Chronic critical limb ischemia is the most advanced form of PAVD, requiring rapid action and an aggressive therapeutic approach to save the affected limb. Especially in diabetics, this disease progresses subtly and often not according to the classic, easily assignable symptoms. The amputation rate is alarmingly high in patients with critical limb ischemia. New, mainly interventional methods with very good primary and secondary openness rates have become established in recent years. These procedures are sometimes very complex, elaborate, time-consuming and require, in addition to manpower, appropriate equipment that can only be offered in a large center.
Chronic critical limb ischemia is defined as persistent, recurrent ischemic rest pain requiring regular adequate analgesia for more than two weeks. The systolic ankle artery pressure must be below 50 mmHg or the toe artery pressure below 30 mmHg. Furthermore, chronic critical limb ischemia includes ulceration or gangrene of the foot or toes with ankle artery pressure less than 50 mmHg or toe artery pressure less than 30 mmHg.
In German-speaking countries, peripheral arterial disease (PAVD) is predominantly assessed according to the Fontaine classification [1] (Table 1) .
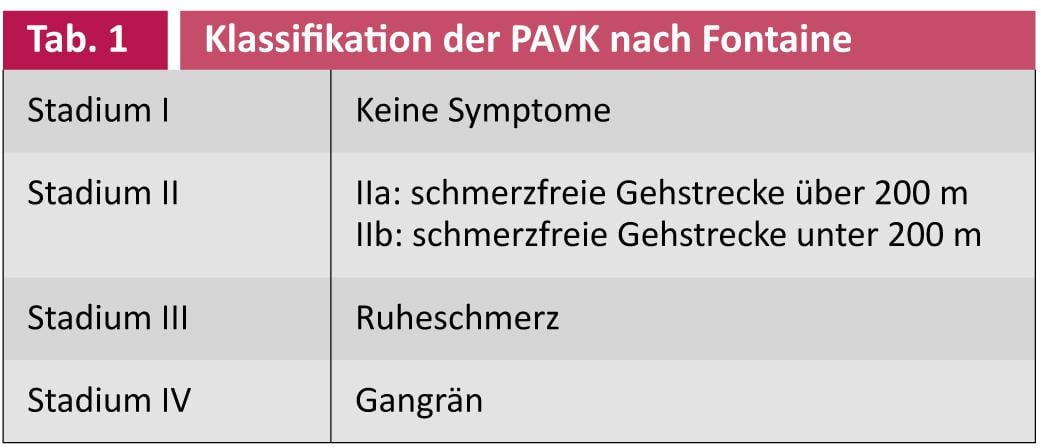
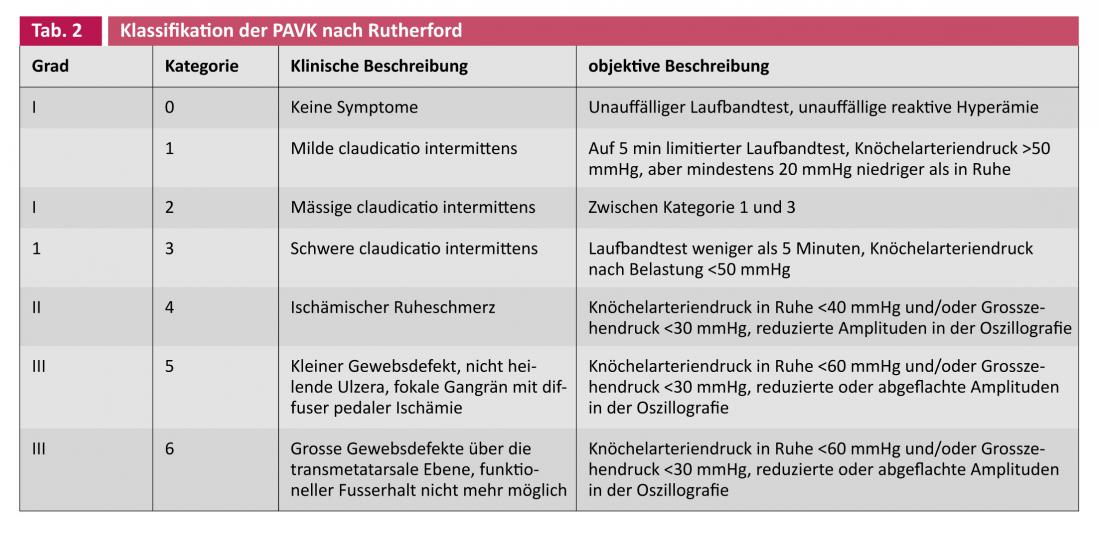
Critical ischemia corresponds to stage III or IV. In the Anglo-American world, the classification according to Rutherford is preferred [2] (Table 2) . Categories 4-6 correspond to critical ischemia.
If revascularization is not possible, the amputation rate in the following six months is 50%. The prognosis quo ad vitam is very poor: 25% of patients with critical limb ischemia die within the first year, 32% within the first two years [3, 4]. Patients with diabetic foot syndrome, who usually have multisegmental, severe vascular changes without the typical symptoms of PAVK, are particularly at risk. In addition, arterial pressure values are often incorrectly high because the arteries can no longer be sufficiently compressed due to pronounced mediasclerosis; sometimes even the peripheral pulses are still palpable in the sense of a stop pulse. All of this lulls us into a false sense of security. Ulcerations of the leg or foot should therefore not be underestimated, especially in patients with diabetes mellitus. In order to save the affected extremities, no unnecessary time should be lost; rapid diagnosis and aggressive revascularization measures are urgently indicated.
Patients with critical limb ischemia (Fig. 1). require the infrastructure of a large major hospital with a corresponding interdisciplinary team of specialists available around the clock. In recent years, great progress has been made in the therapeutic field, especially in interventional therapy. Drug therapy, especially secondary prophylaxis with platelet function inhibitors, lags behind this rapid development, although first studies with a more specific platelet function inhibition with thrombin receptor antagonists have recently been published [5]. However, it is likely to be years before these promising compounds are ready for the market, and even then it remains to be determined whether these new drugs are suitable for secondary prophylaxis after interventional or vascular surgery. There has been a noticeable shift from surgery to minimally invasive catheter interventions [6, 7]. Frequently, autologous venous material is not found to be sufficiently suitable for the demanding and difficult operations or the outflow is too weak to ensure a long openness of the bypass [8, 9]. The main therapeutic goals are to restore adequate blood flow to eliminate rest pain, prevent amputation, and improve the patient’s quality of life.
Clinic
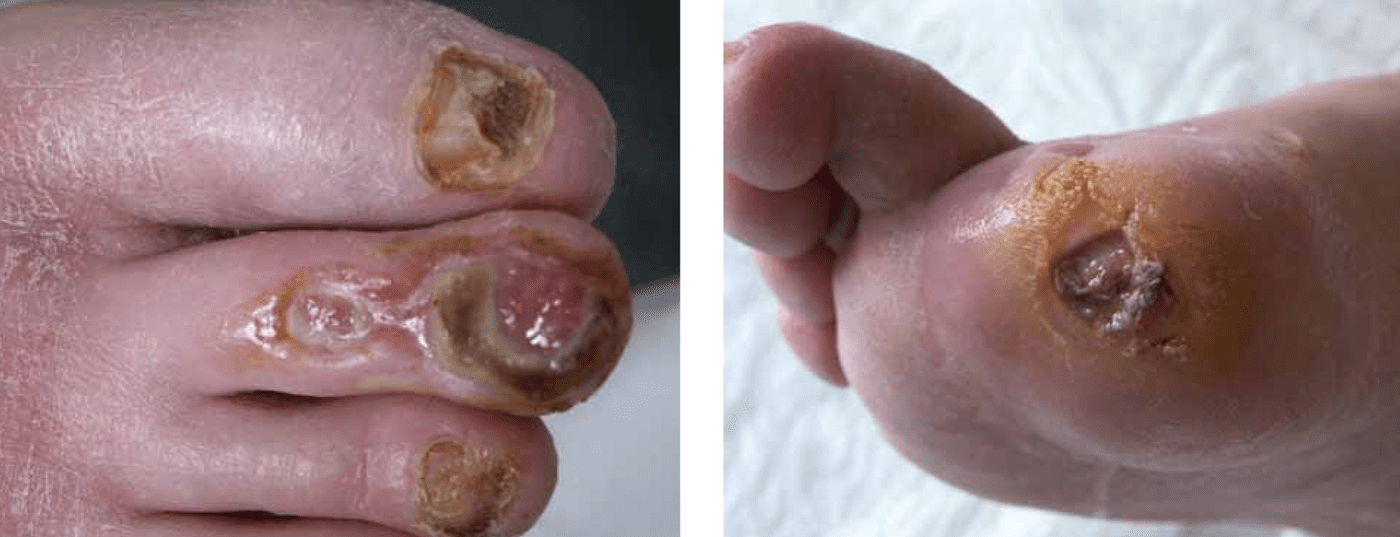
The primary complaints are severe pain, tissue defects, or ischemic neuropathy. Pain at rest occurs predominantly at night, with attacks of pain lasting minutes to hours, which improve when the patient lets the affected leg hang out of bed or sleeps in a sitting position in a chair. Clinically, dry skin, lack of body hair, and loss of subcutaneous adipose tissue are noticeable. Critical limb ischemia does not always present in such a clear and unambiguous clinic, especially in diabetics. In diabetics, all changes are more subtle due to peripheral polyneuropathy. Rest pain is often absent, and diabetic neuropathic ulcer (Fig. 2) usually precedes critical limb ischemia. In order to prevent the disaster in such a case, it is absolutely necessary to act quickly and actively. Unfortunately, many such patients do not come into the hands of a specialized center at all or much too late, so that then not only the affected limb but possibly the life of the affected patient is endangered.

Diagnosis
The key is not to waste unnecessary time. Patients with critical limb ischemia belong in a specialized center quickly. The diagnosis cannot always be made based on clinical presentation and history. A complete vascular status with acquisition of ABI, segmental and digital pulse oscillography, toe artery pressure measurement (Fig. 3), and transcutaneous partial pressure oxygen measurement are standard in these patients.

The next step is duplex sonography, which usually allows immediate treatment planning. In most cases, the goal is to quickly make a decision as to whether an interventional procedure is possible or appropriate, or whether a more complex surgical or hybrid procedure needs to be performed. Duplex sonography in the hands of an experienced specialist is comparable to intra-arterial angiography [10]. The latter can then be performed as part of the interventional or hybrid procedure.
In very complex cases, if time permits and if available, MR angiography is obtained. A targeted, rapid approach without waiting unnecessarily for imaging studies is crucial.
Basic therapy/secondary prophylaxis
Adequate analgesia is a matter of course. A patient with true critical limb ischemia usually requires morphine. Non-steroidal anti-inflammatory drugs, paracetamol or other analgesics are usually not sufficient.
Critical limb ischemia is one of the most severe forms of generalized atherosclerosis, as evidenced by the very poor prognosis of these patients. It should go without saying that these patients should have aggressive secondary risk factor management according to current recommendations.
Drug therapy
Several multicenter controlled trials have shown that critical ischemia can be improved and amputations prevented with a minimum three-week infusion course of iloprost if revascularization is not possible [11, 12].
Interventional therapy
This is where the greatest progress has been made in recent years. Improved techniques and better equipment now allow interventions with amazing success rates that were considered impossible just a few years ago (Fig. 4a-d) . The most important instruments are still a guide wire and a balloon. Fine-tuning, especially of the guidewires, additional equipment such as atherectomy devices, drug-coated balloons (see article by Dr. Büchel et al., p. 15), recanalization aids, unconventional puncture sites, and much more, now allow successful recanalization even in cases that seem hopeless.

In critical limb ischemia, anything that brings blood to the affected limb in any form is allowed. We do not wish to discuss conventional “pure balloon angioplasty” at this point. The method has long proved its worth in the more than 40 years of its existence. In the meantime, an “intervention first” strategy has been documented in numerous studies and has ultimately also found its due place as a clear recommendation in TASC II.
Chronic total occlusion (CTO) is the major challenge today. Chronic total occlusions are technically demanding, time-consuming interventions with special CTO wires and/or CTO catheters [13]. The success of interventional therapy depends on the number and patency of downstream vessels, the patency of plantar arch arteries, and the collateral network between these vessels. For example, the cumulative rate of openness at one year is 25% for a patent artery in the lower leg; it increases to 81% for three arteries in the outflow tract [14]. The more lower leg arteries are pervious, the better and faster the ulcer healing [15]. Recanalization of the arteries mainly responsible according to the angiosome concept is crucial for therapeutic success [16, 17]. The three arteries of the lower leg supply five areas distal to the malleolar plane that can be anatomically classified (angiosomes) [18].
Subintimal recanalization
If it is not possible to bring a guidewire through a long-stretch, heavily calcified occlusion, subintimal recanalization can be performed (Fig. 5a-c) . The first published primary and secondary success rates with a leg preservation rate of 66%, survival rate of 71% and freedom from amputation of 48% after one year made people sit up and take notice [19].
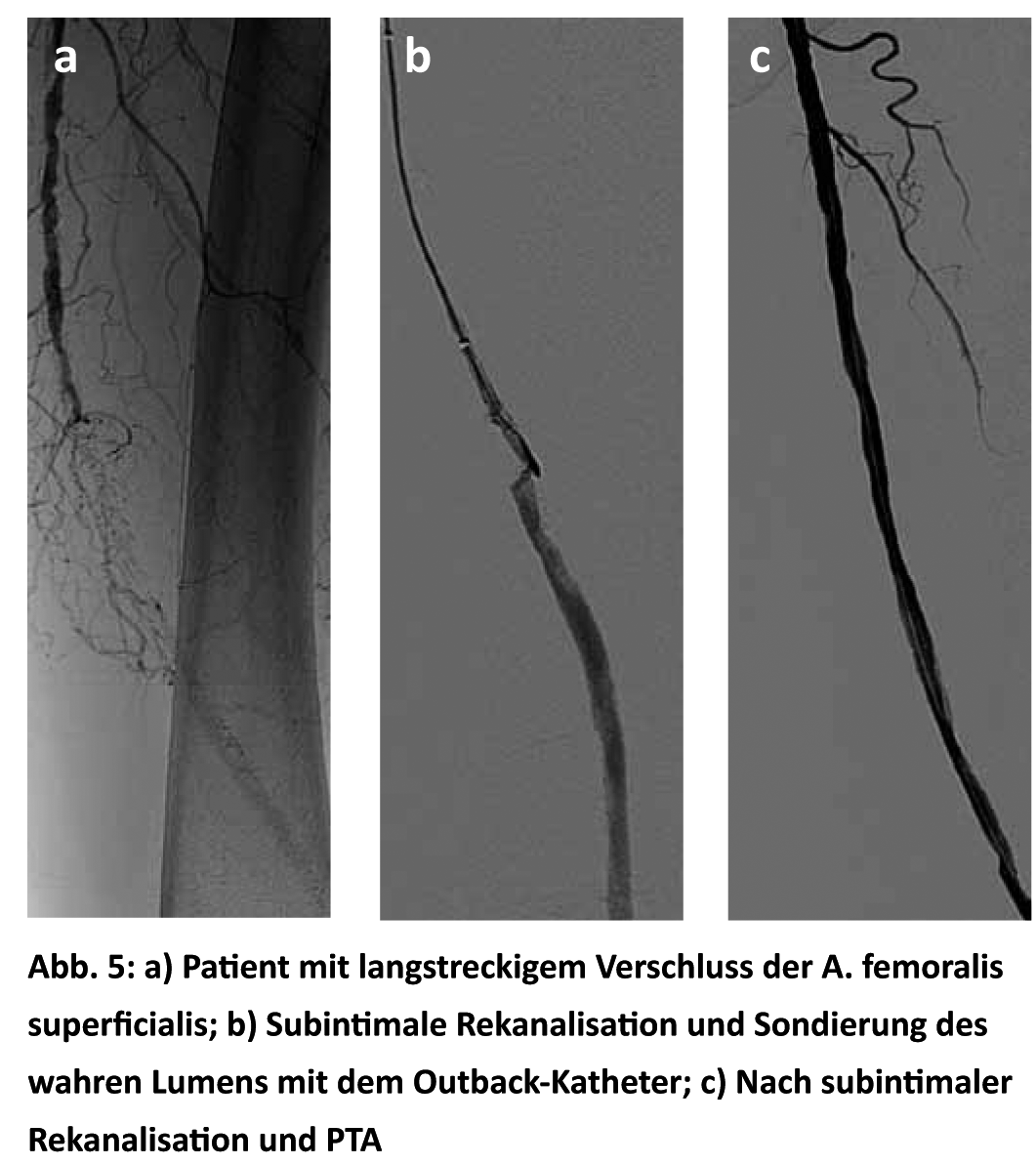
The problem of reconnecting distally to the true lumen was solved by the introduction of the Outback catheter. This method has been the subject of much discussion and has resulted in many publications that have come to very different conclusions. In our hands, subintimal recanalization has not been as successful, so our primary goal is to restore the original lumen, which is increasingly successful with the new generation of CTO wires.
Primary stenting
For supragenual long-distance occlusions, primary stenting has better long-term outcomes than balloon angioplasty alone, with primary open rates of 90, 78, 74, and 69% at one, two, three, and four years, respectively (Zilver stent). The assisted primary open rate was as high as 96% in the first year and then remained at 90% in subsequent years [20]. To obtain such a good result, regular follow-up checks are essential.
When paclitaxel-eluting Zilver stents [21] were used, the results were even better, with a three-year open rate of 83%. Disappointing results have been shown in two trials of sirolimus-eluting stents in long-segment occlusions of the superficial femoral artery, which failed to demonstrate a significantly better difference compared with bare-metal stenting [22, 23].
There are good results for stenting of infrapopliteal lesions. For example, stent-assisted infrapopliteal PTA achieved a primary success rate of 94% with 96% freedom from rest pain, prevention of amputation, and ulcer healing in 82 patients with an extremity at risk of amputation and no longer amenable to surgical management [24].
Drug-eluting stents are becoming more and more prevalent. A comparative study of sirolimus-eluting stents versus bare metal stents showed clear superiority of the SES group in the lower leg. Within a median follow-up period, no restenoses occurred in the SES group compared with 39.1% in the BMS group [25].
Atherectomy
We use atherectomy with the TurboHawk system (Fig. 6) mainly for highly calcified, eccentric sclerotic plaques.
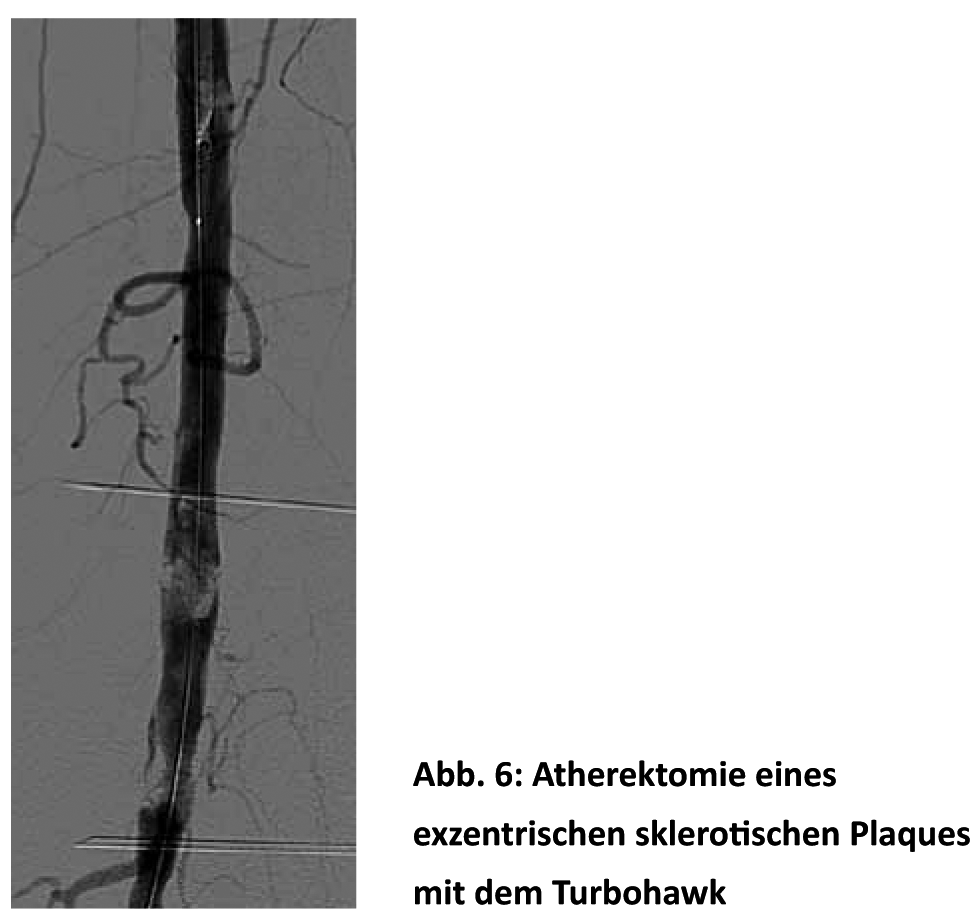
Theoretically, this method avoids the shear forces on the vessel wall, the risk of dissection, elastic recoil, and the potential inflammatory responses after PTA and stenting, which should manifest in a decreased number of restenoses. In any case, initial larger studies showed promising results with amputation prevention in 82% [26]. A primary and secondary open rate of 67 and 91% after one year and of 60 and 80% after two years, respectively, is quite respectable [27].
Conclusion
When leg loss is imminent, any means will do to somehow get blood to the affected limb. The more arteries that can be opened, the better the long-term success. Over the years, we have learned that primary and secondary openness rates do not equate to clinical success. The main therapeutic goal is restoration of blood flow, elimination of rest pain and adequate ulcer healing. If successful, it is possible to get the patient into a gait training program and promote collateral vessel formation. Thus, the discrepancy between primary/secondary openness rate and clinical course is explained. The leg preservation rate and clinical success of intervention were 70 and 80%, respectively, at five years in a larger study of diabetic patients, whereas the primary and secondary openness rates were only 33 and 66%, respectively [28].
Literature:
- Fontaine R, Kim M, Kieny R: The surgical treatment of peripheral arterial circulatory disease. Helv Chir Acta 1954; 5/6: 199-533.
- Rutherford RB, Baker JD, Ernst C, et al: Recommended standards for reports dealing with lower extremity ischemia: a revised version. J Vasc Surg 1997; 26: 517-538.
- Dormandy JA, Rutherford RB: Management of peripheral arterial disease TASC Working Group, TransAtlantic Inter-Society Consensus (TASC). J Vasc Surg 2000; 31 (1Pt 2): S1-S296.
- Norgren L, Hiatt WR, Dormandy JA, et al: Inter-society consensus for the management of peripheral arterial disease (TASC II). J Vasc Surg 2007; 1 Suppl: S5-S67.
- Morrow DA, Braunwald E, Bonaca MP, et al: Vorapaxar in the secondary prevention of atherothrombotic events. NEJM 2012; 366: 1404-1413.
- Faglia E, Dalla Paola L, Cierici G, et al: Peripheral angioplasty as the first-choice revascularization procedure in diabetic patients with critical limb ischemia: prospective study of 993 consecutive patients hospitalized and followed between 1999 and 2003. Eur J Vasc Endvasc Surg 2005; 29: 620-627.
- Bosiers M, Hart JP, Deloose K, et al: Endovascular therapy as the primary approach for limb salvage in patients with critical limb ischemia: experience with 443 infrapopliteal procedures. Vascular 2006; 14: 63-69.
- Nowygrod R, Egorova N, Greco G, et al: Trends, complications and mortality in peripheral vascular surgery. J Vasc Surg 2006; 43: 205-216.
- Conte MS, Bandyk DF, Clowes AW, et al: Results of PREVENT III: a multicenter, randomized trial of edifoligide for the prevention of vein graft failure in lower extremity bypass surgery. J Vasc Surg 2006; 43: 742-751.
- Eiberg JP, Madycki G, Hansen MA, et al: Ultrasound imaging of infrainguinal arterial disease has a high interobserver agreement. Eur J Vasc Endovasc Surg 2002; 24: 293-299.
- U.K. Severe Limb Ischaemia Study Group: Treatment of Limb Threatening Ischaemia with Intravenous Iloprost: A Randomised Double-blind Placebo Controlled Study. Eur J Vasc Surg 1991; 5: 511-516.
- Dormandy J, Belcher G, Bross P, et al: On behalf of the Hawaii Study group: Prospective study of 713 below-knee amputations for ischaemia and the effect of a prostacyclin analogue on healing. British Journal of Surgery 1994; 81: 33-37.
- Khalid MR, Khalid FR, Farooqui FA, et al: A novel catheter in patients with peripheral chronic total occlusions: a single center experience. Catheter Cardiovasc Interv 2010; 76: 735-739.
- Lazaris AM, Salas C, Tsiamis AC, et al: Factors affecting patency of subintimal infrainguinal angioplasty in patients with critical lower limb ischemia. Eur J Vasc Endovas Surg 2006; 23: 668-674.
- Fernandez N, McEnaney R, Marone LK, et al: Multilevel versus isolated endovascular tibial interventions for critical limb ischemia. J Vasc Surg 2011; 54: 722-729.
- Neville RF, Attinger CE, Bulan EJ, et al: Revascularization of a specific angiosome for limb salvage: does the target artery matter? Ann Vasc Surg 2009 ; 23: 367-373.
- Iida O, Nanto S, Uematsu M, et al: Importance of the angiosome concept for endovascular therapy in patients with critical limb ischemia. Catheter Cardiovasc Interv 2010; 75: 830-836.
- Taylor GI, Palmer JH: The vascular territories (angiosomes) of the body: experimental study and clinical applications. Br J Plast Surg 1987; 40: 113-141.
- Spinosa DJ, Leung Da A, Mastumoto AH, et al: Percutaneous intentional extralumial recanalization in patients with chronic critical limb ischemia. Radiology 2004; 232: 499-507.
- Ferreira M, Lanziotti L, Monteiro M, et al: superficial femoral artery recanalization with self-expanding nitinol stents: long-term follow-up results. Eur J Vasc Endovasc Surg 2007; 34: 702-708.
- Ansel GM, Zilver PTX drug-eluting stent trial shows superior 3-year TLR rates in femoro-popliteal disease treatment, EVToday 2012, www.EVToday.com.
- Duda SH, Bosiers M. Lammer J, et al: Drug-eluting and bare nitinol stents for the treatment of atherosclerotic lesions in the superficial femoral artery: long-term results from the SIROCCO trial. J Vasc Interv Radiol 2005; 16: 331-338.
- Duda SH, Bosiers M, Lammer J, et al: Sirolimus-eluting versus bare nitinol stent for obstructive superficial femoral artery disease: the SIROCCO II trial. J Vasc Interv Radiol 2005; 16: 331-338.
- Feiring AJ, Wesolowski AA, Lade S: Primary stent-supported angioplasty for treatment of below-knee critical limb ischemia and severe claudication: early and one-year outcomes. J Am Coll Cardiol 2004 ; 44: 2307-2314.
- Scheinert D, Ulrich M, Scheinert S, et al: Comparison of sirolimus-eluting vs. bare-metal stents for the treatment of infrapopliteal obstructions. EuroIntervention 2006.
- Kandzari DE, Kieszh RS, Aliie D, et al: Procedural and clinical outcomes with catheter-based plaque excision in critical limb ischemia. J Endovasc ther 2006; 13: 12-22.
- Zeller T, Sixt S, Schwarzwalder U, et al: Two-year results after directional atherectomy of infrapopliteal arteries with the SilverHawk device. J Endovasc ther 2007; 14: 232-240.
- Alexandrescu V, Hubermont G, Philips Y, et al: Combined primary subintimal and endoluminal angioplasty for ischaemic inferior limb ulcers in diabetic patients: 5-year practice in a multidisciplinary diabetic foot service. Eur J Vasc Endovasc Surg 2009; 37: 448-456.
CARDIOVASC 2013; no. 1: 8-13.