The SARS-CoV-2 pandemic poses special challenges for physicians and patients – even more so if the latter have pre-existing conditions and are on immunosuppressive drugs. Researchers have explored the question of what impact infection can have on patients with inflammatory rheumatic diseases in several recent studies.
How does (re)activation of an inflammatory rheumatic disease influence the risk of infection and the course of infection? And what impact does the immunosuppressive/immunomodulatory effect of clinically effective therapy have on the risk of infection and the course of infection? Prof. Dr. Hendrik Schulze-Koops, Head of the Rheumatism Unit of the Medical Clinic and Polyclinic IV at the University of Munich Hospital and President of the German Society of Rheumatology (DGRh), is currently confronted with such considerations on a daily basis.
According to the rheumatologist, a major problem, especially at the beginning of the pandemic, was that there was no reliable empirical data from China to fall back on. The DGRh has therefore developed recommendations for action on SARS-CoV-2 in recent months, based on the expert opinion of 17 rheumatologists and including analogies to other viral diseases as well as theoretical considerations. The German and English versions of the recommendations are available on the DGRh website [1].
Case study
A 55-year-old female patient with RF/ACPA-positive erosive rheumatoid arthritis on continuous therapy with a TNF inhibitor in combination with 10 mg/week MTX s.c. is in remission. She is perfectly adjusted, she could remain in professional life this way for at least another 10 to 12 years. Since the outbreak of the COVID-19 pandemic, she has meticulously adhered to all hygiene and spacing requirements of the RKI and has not exhibited any symptoms that would indicate COVID-19 disease. “This is quite typical behavior,” Prof. Schulze-Koops explained: “We know that a great many rheumatism patients act very cautiously and intelligently given their health situation.”
One day, the patient contacts him by phone with a request for advice: Her husband had been contacted by a beer garden where he had spent the previous weekend. Another guest who was in the location at the same time has now tested positive for the SARS-CoV-2 virus, he said.
So what should the patient do now – Prof. Schulze-Koops also posed this question to his online plenum and had them vote via live voting. As response options, he offered:
- (a) perform a SARS-CoV-2 PCR test
- (b) perform a SARS-CoV-2 antibody test.
- c) discontinue the TNF inhibitor
- d) continue therapy unchanged and only perform a PCR virus test when symptoms appear and report again to plan further therapy.
The vote of the participating physicians was clearly in favor of answer d with 83% – which would thus also correspond to the recommendation of Prof. Schulze-Koops. His rationale: The RKI defines patients in categories I and II. A patient who has had contact only with an individual who in turn has had contact with an infected individual does not represent a Category I risk situation. Thus, as long as the patient is symptom-free, one would continue therapy unchanged in this situation for fear of reactivation.
Recommendations for action
Prof. Schulze-Koops advised some general and specific measures in dealing with immunosuppressed patients and SARS-CoV-2. His general recommendations are to avoid unnecessary contact in public or at work and, if necessary, to provide the patient with a certificate confirming immunosuppressive therapy for presentation to the employer. Also, the risks of infection vs. the lack of disease control should be weighed against each other: “8 or 10 weeks ago, we were still saying that we as doctors should also avoid contact if possible. In the meantime, however, risk is no longer so high, and at some point the patient must be controlled.” In addition, the expert advises to follow the recommendations of the RKI and, of course, to be ready to cooperate with colleagues who are primarily treating the infection.
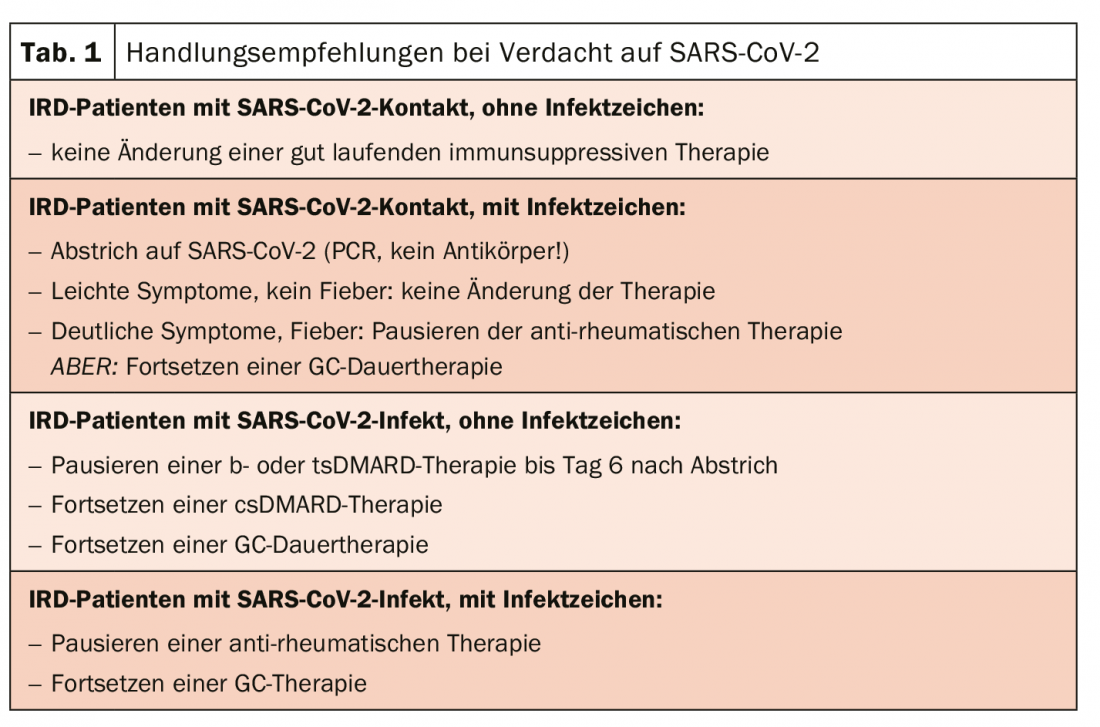
In terms of specific recommendations for action, Prof. Schulze-Koops had one message in particular: DO NOT discontinue/pause/dose reduction of ongoing immunosuppressive therapy solely out of fear of SARS-CoV-2 (Tab. 1)! In the meantime, there are a number of data indicating that patients under rheumatologic therapy are not particularly at risk.
For example, scientists from Italy have published a paper [2] describing the clinical course of COVID-19 in a series of patients with chronic arthritis. They surveyed 320 patients with chronic arthritis on biologic (bDMARD) or JAK-inhibitor (tsDMARD) therapy by telephone between February and March. Among these patients, there were a total of only 4 patients with COVID-19 symptoms and confirmed SARS-CoV-2 infection. 4 patients had clinical symptoms of COVID-19 disease but no evidence of SARS-CoV-2 infection, and 5 patients had contact with SARS-CoV-2 infected persons but no symptoms themselves. “So a maximum of 8 out of 320, which is less than 3% of patients living in northern Italy with a known immunosuppressive therapy, and this at the time of the peak of the Italian pandemic – an extremely low number, which is very reassuring for our patients,” the rheumatologist stated. The symptoms of the affected patients in Italy were typical: they had fever, cough, rhinorrhea and felt listless due to the viral infection, but only one patient had to be hospitalized at all.
A study from New York [3] evaluated 86 patients with inflammatory rheumatic disease (IRD) with COVID-19 (n=59) or suspected COVID-19 (n=27), 62 of whom had bDMARDs or tsDMARDs. Although the patient numbers were relatively small, the evaluation nevertheless shows that the incidence of hospitalization among patients with IRD is as great as that to other patients with COVID-19 in a large New York cohort of about 135 000 infected persons, of whom more than 35 000 had already been hospitalized. According to this study, the fact that patients were already taking biologics at the onset of the disease was not associated with an increased likelihood of severe pandemic COVID-19.
The largest study in this regard comes from central and southern Italy [4]: There, 859 patients with IRD under bDMARD or tsDMARD were also surveyed by telephone. Only 2 patients were found to be positive, one of whom had to be hospitalized for 3 days, and the other was completely asymptomatic. Again, the authors conclude that patients on such therapy do not develop clustered COVID-19. However, the scientists are a bit more cautious in their statement here and emphasize that these results should not lead to possibly attributing a protective role to the drugs, because patients with inflammatory diseases are more aware of the increased risks they are exposed to and therefore have followed and implemented all protective measures – unlike perhaps the one or other average person.
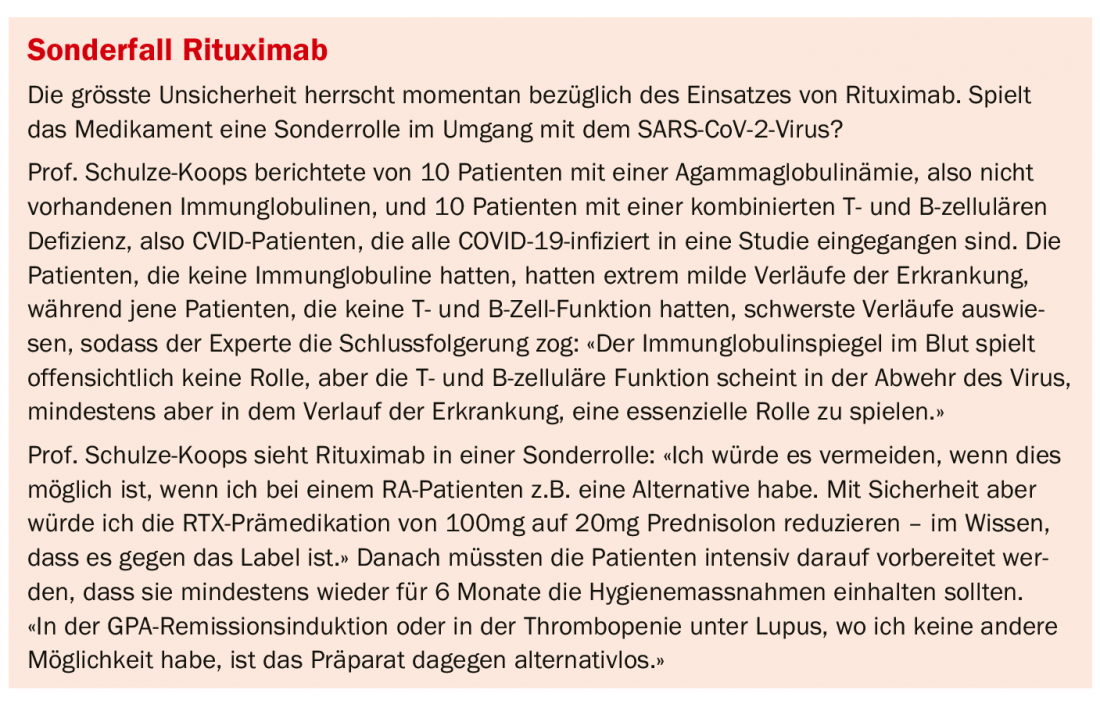
Prof. Schulze-Koops also emphasized this and also reported two deaths in this context: The two RA patients were under rituximab. The first was suddenly diagnosed with COVID-19 disease immediately after his second infusion, and the other six months after the infusion. Both died of multiple organ failure within 10 to 17 days. So there is obviously a need for caution here after all, and not a general all-clear.
Literature:
- https://dgrh.de/Start/Wissenschaft/Forschung/COVID-19/Empfehlungen-für-Patienten.html
- Monti S, et al: Ann Rheum Diss 2020; 79: 667-668; epub 02 Apr 2020.
- Haberman R, et al: N Engl J Med; doi: 10.1056/NEJMc2009567; epub 29 Apr 2020.
- Conticini E, et al: Ann Rheum Dis; doi: 10.1136/annrheumdis-2020-217681; epub 15 May 2020.
InFo PAIN & GERIATry











