Struma colli (“goiter”) is the name given to an enlargement of the thyroid gland of varying etiology. If goiter is clinically suspected, imaging techniques (scintigraphy, x-ray, CT, MRI) are informative. The choice of examination depends on the clinical findings and the research question.
In the previous articles on dysphagia, various causes of dysphagia have already been discussed. The subject will be continued today with struma colli. The complex diagnosis of enlarged thyroid gland includes clinical, laboratory and imaging examination, primarily with sonography. This procedure is available nationwide, is inexpensive, relatively less time-consuming, and can be used without problems in all age groups in the absence of radiation exposure. It is the ideal imaging diagnostic method for progress monitoring during therapy. Laboratory tests of thyroid hormones and antibodies are an important part of the examinations and consecutive therapeutic medicinal or also remedial surgical treatment. Functional tests such as iodine or technetium uptake complement the laboratory procedures. Thyroid scintigraphy completes the morphologic and functional view of the thyroid situation [1,4]. Prior to scheduled CT examinations with intravenous administration of contrast medium, clarification of the functional status of the thyroid gland is required, since the high iodine concentration in the X-ray contrast medium can provoke acute hyperthyroidism if the patient has a corresponding disposition.
When thyroid pathology is clinically suspected, nodular changes are detected sonographically in up to 67% of examinations [3]. The sensitivity of the method is 88% and the specificity is 49%. With a negative predictive value of 88%, the diagnostic confidence is 94%. The malignancy rate reaches 5%.
Diffuse volume increase of the thyroid gland, which may also spread retrosternally, without nodular change or hyperthyroid metabolic state is called diffuse euthyroid goiter, usually caused by iodine deficiency. If the change is detectable in at least 5% of the local population, endemic goiter is present. Autoimmune diseases, biosynthetic disorders and nodular changes are then accompanying factors in the history of these patients.
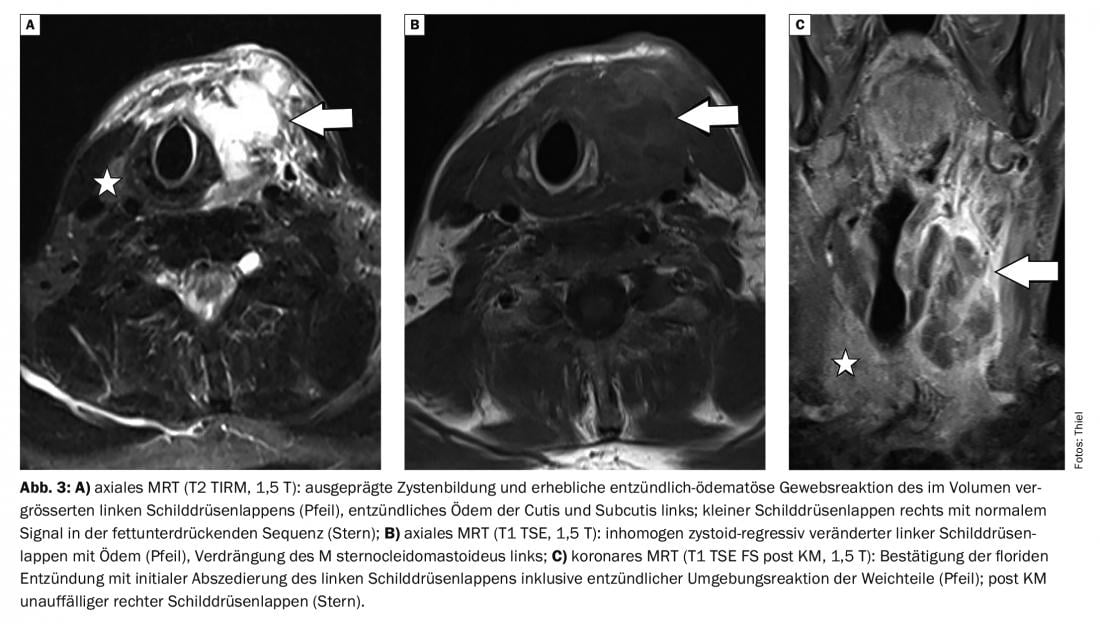
Table 1 lists the different types of goiter with their functional characteristics. The risk of adenoma degeneration correlates with the tissue structure (Tab. 2) . The WHO classifies goiter into different degrees of severity (Tab. 3), which is based on the size of the thyroid gland [5]. The symptomatology of goiter is variable and size-dependent. Small strumen and nodules are usually asymptomatic. If the size progresses, local discomfort with a feeling of laxity, pressure or tightness in the throat occurs in the course of the disease, occasionally there is a compulsion to clear the throat. When pressure is applied to the esophagus, dysphagia may develop, and stenosis of the trachea causes difficulty breathing and shortness of breath. Large retrosternal portions of goiter may limit hemodynamics of supraaortic vessels.
The therapy is to be determined individually, depending on the size of the goiter, resulting symptoms and metabolic situation.
X-ray examinations cannot provide information about the actual size of the thyroid gland and its functional position. A space-occupying effect on the trachea is demonstrable with images of the neck in 2 planes.
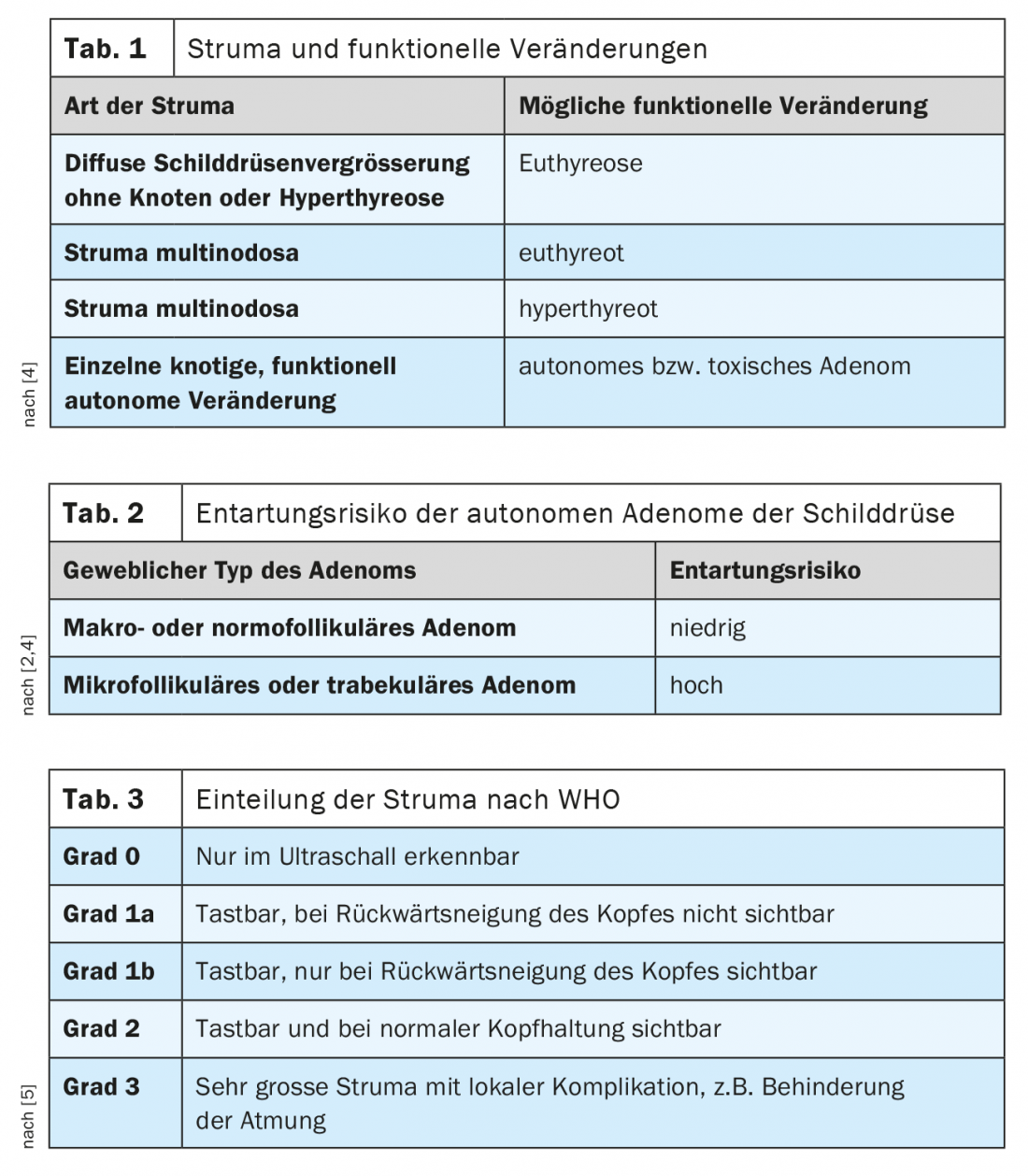
Along with scintigraphy, sonography is the imaging modality of choice for structural assessment of the thyroid gland; scintigraphically cold nodules can also be verified in the presence of cysts. The volume of the thyroid lobes can also be reliably determined by ultrasonography.
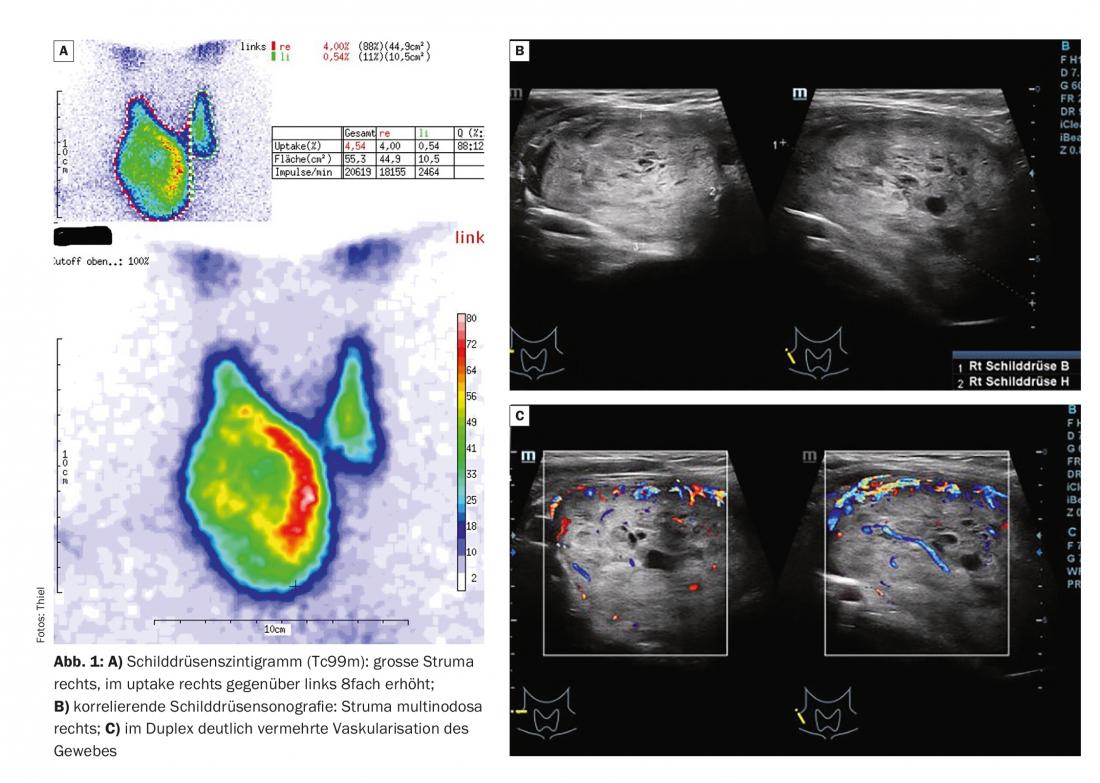
Computed tomography can assess the shape, size, and structure of the thyroid gland; however, the imaging technique is not the method of choice for thyroid diagnosis. If structural pathologies, e.g., regressive changes or volume increases, are present, they are usually incidental findings on CT scans of the neck region or spine.
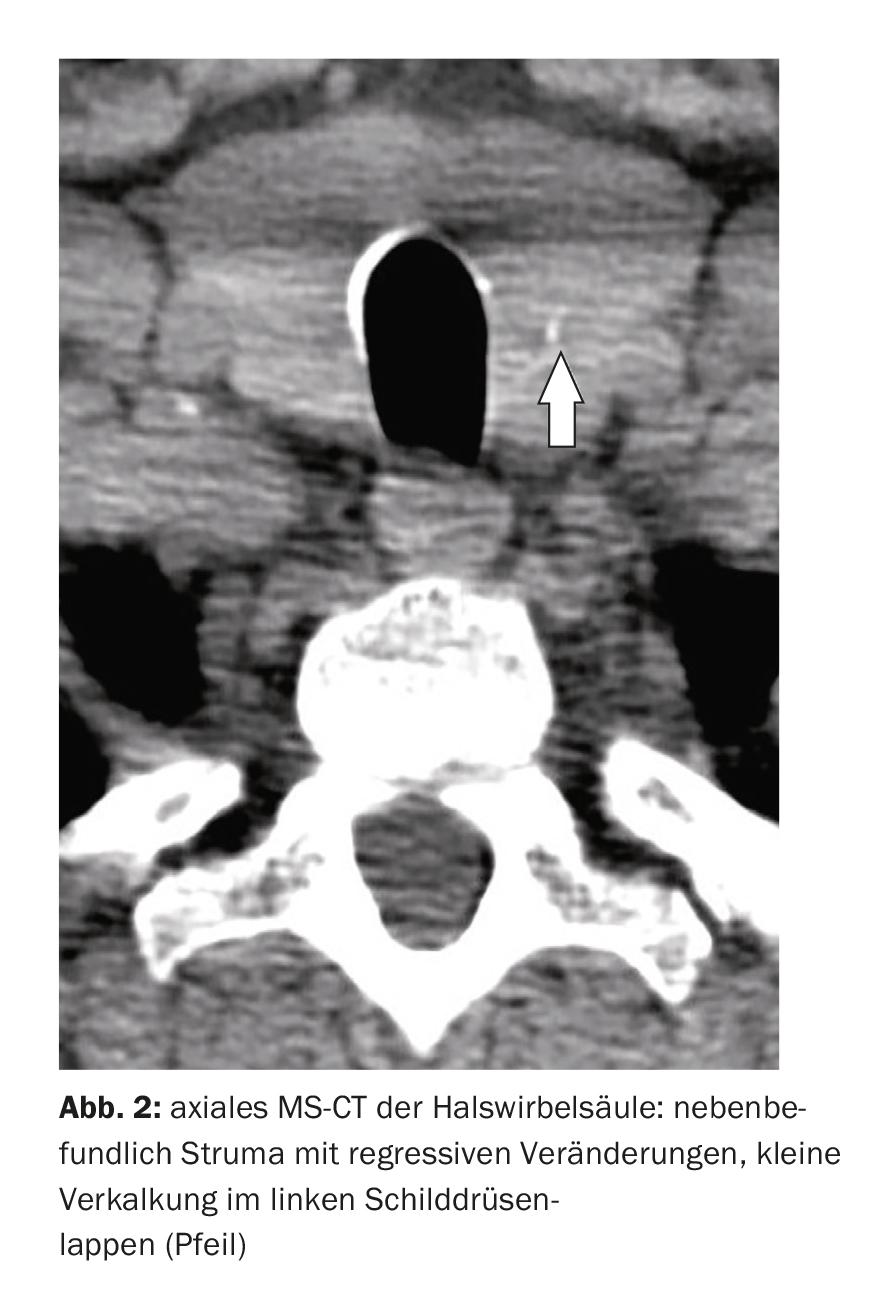
Magnetic reson ance imaging, like computed tomography, is not the primary imaging tool for thyroid examination. Extensive local tumorous processes or inflammations are, however, very good for differential diagnosis and the advantages of the fine ionizing radiation and the high soft tissue contrast should not be underestimated. Intravenous contrast administration is possible in goiter or hyperthyroidism because MR contrast agents do not contain iodine.
Case studies
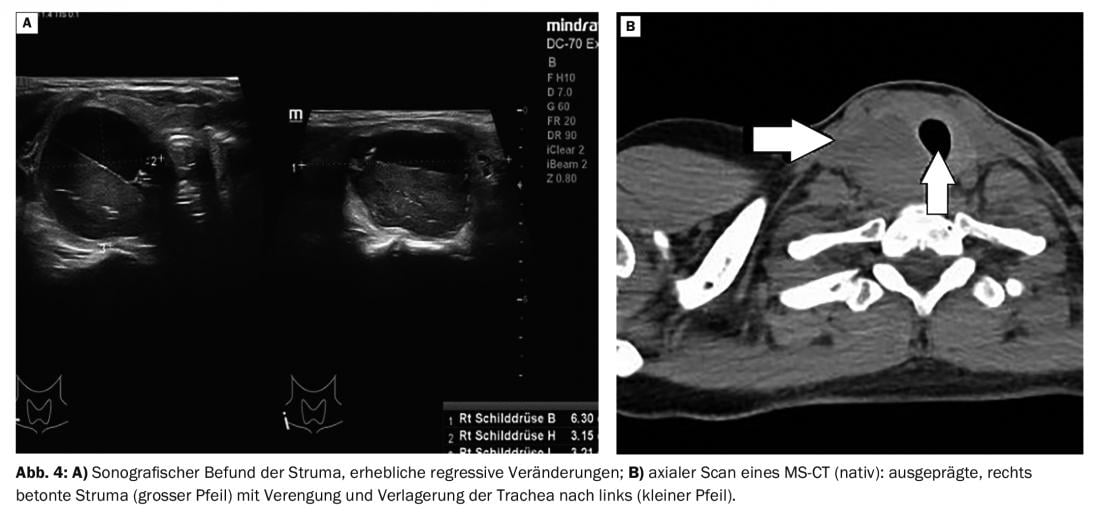
In case report 1, a 55-year-old male patient complained of swelling, pressure, and licking sensations on the right side of his neck. Scintigraphic and sonographic evidence of a large right goiter was present (Fig. 1A, B and C). Case study 2 showed a goiter (Fig. 2) with regressive changes on the left side in a 48-year-old female patient with cervical syndrome on CT. Case report 3 documents a rapid increase in the circumference of the soft tissues of the neck within one week with local pain, redness and increasing dysphagia in a 59-year-old man. Magnetic resonance imaging demonstrated extensive inflammation of the left thyroid portions with incipient abscessation (Fig. 3A, B, and C), which clinically resulted in severe disease. Case report 4 shows sonography and native CT (Fig. 4A and B) of a 41-year-old female patient with increasing right neck mass, sensation of pressure and lumpiness, and new onset of right phrenic nerve paresis. Sonographically large goiter on the right with cyst. On CT, significant impression of the trachea and displacement to the left (small arrow) by the goiter (large arrow). There was also autonomy.
Take-Home Messages
- Imaging studies alone do not provide reliable information about thyroid function.
- Clinical examination, determination of laboratory parameters and thyroid sonography and scintigraphy ensure the diagnosis of morphological and functional thyroid disease.
- MRI provides complementary information, particularly differential diagnoses to other local space-occupying lesions or inflammation.
- Thyroid enlargement with homogeneous or nodular structure may be in a euthyroid or hyperthyroid metabolic state.
- About 5% of nodular structural changes of the thyroid gland are malignant.
Literature:
- Bergmann P, Cannie M: Blood tests and imaging in thyroid pathology. Rev Med Brux 2012; 33(4): 246-253.
- Dietel M, Suttorp N, Zeitz M (eds.): Harrison’s Internal Medicine. Volume 2, 2009, 17th ed. ABW Wissenschaftsverlag Berlin: 2766.
- Liénart F, et al: Thyroid nodules: benign or malignant? Rev Med Brux 2011; 32(5): 445-452.
- Thiel HJ: Cross-sectional diagnosis of the spine (7.14). Incidental findings: struma colli. MTA Dialog 2013(6), 14: 532-534.
- Zieren HU: Thyroid enlargement. www.deutsches-schilddruesenzentrum.de, (last accessed 11.05.2022)
HAUSARZT PRAXIS 2022; 17(6): 38-41











