Cervical lymphadenopathies are painful or painless swellings of the cervical lymph nodes and may be due to leukemias, lymphomas, and tumors of the head, neck, and mouth, in addition to local or systemic infections. Suitable imaging techniques for detecting cervical lymphoma include sonography, computed tomography, and especially magnetic resonance imaging.
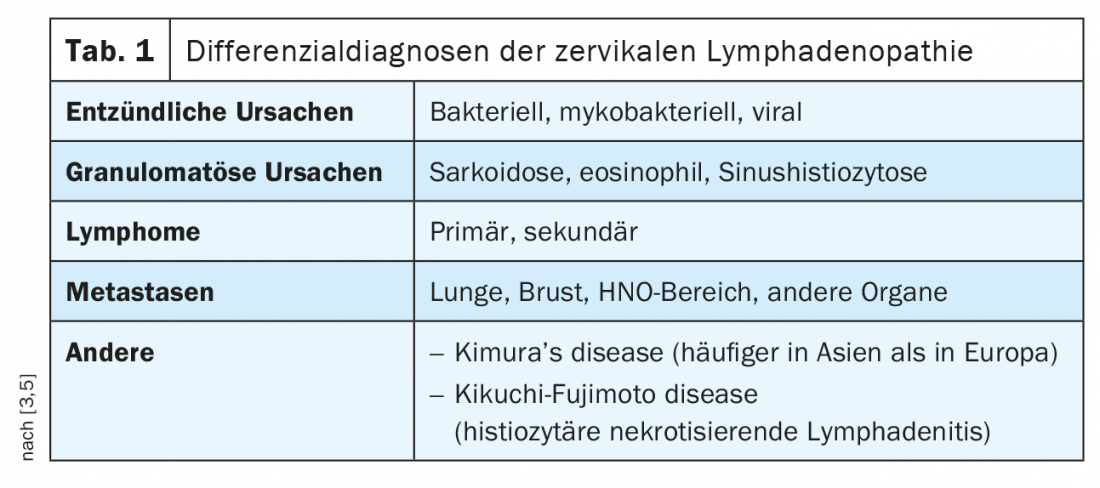
Cervical lymph node swelling is common in daily practice. A wide spectrum of causes needs to be clarified with varying clinical symptoms [3], ranging from asymptomatic to severe. Accurate medical history, clinical and laboratory examinations as well as further imaging diagnostics are part of the diagnosis, which in some cases must be supplemented by tissue clarification. Table 1 lists important differential diagnoses of cervical lymph node swelling.
Cervical lymph node enlargement can occur in all age groups. They can also be an expression of a tumorous event in children and adolescents, although inflammatory causes predominate in this age group [2]. In the age group below 14 years, malignant lymph node changes have a frequency of 1:7000, with Hodgkin’s and non-Hodgkin’s lymphomas accounting for about 10-15%.
Lymphomas in Hodgkin’s and non-Hodgkin’s disease account for a proportion of malignant lymph node swellings in the neck that should not be underestimated, even in adults [4,8]. The median peak age for men is 46, for women 43.
Accurate anamnesis and clinical examination are the basis of diagnostic measures. Depending on the extent and localization, they may cause dysphagia, a sensation of pressure and lumpiness in the throat, or dysphonia. B-symptomatology can be recorded anamnestically. Hematologic differential diagnosis with clarification of subtypes sets the prognostic course. The extent of lymph node involvement or even other organs can be reliably determined with cross-sectional imaging examinations.
Radiographic examinations have no role in the detection of cervical lymphoma. Occasionally, soft tissue-dense space-occupying lesions are seen with large lymphoma conglomerates, including displacement and stenosis of the trachea. If osseous destruction is present, it can be detected radiographically.
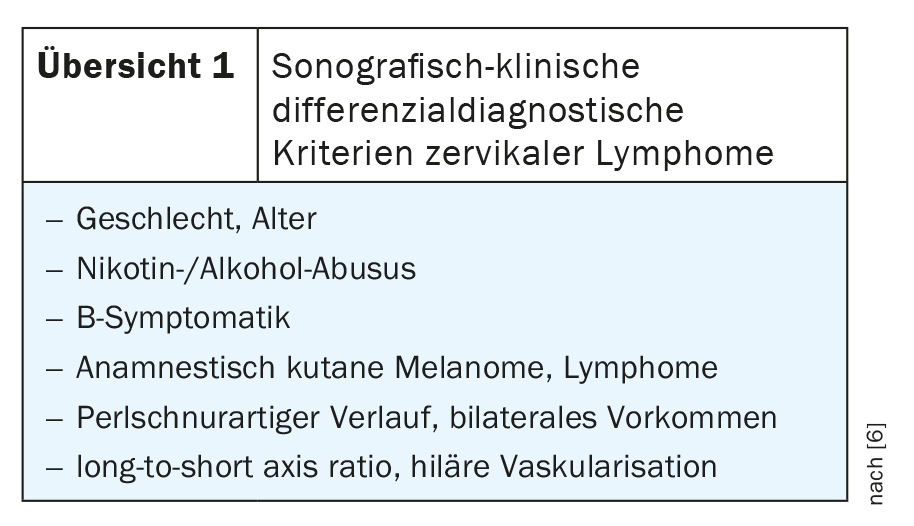
Sonography of the soft tissues of the neck can already be used in a diagnostic direction in cervical lymphomas that are readily assessable by imaging. In overview 1 anamnestic and image morphological criteria of the differential diagnosis of lymph node enlargement of the neck can be read [6].
Computed tomography and especially magnetic resonance imaging (with the high soft tissue contrast) are efficient imaging techniques in the detection of cervical lymphoma [1]. Contrast-assisted MRI is very good at detecting inflammatory and melting changes and soft tissue infiltration, and CT has a slightly higher value in assessing bony changes. A diagnostic algorithm for CT examinations has been developed to differentiate cervical necrotizing lymphadenopathy, including several image morphologic and clinical criteria [7].
Case study
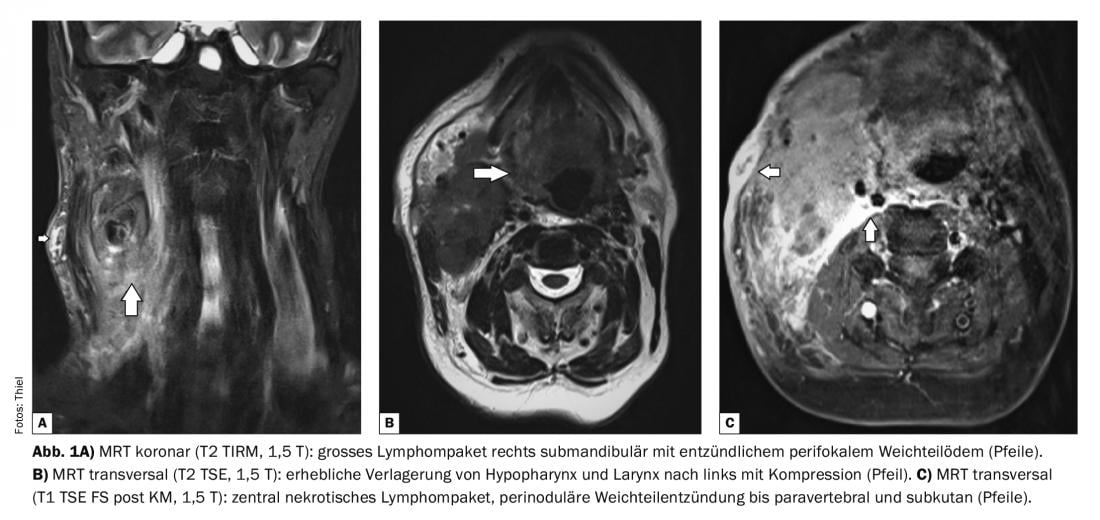
Case report 1 shows a large lymphoma packet in a 57-year-old patient at the time of examination (Fig. 1A to C) . Biopsy showed necrotizing lymphadenitis. The space-occupying effect was remarkable with displacement of the submandibular gland, displacement of the base of the tongue, and hypopharynx and larynx to the left. Compression of the jugular vein and lateralization of the sternocleidomastoid muscle. There was also a suspicion of an initial fistula to the lateral side, cutis and subcutis as well as platysma were inflammatory edematous thickened. Clinically, there was a marked clinical picture with reduced general condition, fever, difficulty swallowing, pain and swelling of the right side of the neck and the angle of the jaw, and redness of the skin.
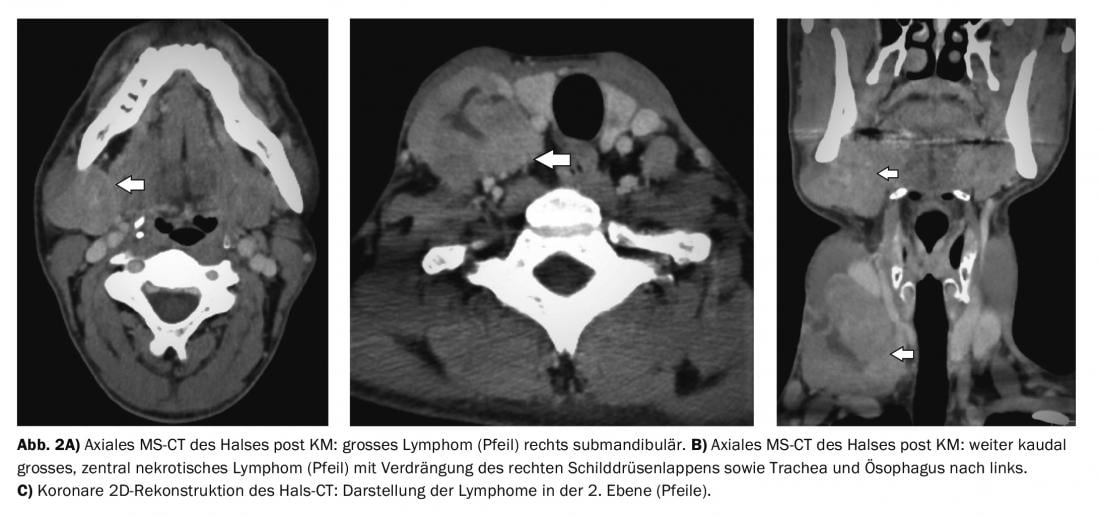
case 2 documented cervical lymph node metastases (Fig. 2A to C) submandibular and deep cervical with resulting dysphagia in a 37-year-old man with neuroendocrine carcinoma.
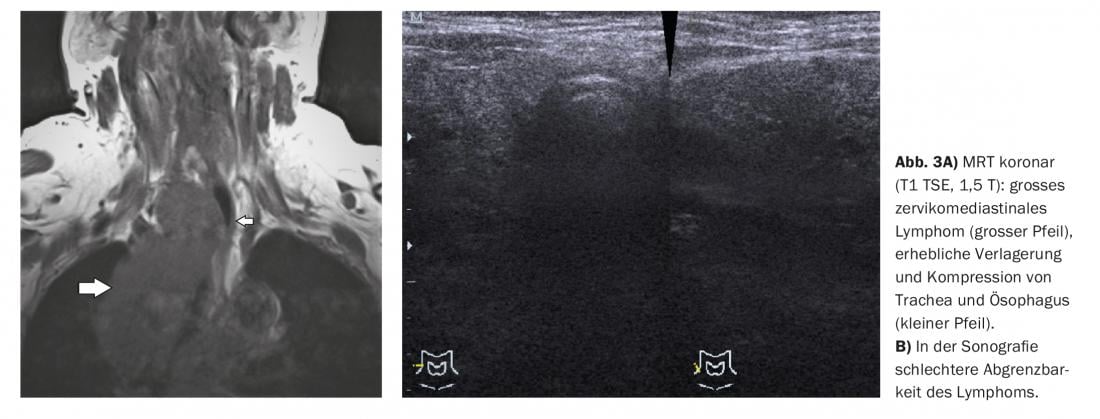
Case example 3 shows the extent of inflammation with reactively enlarged lymph nodes from cervical, mediastinal to abdominal in a patient with actinomycosis (Fig. 3A and B) who was 57 years old at the last follow-up examination with a 16-year course. There was also dysphagia.
Take-Home Messages
- Cervical lymph node swelling occurs in a variety of inflammatory and tumor diseases. They can occur in all age groups.
- Depending on the size and location, they cause different discomfort.
- The exact diagnostic assignment of lymphomas requires a precise history, clinical and laboratory examination, and further imaging clarification.
- Biopsy can be used for tissue classification and determination of dignity.
Literature:
- Chisin R, Weber AL: Imaging of lymphoma manifestations in the extracranial head and neck region. Leuk Lymphoma 1994; 12(3-4): 177-189.
- Gaini RM, et al: Lymphomas of head and neck in pediatric patients. Int Pediatr Otorhinolaryngol 2009; 73 Suppl 1: S65-70.
- Kaji AV, Mohuchy T, Swartz JD: Imaging of cervical lymphadenopathy. Semin Ultrasound CT MR 1997; 18(3): 220-249.
- Nayak LM, Deschler DG: Lymphomas. Otolaryngol Clin North Am 2003; 36(4): 625-646.
- Rafaty FM: Cervical adenopathy secondary to toxoplasmosis. Arch Otolaryngol 1977; 103(9): 547-549.
- Strassen U, et al: Sonographic differentiation between lymphatic and metastatic disease in cervical lymphadenopathy. Laryngoscope 2018; 128(4): 859-863.
- You SH, et al: Cervical necrotic lymphadenopathy: a diagnostic tree analysis model based on CT and clinical findings. Eur Radiol 2019; 29(10): 5635-5645.
- Zapater E, et al: Malignant lymphoma of the head and neck. Oral Dis 2010; 16(2): 119-128.
HAUSARZT PRAXIS 2022; 17(9): 36-38