The terms atopic dermatitis, atopic eczema and atopic dermatitis stand for a global skin disease, with children and adolescents being the most frequently affected. In 2020, a systematic review included more than 7000 publications worldwide with epidemiologic data on atopic dermatitis in children and adults. This meta-analysis found that up to 17.1% of adults and 22.6% of children are diagnosed with atopic dermatitis annually.
Neurodermatitis – atopic eczema – atopic dermatitis: These three terms stand for a global skin disease, whereby children and adolescents are most frequently affected. In 2020, by Bylund et al. [1] collected more than 7000 publications with epidemiological data on atopic dermatitis in children and adults worldwide in a systematic review. This meta-analysis found that up to 17.1% of adults and 22.6% of children are diagnosed with atopic dermatitis annually, and up to 9.6% of new cases are recorded in children annually.
We know that atopic dermatitis is a non-contagious, complex and chronic disease, with dominant symptoms such as skin florescences and severe itching with -resulting sleep disturbance. As Tay et al. described in 2002, these symptoms have an increasingly negative impact on the mental and physical situation of affected patients, with eczema and excruciating itching seriously and persistently reducing the quality of life [2].
Evidence of autoimmune-mediated genesis.
In 2006, Biedermann demonstrated that atopic dermatitis also increases the risk of superinfection induced predominantly by Staphylococcus aureus, viruses, and mycoses [3], and Tang et al. demonstrated in 2012 that immunoglobulin E-mediated sensitization to aeroallergens or food allergens is present in 50 to 80% of patients with atopic dermatitis [4]. Furthermore, Tang et al. show in their meta-analysis that in some of these patients evidence for an autoimmune-mediated genesis of atopic dermatitis was found. The authors demonstrated evidence for autoreactivity toward various proteins in 23 to 91% after reviewing 14 studies with 2644 study participants.
Considering the commonly known symptoms of atopic dermatitis such as severe itching, sleep disturbance, and very dry scaly erythematous skin as well as the just mentioned secondary symptoms or diseases, Ho et al. 2010 demonstrated in a study that, due to evidenced and high psychosocial impact and stress on medical staff and caregivers of individuals with atopic dermatitis, their mental and physical stress is significantly higher compared to medical staff of other patient groups, such as for insulin-dependent diabetics [5]. From this point of view, the maxim of the German and Austrian societies and the professional associations for dermatology, allergology and venereology, “the diagnosis and treatment of atopic dermatitis and its complications must be carried out in a medically qualified manner”, in the updated “Guideline atopic dermatitis of 2014”, represents a high standard [6].
Low acceptance for prevention measures
In this context, it must be stated that a certain and precisely definable self-management plays an important role in improving or maintaining the quality of life of patients with atopic dermatitis. However, evidence-based analyses and real-world experience show that there is still too low a level of acceptance for recommended prevention and management measures, including the use of local and systemically administered drugs.
In this context, experience has taught that knowledge about the condition and the understanding based on this also lead to improved compliance and stricter adherence with regard to the implementation of the therapy for the disease neurodermatitis. Subsequently, this results not only in an increase in patient well-being but also in an improvement in treatment outcomes, as shown in studies by Zirwas and Holder from 2009 [7] and Grillo et al. from 2006 [8]. Thus, patients in these studies with a high level of knowledge about diagnosis and diagnosis control were significantly more likely to have restitutio ad integrum or at least significant symptom relief compared with patients with less interest in the course of the disease.
Neurodermatitis control
For clinical control of the course of atopic dermatitis, 3 principles for timely response to exacerbations are imperative:
- Detection and monitoring of possible triggers, identifying allergens in particular for atopic eczema.
- Monitoring the severity of the disease based on symptoms and efflorescences. Optimally, this control is carried out with the patient’s participation.
- Short-term success checks with regard to the current therapy concept.
The latter principle implies an eminent and multifactorial mode of application, as it implies different forms of therapy control. These include traditional contacts with medical staff and, increasingly, interactive contacts via application software recommended by Williams 2005 [9], which can be used to support patients and medical staff via monitoring.
In recent years, it has been shown that apps for smartphones can help increase patients’ and caregivers’ knowledge about their conditions. In addition, it has been demonstrated that this allows certain control functions and decision-making to be exercised in informed patients. These empower them to make informed decisions regarding self-care or care for children and indicate benefits and time savings in that contacts with medical offices and facilities can be reduced to what is necessary, as highlighted in 2016 by Whitehead and Seaton’s study [10].
Compared to other body regions, dermatological diseases have a decisive advantage for smartphone-based forwarding of efflorescences. The assessment of the type and severity of atopic dermatitis is immediately and continuously repeatable after referral by the patient to the professional staff of a medical facility.
Numerous apps have been developed in recent years for the transmission and analysis of atopic dermatitis data to clinical facilities and practices, and evidence of diagnostic inaccuracies in smartphone use has accumulated worldwide for both atopic dermatitis apps and apps for other conditions, as in research by Yang and Silverman in 2014 [11] and by Bates et al. 2018 [12] could be detected. There was also evidence from numerous apps for atopic dermatitis that these medical apps needed to be improved, with attention to improving privacy.
Evaluation of 98 neurodermatitis apps
In a comprehensive study by van Galen et al. from 2020, for the first time, all neuro-dermatitis apps on the market worldwide in 2016-2018 in English, Spanish and Chinese were subjected to an analysis regarding the conformity of these apps with international clinical guidelines [13]. A total of 98 apps were subjected to a quality check in the study. Of these 98 apps, 47% had only educational information about atopic dermatitis, 38% had a tracking function alone, and 13 apps, or 15%, had both functions available. The authors were able to demonstrate that 34% of the apps conveyed erroneous information regarding both treatment recommendations and the prognosis of atopic dermatitis.
Only 13 apps contained information on pharmacological therapies and 16% on non-pharmacological therapies based on international guidelines. Of a total of 98 neurodermatitis apps evaluated, 31 apps (31.6%) had a tracking function for the diagnosis and severity of the condition. However, of these 31 apps, only 12 (12.2%) were based on 3 validated scoring systems. The validated scores were:
- the SCORAD scoredeveloped by the European Task Force in 1993 to objectify the degree of spread, severity and subjective symptoms of atopic dermatitis [14],
- The results of Eichenfield et al. Score developed in 2014 for diagnosis and patient-oriented eczema measurement with monitoring of transepidermal loss of water and skin temperature measurement [15 and
- the data presented by Koh et al. Patient Eczema Severity Time (PEST) score developed in 2017 to record the severity, relapse, or recovery of atopic dermatitis by patients or caregivers [16].
The conclusion of the study by Galen et al. was that the apps currently available for neurodermatitis need to be optimized. In principle, valid quality assurance mechanisms for the creation of neurodermatitis apps should be worked out, on the basis of which one can develop suitable apps for patients and caregivers. As the quality of apps improves, the mobile health management sector could unleash great potential to improve patient care and self-management. A prerequisite for this are measures to improve quality standards, concluded van Galen et al. in your analysis of 2020.
The problems of implementing the requirement to improve quality standards for apps had already been accurately analyzed in 2016 by Albrecht [17] in a comprehensive study by the German Federal Ministry of Health entitled “Gesundheits-Apps – Viele Chancen, wenig Evidenz”. In the analysis, the study authors, led by Albrecht, pointed out that physicians should take a lead role in the emergence of health apps. They therefore conclude: “The medical professions can act as role models here. This requires the professional associations of the health care professions and professional societies, which must also clarify remuneration.
Quality standards for neurodermatitis apps
The quality standards for apps in medicine required for the implementation of Albrecht 2016 in Germany apply equally to neurodermatitis apps developed for patients and parents of affected children. The primary goal of this measure is the intention to provide affected persons and parents with a scientifically based tool for adequate management of the disease and to provide physicians with important, patient-relevant data for targeted therapy. When developing apps for patients with atopic dermatitis, care must be taken to ensure that all personal data stored on them complies with the European data protection guidelines of the EU General Data Protection Regulation with the required care.
The scientific foundation for the development of evidence-based apps is based on the recommendations of the guideline “Neurodermatitis”, which was published within the framework of the Association of the Scientific Medical Societies of Germany in 2015 under the AWMF registration number 013-027 by Albrecht 2016 [17]. The guideline “Neurodermatitis” was developed in cooperation between dermatologists, pediatricians and allergologists. An important statement of the guideline is the recommendation to prescribe partial or full inpatient treatment in addition to outpatient therapy, depending on the severity of the neurodermatitis and special diagnostic issues such as testing of allergens.
Another scientific fund for the development and optimization of neurodermatitis apps results from training and knowledge transfer by the Arbeitsgemeinschaft Neurodermitisschulung im Kindes- und Jugendalter e.V. (AGNES), founded in 1999. It should apply to new neurodermatitis apps to be developed that the medical, educational, psychological and nutritive findings on neurodermatitis conveyed via AGNES find their way into the function of these apps. The neurodermatitis guideline recommends structured interdisciplinary neurodermatitis training according to the curriculum of the Arbeitsgemeinschaft Neurodermitisschulung (AGNES) e.V. (Neurodermatitis Training Working Group) for caregivers with children in the age group up to 7 years and for children from 8 to 12 years and their caregivers, as well as for pa-tients aged ≥13 years with chronic or chronic-recurrent atopic dermatitis. These recommendations are based in particular on the studies by Staab et al. [18,19] and the study by Kupfer et al. [20] on age-related training for children and adolescents and their parents.
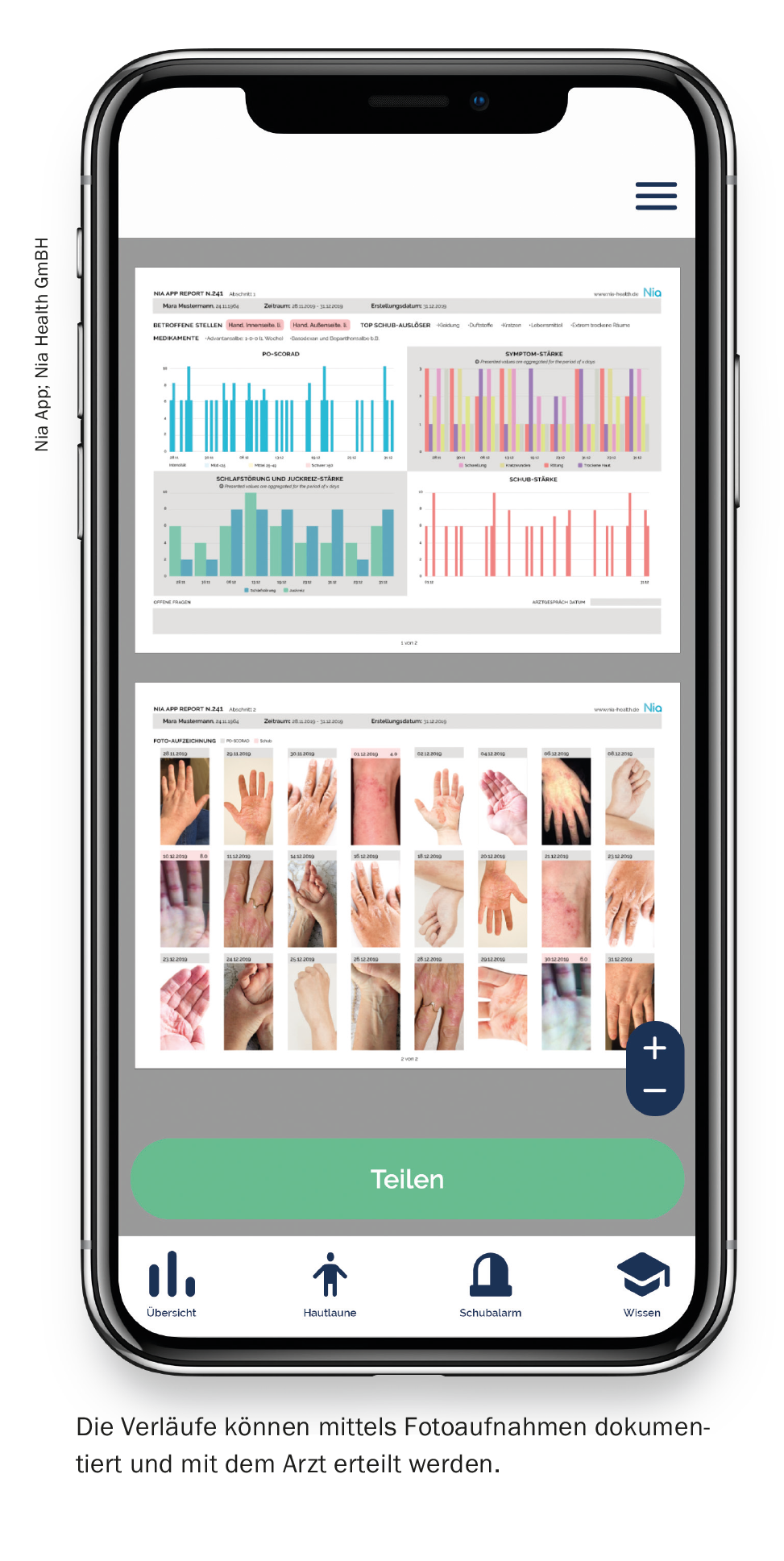
Ongoing documentation with the help of apps
With apps programmed in this way, patients and parents of children with the disease can continuously document the skin changes induced by neurodermatitis on the basis of validated scores such as PO-SCORAD and SA-EASI:
- Photographic images can be used to document the skin florescences of the affected areas of the body.
- Efflorescences such as erythema, lichenification, excoriation, infiltration, crusting, and in the case of the PO-SCORAD, edema, can be used to assess the severity of atopic dermatitis using textual records with a patient-oriented scoring system.
- With the PO-SCORAD you can additionally enter the symptoms “itching” as well as “sleep disturbances”. Using the visual analog scale “VAS”, values from 0 (asymptomatic) to 10 (maximum intensity) are given by the patient for the 2 symptoms, so that 2 results between 0 to 20 scale values can result.
Apps with such functionality help atopic dermatitis patients gain an optimal overview of their health progress through digital accompaniment. Furthermore, documentation enables patients and parents to identify and avoid relapse triggers more quickly, and relevant patient data is immediately available online for physicians.
To optimize knowledge, well-programmed apps must be able to provide sufferers and parents with recommendations for dealing with the disease that are close to everyday life and easy to implement. Furthermore, patients must have the opportunity to receive validated answers to frequently asked, medically relevant questions. Such atopic dermatitis-specific question-answer catalogs should be based on a validated curriculum for the development of evidence-based atopic dermatitis apps, such as the curriculum developed by AGNES [21,22].
High-quality neurodermatitis apps can provide further information to the relevant doctors through sufferers or parents:
- Reporting of a neurodermatitis flare-up and indication of a possible flare-up trigger,
- Comparison of photographs of the skin before and during a neurodermatitis flare-up,
- Notification of medication currently being taken.
The rapid transmission of this information in the form of a detailed report to responsible physicians enables prompt diagnoses and efficient therapy options. In addition to transmitting acute courses of the disease, apps equipped in this way can help to prepare this consultation competently and time-effectively before a visit to the doctor by transmitting medical data and images of the eczematous skin changes.
Neurodermatitis apps classified as high quality are continuously updated with medical knowledge content as well as recommendations for psychological harmonization, optimal nutrition, and advice on suitable sports activities. For example, important guidance is always provided in an up-to-date and timely manner on the four pillars of the AGNES curriculum.
By way of example, the most important evidence-based topics are listed for the four subject areas of medicine, psychology, nutrition, and nursing.
For medicine: information on current training programs for the diagnosis and treatment of neurodermatitis, such as “possible triggers and avoidance of exacerbations”.
For psychology: training in the tactical handling of psychosocial stress situations for affected persons and parents of ill children with stress reduction. Training to develop self-control strategies to reduce scratch frequency and combinations of behavioral therapy and dermatologic training.
For nutrition: training regarding child-friendly nutrition and imparting knowledge about neurodermatitis-relevant food allergies.
For care: training on daily care measures such as application of creams, ointments, dressings and bandages. Information about skin irritating perfumes, shampoos and shower gels.
Conclusion
In recent years, standards for the development of health apps have been defined worldwide, including in Germany by a 2016 study of the Federal Ministry of Health by Albrecht [17]. As outlined in this article on neurodermatitis apps, sound scientific content based on validated scoring systems, highest quality assurance, and legal foundations for data protection are essential prerequisites for the development of efficient health apps.
Take-Home Messages
- None of the atopic dermatitis apps from the study by van Galen et al. from 2020 was from the German-speaking region.
- A high-quality neurodermatitis app should be based on validated scoring systems, the highest quality assurance, and legal foundations for data protection – essential prerequisites for the development of efficient health apps.
- Responsible physicians can already receive important information about the course of the disease in the form of medical data, disease progression with a validated scoring system and images of the eczematous skin changes by means of a high-quality neurodermatitis app, thus creating efficient personalized therapy plans and managing consultations competently and time-effectively.
Literature:
- Bylund S, von Kobyletzki LB, Svalstedt M, et al: Prevalence and Incidence of Atopic Dermatitis: A Systematic Review. Acta Derm Venereol 2020; 100: adv00160.
- Tay YK, Kong KH, Khoo L, et al: The prevalence and descriptive epidemiology of atopic dermatitis in Singapore school children. Brit J Dermatol 2002; 146: 101-106.
- Biedermann T: Dissecting the role of infections in atopic dermatitis. Acta Derm-Venereol 2006; 86: 99-109.
- Tang TS, Bieber T, Williams HC: Does “autoreactivity” play a role in atopic dermatitis? J Allergy Clin Immunol 2012; 129: 1209-1215.
- Ho RCM, Giam YC, Ng TP: The influence of childhood atopic dermatitis on health of mothers, and its impact on Asian families. Pediatr Allergy Immunol 2010; 21: 501-507.
- Atopic dermatitis guideline; www.awmf.org/uploads/tx_szleitlinien/013-27l_S2k_Neurodermitis (last accessed Jan. 31, 2021).
- Zirwas MJ, Holder JL: Patient education strategies in dermatology: part 1: benefits and challenges. J Clin Aesthet Dermatol 2009; 2: 24-27.
- Grillo M, Gassner L, Marshman G, et al: Pediatric atopic eczema: the impact of an educational intervention. Pediatr Dermatol 2006; 23: 428-436.
- Williams HC: Clinical practice. Atopic dermatitis. NEJM 2005; 352: 2314-2324.
- Whitehead L, Seaton P: The effectiveness of self-management mobile phone and tablet apps in long-term condition management: a systematic review. J Med Internet Res 2016; 18: e97.
- Yang YT, Silverman RD: Mobile health applications: the patchwork of legal and liability issues suggests strategies to improve oversight. Health Aff 2014; 33: 222-227.
- Bates DW, Landman A, Levine DM: Health apps and health policy: what is needed? JAMA 2018; 320: 1975-1976.
- van Galen LS, Xu X, Koh MJA, et al: Eczema apps conformance with clinical guidelines: a systematic assessment of functions, tools and content. Br J Dermatol 2020; 182: 444-453.
- European Task Force: Severity Scoring of Atopic Dermatitis: The SCORAD Index. Dermatology 1993; 186: 23-31.
- Eichenfield LF, Tom WL, Chamlin SL, et al: Guidelines of care for the management of atopic dermatitis: section 1. Diagnosis and assessment of atopic dermatitis. J Am Acad Dermatol 2014; 70: 338-351.
- Koh MJ, Giam YC, Liew HM, et al: Comparison of the simple patient-centric atopic dermatitis scoring system PEST with SCORAD in young children using a ceramide dominant therapeutic moisturizer. Dermatol Ther (Heidelb) 2017; 7: 83-93.
- Albrecht UV: Chapter Rationale. In: Albrecht UV. (Ed.): Opportunities and risks of health apps (CHARISMHA). Hannover Medical School 2016, 2-6; www.digibib.tu-bss.de/?docid=6002.
- Staab D, Diepgen TL, Fartasch M, et al: Age-related, structured educational programmes for the management of atopic dermatitis in children and adolescents: multicentre, randomised controlled trial. Br Med J 2006; 332: 933-936.
- Staab D: Structured educational programs for children with atopic dermatitis and their parents. Allergology 2010; 33: 267-270.
- Kupfer J, Gieler U, Diepgen TL, et al: Structured education program improves coping with atopic dermatitis in children and their parents – a multicenter, randomized controlled trial. J Psychosom Res 2010; 68: 353-358.
- Van den Berg N: The AGnES curriculum – evidence-based qualification content and practice competencies from the AGnES model projects (2005-2008) for the implementation of medically ordered assistance services in patients’ homes according to § 87 para. 2b SGB V. Germany, Neubrandenburg University of Applied Sciences 2006.
- Van den Berg N, Meinke C, Heymann R, et al: AGnES: GP support by qualified practice staff. Dtsch Ärztebl 2009; 106: 3-9.
DERMATOLOGIE PRAXIS 2021; 31(3): 10-14