In economic terms, back pain plays a major role – not so much because it is particularly expensive to treat, but because it is so common. In addition, many sufferers turn to painkillers without consulting a doctor, often choosing the wrong substance. The Rheumatism League has investigated the extent to which the Swiss suffer from back pain.
In 2018, the Lancet Low Back Pain Series Working Group bemoaned a global problem of mismanagement of low back pain [1]. The group documented the phenomenon of unnecessary care in both high- and low-income settings, where patients receive health care services that do not meet international guidelines. The articles summarized that unnecessary care, including complex pain medications, spinal imaging tests, spinal injections, hospitalizations, and surgical procedures, is dangerous for most patients with low back pain.
For example, a 2018 meta-analysis found that simple imaging tests were requested in a quarter of consultations for low back pain (415,579 of 1,675,720), and the rate of complex imaging (e.g., magnetic resonance imaging) had increased over 21 years [2]. There is no strong evidence of benefit with spinal fusion surgery compared with nonsurgical care for people with low back pain associated with spinal degeneration. And in 2014, 3-4% of the adult population in the United States was prescribed long-term opioid drug therapy, in many cases due to chronic low back pain. As a result, for several years, drug options have taken a back seat in the treatment of back pain and are only recommended when non-drug options have been exhausted or are not effective. All six major international clinical guidelines published since 2016 are moving in this direction (Overview 1).
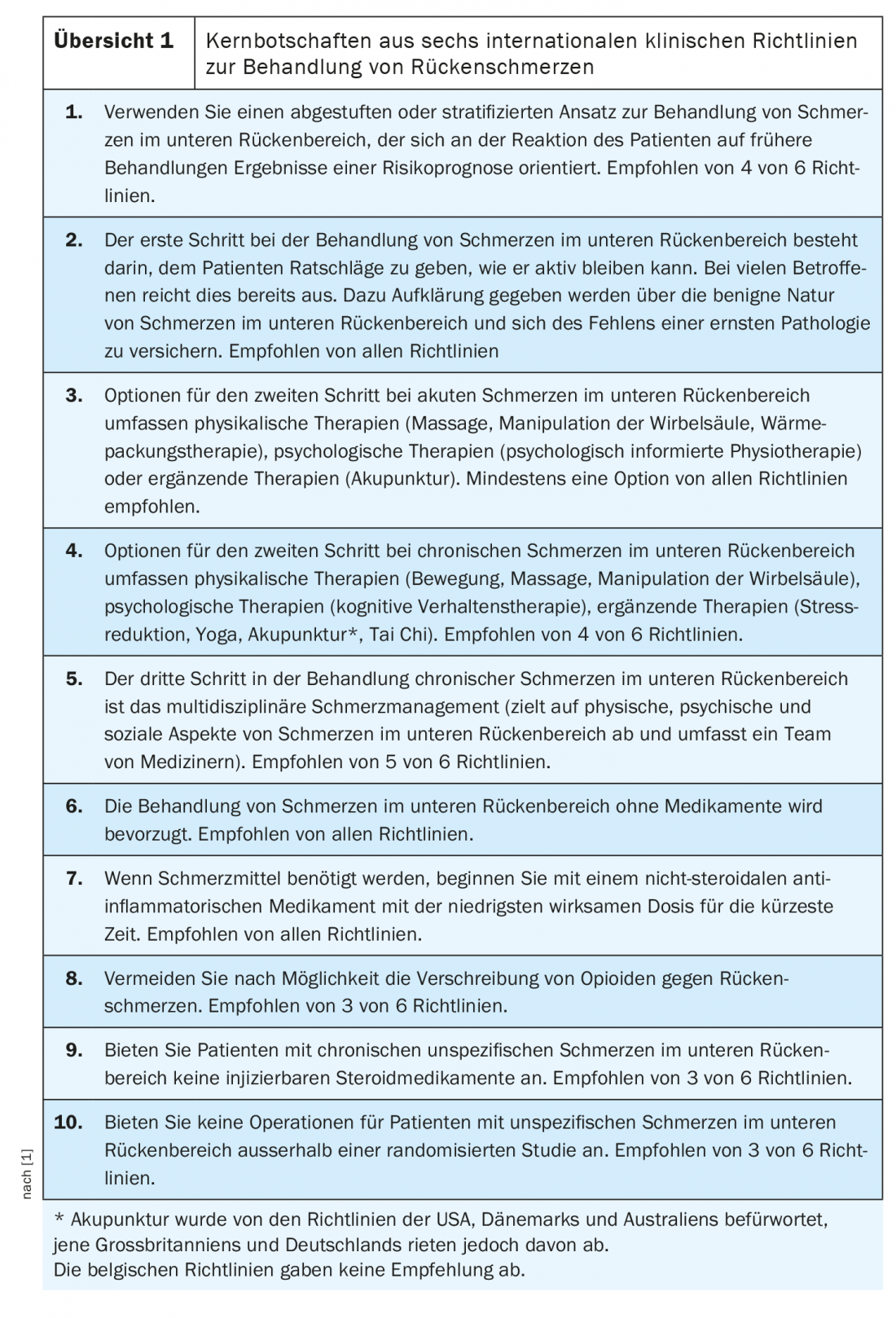
Women and smokers more affected
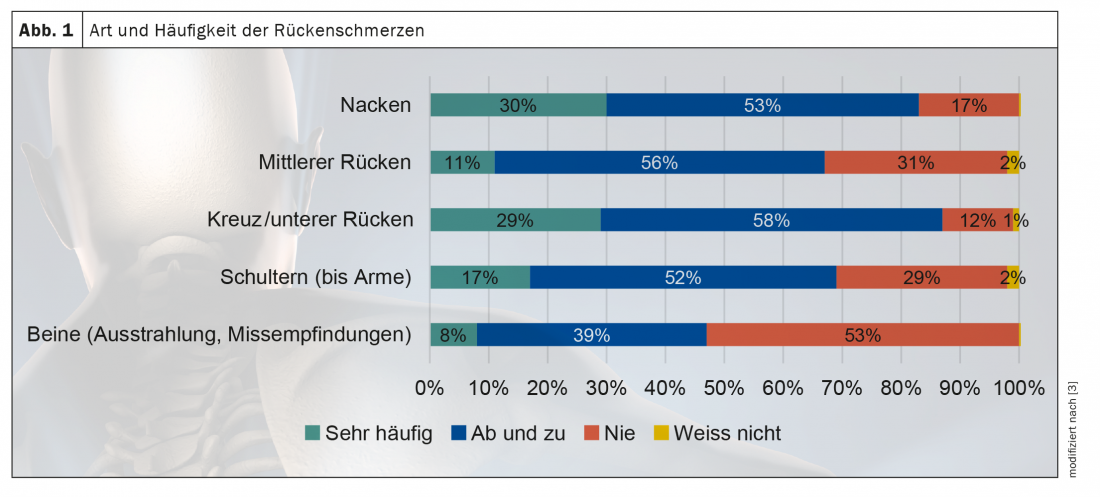
The Rheumatism League Switzerland wanted to find out what the situation is like in Switzerland and, in collaboration with GfK Switzerland, conducted an online survey on the subject of back pain in the spring. The results of the survey are reflected in the Back Report Switzerland 2020, which was published in the summer [3]. One of the key findings: 88% of respondents reported suffering from back pain at least once a year (12%), several times a year (26%), several times a month (28%) or even several times a week (22%). Women and those of lower socioeconomic status are significantly more likely to be affected. Although pregnancy is an additional trigger for back pain in women, the large difference between the sexes (56% vs. 44%) cannot be derived from this alone. Research has also not yet been able to provide conclusive explanations for gender differences in back pain [3]. The results of the back report also indicate that smokers suffer from back pain more often than non-smokers: 60% of smokers have back pain several times a week (31%) to several times a month (29%), compared to only 48% of non-smokers (20% several times a week, 28% several times a month).
The majority of respondents suffer from low back or neck pain (Fig. 1). The majority of Swiss respondents named muscle tension (57%), overload (38%), incorrect movement (37%), stress, worries and problems (33%), wear and tear on the spine, slipped discs, etc. (18%) and spinal deformity (12%) as the reasons for their pain. Muscle tension is seen as a cause significantly more often by “predominantly sedentary” (63.4%) or “sedentary and physical” (64.7%) workers than by purely “physical” workers (55.5%). Working people in full (60%) and part-time (65.4%) perform these tensions significantly more often than non-working people (44.6%). One in four people reported that back pain interfered with their gainful employment.
Caution with opiates
When it comes to managing their back pain, most patients first try to help themselves before seeing a medical professional: “Grit my teeth and live as usual” (75%), actively exercise (71%), and “I try to take it easy and keep rest” (63%) were the top 3 measures. The whole to the doctor (22%) came still after the physiotherapy (30%). However, 58% reported self-medicating. The French-speaking Swiss and women use painkillers significantly more often than the German-speaking Swiss and men (each approx. 70% vs. approx. 60%). People with chronic back pain and smokers also take painkillers for back pain significantly more often than people with acute back pain and non-smokers.
The report’s findings suggest that the majority of respondents are unaware of warning signs of when a visit to the doctor would be appropriate, such as fever, weight loss, or tingling in the arms and legs. This finding is concerning because fever, weight loss, and neurologic deficits are among the “red flags” that require rapid evaluation by a specialist, the report’s authors write.
In the past, non-opioid analgesics (e.g., acetaminophen) were often prescribed for acute back pain. However, recent evidence increasingly points to the ineffectiveness of such analgesics and advises the use of nonsteroidal anti-inflammatory drugs (NSAIDs) for acute back pain [1,4]. Caution is especially advised when taking opiates. Here, the guidelines clearly recommend taking them only for chronic back pain and only for a short period of time as part of an overall therapeutic approach [4,5]. In cases of acute non-specific back pain, it is advised to inform the sufferers about the good prognosis and the high chances of self-healing.
Literature/Sources:
- Traeger AC, Buchbinder R, Elshaug A, et al: Care for low back pain: can health systems deliver? Bulletin World Health Organization 2019; 423-433; doi: 10.2471/BLT.18.226050.
- Downie A, Hancock M, Jenkins H, et al: How common is imaging for low back pain in primary and emergency care? Systematic review and meta-analysis of over 4 million imaging requests across 21 years. Br J Sports Med 2019; doi: 10.1136/bjsports-2018-100087.
- Rheumaliga Schweiz: Rückenreport Schweiz 2020; www.rheumaliga.ch/assets/doc/CH_Dokumente/medien/grosser-rueckenreport-2020/Rueckenreport-2020.pdf.
- Foster NE, et al: Low back pain 2: Prevention and treatment of low back pain: evi-dence, challenges, and promising directions. The Lancet 2018; 391: 2368-2383; doi: 10.1016/S0140-6736(18)30489-6.
- Oliveira CB: Clinical practice guidelines for the management of non-specific low. European Spine Journal 2018; 2792-2800; doi: 10.1007/s00586-018-5673-2.
HAUSARZT PRAXIS 2020; 15(12): 22-24