Inflammatory bowel disease (IBD) can have many causes. However, the connection with exposure to altitude has not yet been investigated prospectively. Scientists from Zurich have now approached this question with a study.
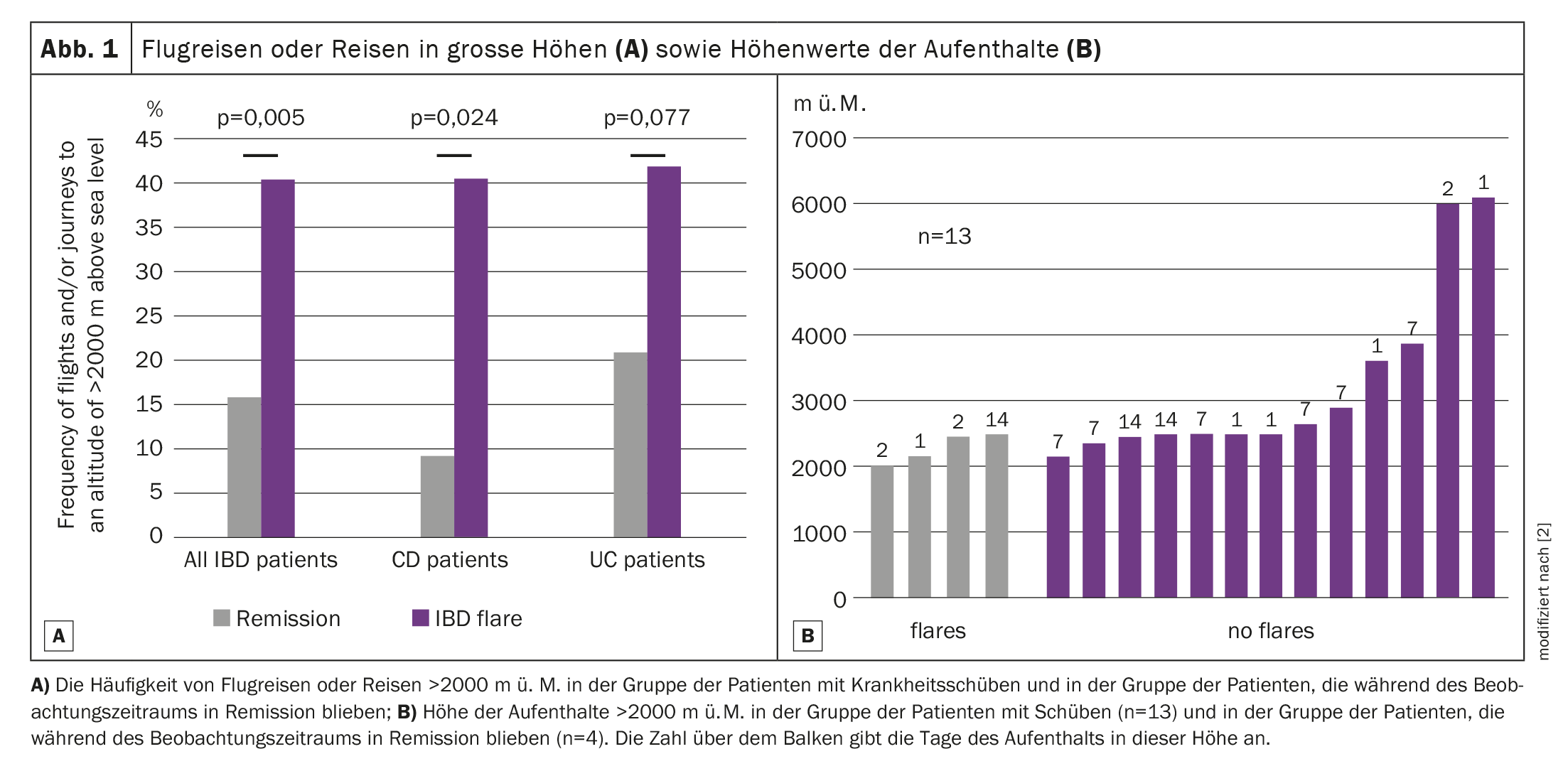
To date, it is known that high altitudes can lead to gastrointestinal ulcers and are associated with worsening of IBD patients, explained Prof. Dr. Stephan Vavricka, Center for Gastroenterology and Hepatology and University Hospital Zurich, by way of introduction [1]. Travel to the mountains and flights are associated with an increased risk of relapses in patients with inflammatory bowel disease (Fig. 1) .
However, there have been no studies to date that have prospectively investigated the effects of altitude exposure on the activity of IBD. Prof. Vavricka’s group has now investigated the disease activity in IBD patients after 3 hours of exposure in a hypobaric pressure chamber imitating an altitude of 4000 meters and compared the results with healthy control subjects. The focus was on clinical and endoscopic disease activity and the composition of the microbiota in the three cohorts.
11 patients with Crohn’s disease (CD, 6 men, age 35.6 ± 13.7 years), 9 patients with ulcerative colitis (UC, 3 men, 31.4 ± 10.8 years) and 10 healthy control subjects (7 men, 27.7 ± 4.9 years) underwent rectosigmoidoscopy at the outpatient clinic in Zurich, the baseline value was thus 490 meters above sea level. This was followed by 3 hours of exposure in a hypobaric pressure chamber (follow-up examinations on day 1 and day 7). The pressure in the chamber was 462 mmHg, the PaO2 value was 7 kPa. Disease activity was also assessed using symptom scores, CRP levels and fecal calprotectin. The composition of the intestinal mucosa-associated microbes was analyzed using high-throughput sequencing.
Calprotectin increased in CD patients
Exposure in the hypobaric pressure chamber was well tolerated by all subjects. The mean oxygen saturation decreased from 97.5% ± 1.3 to 80.9% ± 4.1 and returned to normal values after the hypobaric intervention (p<0.0001). Clinical and endoscopic disease activity was not significantly changed before and after the intervention. However, two UC patients experienced a mild relapse, and another UC patient was no longer included in the follow-up due to a relapse.
New endoscopic lesions were detected in one healthy volunteer and one UC patient. Prof. Vavricka continued. Fecal calprotectin levels increased significantly in CD patients during the follow-up period (p=0.031), but not in UC patients and healthy controls. No changes were observed in the CRP values. The percentage of calprotectin-based disease remission (fecal calprotectin <100 μg/g) decreased in all groups after exposure to the hypobaric pressure chamber and increased thereafter, with a significant decrease in the control group (100% at baseline vs. 50% at day 1, p=0.029) and in all patients combined (73.3% at baseline vs. 36.7% at day 7, p=0.013). No differences were observed in the alpha and beta diversity of the composition of the stool microbiota before and after exposure to the hypobaric pressure chamber.
The three-hour exposure in a hypobaric pressure chamber did not lead to higher disease activity, Prof. Vavricka concluded. However, mild relapses and the development of endoscopic lesions were observed in a subgroup of patients. According to the expert, the significant decrease in calprotectin-based remission rates between baseline and day 7 indicates a subclinical effect of short-term hypoxia.
Take-Home-Messages
- In a prospective study with healthy volunteers and IBD patients, a 3-hour exposure in a hypobaric low-pressure chamber led to higher disease activity in some patients.
- Calprotectin-based remission rates decreased significantly between baseline and day 7, suggesting a subclinical effect of short-term hypoxia.
- This cannot be explained by changes in the composition of the microbiota in general.
Congress: SGG Annual Congress 2023
Sources:
- Vavricka SR: Vortrag «A prospective interventional study to evaluate the effect of hypoxia on healthy volunteers and patients with inflammatory bowel disease: The Altitude IBD study»; Jahreskongress der Schweizerischen Gesellschaft für Gastroenterologie (SGG), Interlaken, 14.09.2023.
- Vavricka SR, Rogler G, Maetzler S, et al.: High altitude journeys and flights are associated with an increased risk of flares in inflammatory bowel disease patients. Journal of Crohn’s and Colitis 2014; 8(3): 191–199; doi: 10.1016/j.crohns.2013.07.011.
GASTROENTEROLOGIE PRAXIS 2023; 1(2): 18–19