arteritis, arteriitis temporalis): risk of irreversible blindness, increased vascular risk up to insult. If suspected, begin steroid therapy immediately and do not wait until a biopsy can be taken.
- Small-vessel vasculitis and collagenoses with organ involvement: high morbidity and mortality when kidney, lung, or CNS are involved.
- Erosive inflammatory arthropathies: very rapid joint destruction and increased cardiovascular risk.
Inflammatory or mechanical?
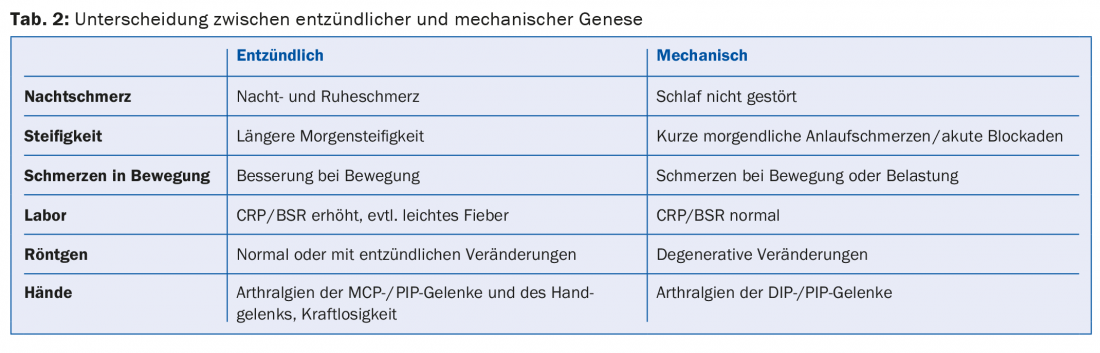
In practice, the distinction between inflammatory and mechanical genesis is important. Anamnestic night and rest pain and prolonged morning stiffness tend to indicate an inflammatory cause, as does elevated CRP, even if the elevation is mild (Table 2) .
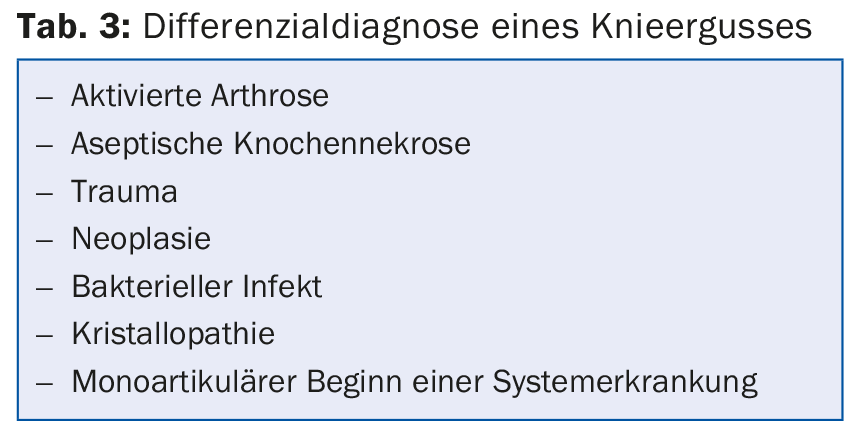
In the case of an acutely swollen knee, the cell count in the joint puncture provides a decisive indication of the genesis: a leukocyte count of >2000/µl indicates inflammation (Tab. 3) . In young patients with a swollen knee, this is considered to be the result of gonorrhea until proven otherwise. “If you suspect gonorrhea, you need to be very persistent with the history,” the speaker recommended. “No patient volunteers that they have had unprotected sex.”
A red, swollen joint is primarily considered an emergency. Caution should be exercised especially in patients who have had podagra several times – it is quite possible that recurrence of swelling and redness of the metatarsophalangeal joint is not caused by gout, but it is septic arthritis in urate arthropathy. Although the joint does not have to be punctured in every case of podagra, possible infections should be carefully clarified during the systemic history and attention should be paid to whether the patient subjectively describes the complaints as “different from what he or she is used to”. In case of doubt, joint puncture is always useful. “Furthermore, you can apply the most effective analgesia with Kenacort and lidocaine in the context of joint puncture,” Dr. Andor reminded.
Inflammatory diseases are often more treatable than mechanical ones. Adequate, prompt treatment is critical to maintaining quality of life and reducing mortality. Primary care providers usually work with a rheumatologist when inflammatory rheumatic disease is suspected. To avoid wasting time with urgent patients, Dr. Andor advised signaling urgency at the time of registration, “Write on the registration form the patient’s specific complaints and that a high-grade suspicion of a particular disease is present. A call to the rheumatologist may also be useful.”
Rheumatoid arthritis, psoriatic arthritis or collagenosis?
For the diagnosis of rheumatoid arthritis (RA), anti-CCP antibodies (ACPA) are considered highly specific when titers are >100 U/ml. This does not apply to low ACPA titers <50 U/ml, in which case it may rarely be a collagenosis, psoriatic arthritis, sarcoidosis, or other infectious or chronic disease. inflammatory disease. Rheumatoid factors are even more nonspecific. Ultrasound plays an important role in the diagnosis of RA because it can detect erosions before they become visible on x-ray, and power Doppler can detect and quantify inflammatory activity early.
With arthralgias and swellings of the DIP and PIP joints, the differential diagnosis is sometimes particularly difficult. Psoriatic arthritis may also be present with very discrete skin involvement and look deceptively similar to finger polyarthrosis. Therefore, a precise personal history (previous skin problems), the family history (psoriasis in relatives?) and the precise examination of the entire skin (including rima ani, scalp, palms and feet, belly button, nails) are important.
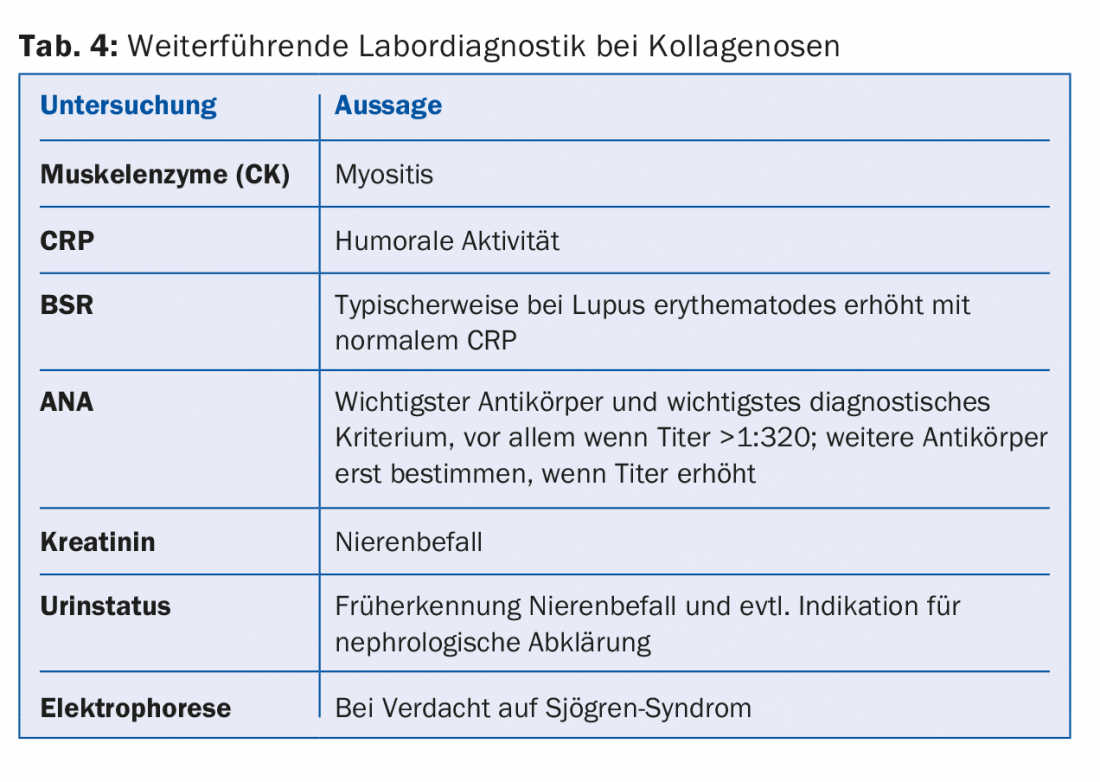
If collagenosis is suspected, it is not useful to simply check “rheumatoid block” on the laboratory sheet. A specific search is diagnostically more useful and costs less (Tab. 4) . Since collagenoses always put the organs at risk, patients may need to be evaluated and followed up by the appropriate specialists (nephrologist, cardiologist, pulmonologist).
Polymyalgia rheumatica – really?
“Polymyalgia rheumatica is one of the most common misdiagnoses,” Dr. Andor said. Symptoms are often nonspecific (shoulder and pelvic girdle pain, morning stiffness >45 minutes, humoral activity, seronegative), but the list of differential diagnoses is long – including paraneoplastic myalgias, infection-associated myalgias, hypothyroidism, and vasculitides.
The disease is very rare in persons under 60 years of age and virtually never occurs in persons under 50 years of age. In younger patients with suspected polymyalgia rheumatica, it is therefore worthwhile to conduct an intensive search for another cause of the symptoms. Also, the criterion that pain subsides rapidly with steroid therapy is not evidence of polymyalgia rheumatica, because steroids work very well for very many conditions. “Pay attention to whether humoral activity also decreases after steroid administration,” the speaker advised. “If it doesn’t, it’s probably not polymyalgia rheumatica.” Basically, “Don’t trust atypical polymyalgia rheumatica – it remains a diagnosis of exclusion.”
Endocrine arthopathies
Endocrine arthropathies also play a significant role in musculoskeletal pain, typically as a result of diabetes mellitus, hypo- or hyperthyroidism, hyperparathyroidism, or, rarely, acromegaly. An endocrine cause should be considered especially in the case of the following complaints:
Carpal tunnel syndrome (CTS) – often operated on even though the condition is due to an underlying endocrine disorder
- CPPD arthropathy (radiological chondrocalcinosis)
- Myalgias and muscle weakness
- Raynaud’s syndrome
Many diabetics suffer from rheumatic complaints. These typically occur when diabetes has been present for a long time. One of the most severe complications is Charcot arthropathy, which affects about 1% of diabetics. Early symptoms include swelling, redness and pain of the foot, and as it progresses, destruction of the toe and metatarsal joints occurs rapidly. Extra-articular manifestations are also common in diabetics, for example calcification of tendons and ligaments, CTS, “frozen shoulder,” Dupuytren’s contracture, or non-painful stiffening of the finger joints (diabetic cheiroarthropathy, fingers can no longer be fully extended).
Source: Update Refresher General Internal Medicine, Module Rheumatology, November 5, 2015, Zurich
HAUSARZT PRAXIS 2015; 10(12): 39-41











