Heart failure often does not come alone. One third of the patients also suffer from renal insufficiency. A major challenge here is the iron deficiency that often occurs. Interdisciplinary management is required here.
Heart failure remains the fastest growing cardiovascular disease in Western industrialized countries. The prevalence among those over 45 years of age is already two percent. Despite major advances in the treatment of this disease, the prognosis has not yet improved significantly. This is partly due to one of the most common and progressive complications – renal failure. There is a close interaction between the two organs, so that the severity of renal insufficiency fluctuates with the severity of the patient’s clinical condition (Fig. 1).
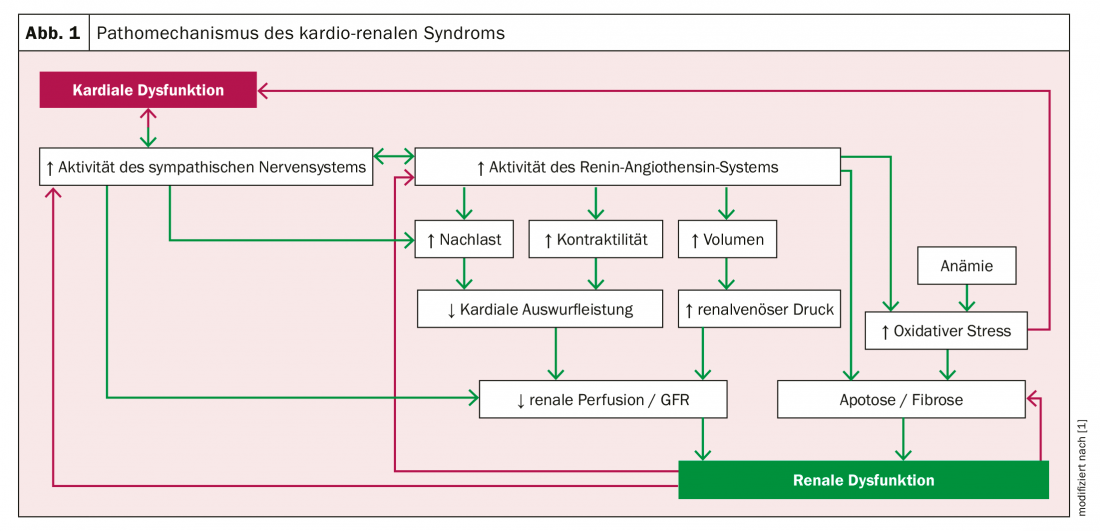
Cardio-renal patients therefore require comprehensive, interdisciplinary care to manage additional comorbidities and therapy-associated complications. The therapeutic goals in the treatment of acute heart failure are rapid stabilization of hemodynamics and symptom improvement and improvement of respiratory status. Diuretics, vasodilators, and positive inotropic agents are the focus of therapy along with general and supportive measures. By stabilizing and improving cardiac function, glomerular pressures should be improved. The therapy of acute kidney injury is based on the respective stage. In principle, the prevention or treatment of volume overload by controlled volume reduction is of central importance.
Challenge iron deficiency
One of the biggest challenges, however, is the common iron deficiency. This is also closely associated with increased mortality in the cardio-renal patient and additionally with decreased exercise capacity. Iron is not only needed for oxygen transport, but also for cellular energy production and as an essential component in numerous enzymatic metabolic processes.
European heart failure guidelines recommend i.v. therapy with ferric carboxymaltose in symptomatic patients. According to studies, this iron supplementation leads to a significant improvement in terms of heart failure-related symptoms, exercise capacity and quality of life. Recent analysis of a meta-analysis of four controlled trials demonstrated a 41% risk reduction in cardiovascular-related hospital admissions and mortality compared with placebo. Oral iron administration, on the other hand, is often poorly tolerated gastrointestinally and results in lower absorption rates.
Keeping an eye on the RAAS blockade
Drug-induced blockade of the renin-angiotensin-aldosterone system (RAAS) generally shows a positive effect in cardio-renal patients. However, many RAAS inhibitors cause a dangerous increase in serum potassium concentration. Hyperkalemia, in turn, increases the risk of hospitalization and mortality. Nevertheless, to achieve a sufficiently high RAAS inhibition, the non-absorbable, sodium-free potassium exchanger Patiromer should be used. In clinical trials, it showed a favorable benefit-risk profile and rapidly lowered potassium levels when taken daily.
Source: Heart Failure
Literature:
- Bock JS, Gottlieb SS: Cardiorenal syndrome: new perspectives. Circulation 2010; 121: 2592-2600.
CARDIOVASC 2019; 18(4): 24 (published 8/23/19, ahead of print).