Most pregnancies with epilepsy proceed without problems, but it is important to anticipate epilepsy-specific problems and to work on them together with the doctor and the patient within the framework of targeted pregnancy “management”. This review addresses these problems before and during pregnancy at birth and postpartum.
The presence of epilepsy should not be taken as a reason to refrain from having children of one’s own despite the desire to have children. Most pregnancies in epilepsy go smoothly, and most children born to mothers (and fathers) with epilepsy are born healthy and develop according to expectations. However, epilepsy-specific problems must be anticipated in the case of the desire to have children and pregnancy, and these can be dealt with jointly by the doctor and the patient as part of targeted pregnancy “management”. The present orienting overview addresses these problems in a certain chronological order: Which aspects have to be considered before pregnancy, during pregnancy and at birth and postpartum? The focus of consideration is on the constellation of epileptic (potential) mother and child, not on epilepsy-related aspects of the male desire to have a child, i.e. not on the (potential) father. Although male fertility may also be impaired by epilepsy and medication [1], and paternal epilepsy may also slightly increase the risk of epilepsy in the child [2]. But the child is exclusively exposed to maternal medications and maternal seizures during pregnancy, and the mother, but not the child’s father, must experience the interrelationships of epilepsy and pregnancy firsthand.
Fertility
Epilepsy and additionally anticonvulsant medication can reduce female fertility by 15-30% via different mechanisms [1]. However, women with epilepsy who have a manifest desire to have children and who are not previously known to have a fertility disorder do not experience delayed pregnancy compared to healthy women [3]. In most cases, pregnancy in epilepsy can be achieved as desired.
Maternal health risks
Women with epilepsy have slightly increased risks of spontaneous abortion, prenatal and postpartum hemorrhage, arterial hypertension, and delivery before 37 weeks’ gestation compared with women without epilepsy [4]. Drug-treated women with epilepsy showed a slightly increased risk of postpartum hemorrhage compared with women with untreated epilepsy [4]. In an older review study, however, no clearly epilepsy-related increased risk for gestational hypertension, preeclampsia, spontaneous abortions, perinatal death of the child, or status epilepticus of the mother had yet become apparent from the available data [5], but at least in another single study [6] an increased incidence of gestational diabetes had.
Inheritance risk
Before pregnancy, one would like to assess the risk for the occurrence of fetal epilepsy. In the rare monogenic disorders with epilepsy, special human genetic counseling should be provided in view of the sometimes quite high risk of inheritance [7]. In other epilepsies, the risk of inheritance is comparatively low. Overall, approximately 4-5% of children born to women with epilepsy also develop epilepsy [8]. In acquired epilepsies with symptomatic etiology, the risk is even lower, as expected, and in idiopathic epilepsies it increases at most to the lowest double-digit percentage by 10%.
Seizure risk during pregnancy
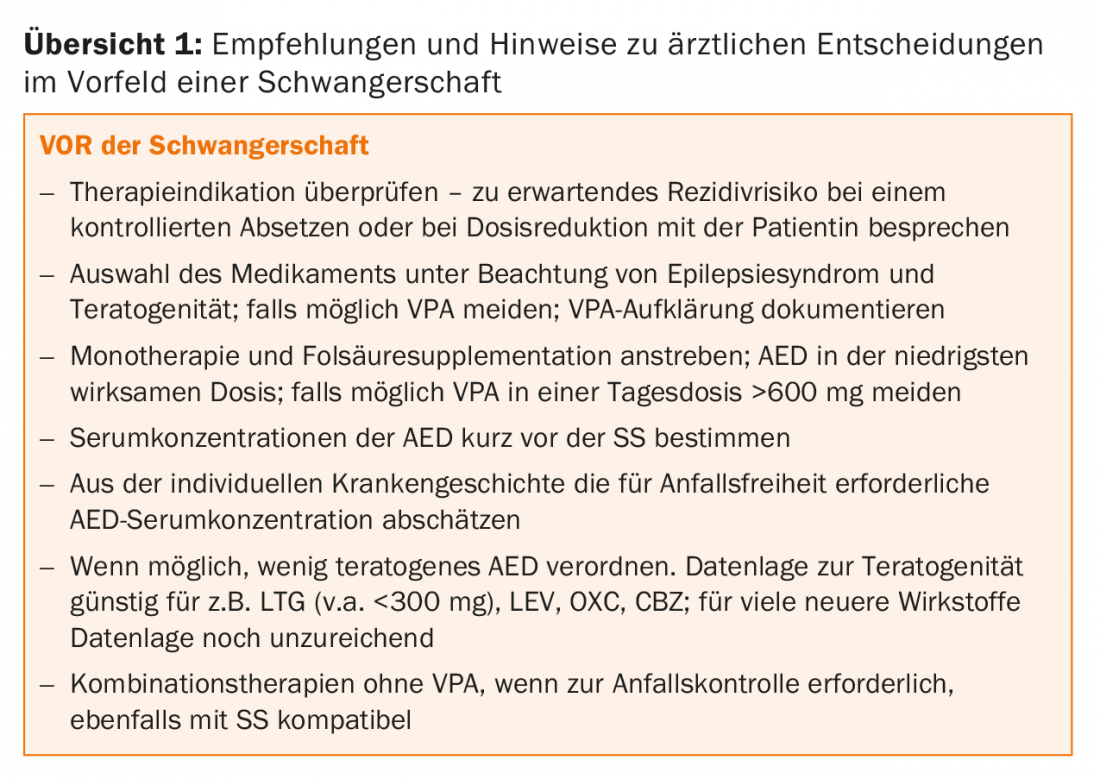
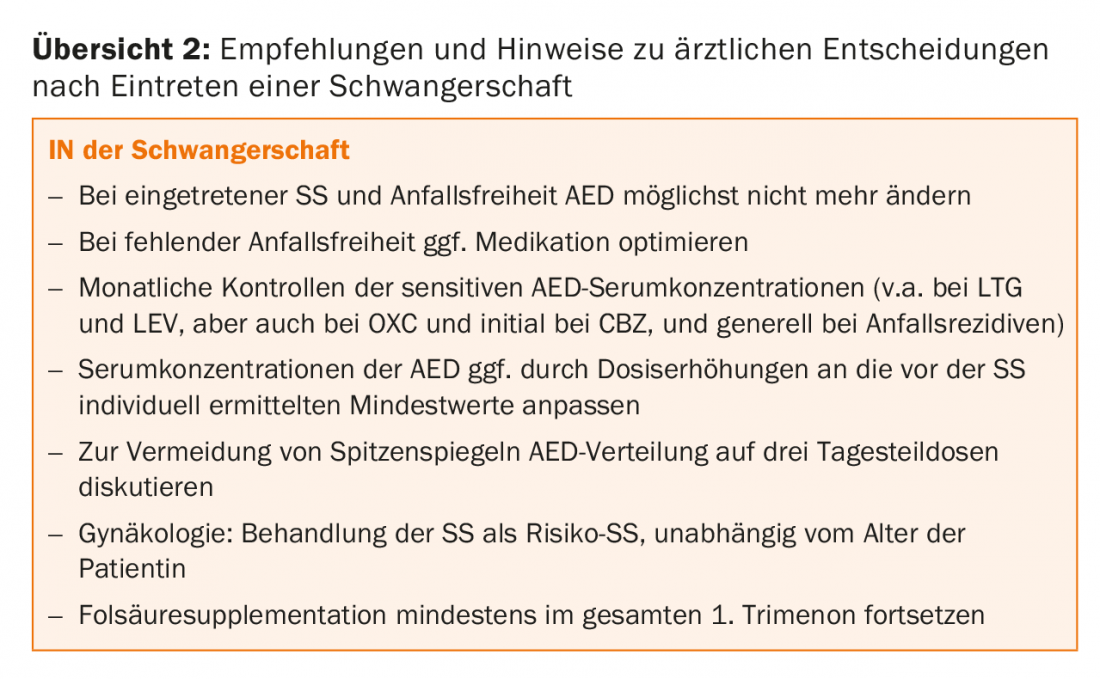
The seizure situation remains unchanged during pregnancy in approximately 54-80% of women; spontaneous improvements are reported in 3-24% and worsening in 14-32%, depending on the study [5]. Often, deteriorations are due to independent dose reductions or discontinuation of anticonvulsants. During pregnancy, the seizure situation is also less favorable in untreated epilepsies than in treated epilepsies. Drug treatment with low risk in terms of teratogenicity can avoid a relevantly increased risk of malformation compared with untreated epilepsy [9]. Since freedom from seizures for the mother must be regarded as the primary therapeutic goal in pregnancy anyway, most patients will be advised to continue anticonvulsant therapy during pregnancy. In seizure-free treated patients, dose reduction or outright discontinuation may be discussed prior to planned pregnancy based on individual assessment of seizure recurrence risk. Dose reduction may be of interest especially in monotherapies with valproate, lamotrigine, or carbamazein, as an increase in malformation rates as a function of dose level has been quite well demonstrated for these agents [10,11]. This effect is particularly dramatic with valproate, with rates ranging from well below 10% at doses of no more than 600 mg to rates of over 20% at high doses of 1500 mg and above [11]. Prior to the onset of pregnancy, seizure freedom or best possible seizure control should be documented for at least six months in the achieved treatment situation (maintenance of previous medication, switch to non-problematic agent, dose reduction, discontinuation of AED). For anticonvulsants with dose-dependent teratogenicity (e.g., valproate, carbamazepine, lamotrigine), the lowest necessary dose can be targeted before pregnancy, again with at least six months of stable medication before conception. If seizure freedom was achieved for 9-12 months before the onset of pregnancy, the chance of seizure freedom through pregnancy is also very high (84-92%) [5].
Drug treatment for pregnancy desire
The choice of anticonvulsant or anticonvulsants is determined primarily by the teratogenic risk of the agents, in addition to individual and syndrome efficacy. Infantile malformation rates are increased up to threefold in treated epilepsy patients compared to healthy untreated women [12]. Comparatively high malformation rates under monotherapy are found for valproate (depending on study and dose up to well above 10%), primidone and to a lesser extent for phenobarbital and – inconsistently – phenytoin [13,14]. With newer anticonvulsants such as lamotrigine, levetiracetam, and oxcarbazepine, malformation rates are encouragingly low at 2-4% [15,16], but can increase into the higher single-digit percentages with high-dose therapies. Other newer anticonvulsants cannot (yet) be recommended for use in pregnancy: either because of lack of data (e.g., perampanel, brivaracetam) or because of critical evidence and/or conflicting findings on malformations and birth weight (e.g., topiramate, zonisamide, pregabalin) with still insufficient data, especially for monotherapies.
In patients who are well controlled on combination anticonvulsant therapy, the question arises whether to switch to monotherapy nevertheless for pregnancy. In older studies [17], the malformation rate increased significantly with the number of agents administered. However, more recent studies with combination therapies that include newer anticonvulsants suggest that under current therapeutic conditions (with only very infrequent use of, for example, phenobarbital and primidone), increased malformation rates become apparent especially with such polytherapies that also include valproate. Combinations without valproate (e.g., with carbamazepine or lamotrigine) often do not show significantly increased rates compared with monotherapies [18]. In this respect, the earlier rule of thumb to avoid polytherapies in pregnancy if possible must be put into perspective. However, findings continue to emerge that polytherapies can also negatively impact children’s cognitive development. Since such negative cognitive effects in monotherapies have also been demonstrated primarily for valproate [19–21], in the future, polytherapies without valproate would have to be studied again specifically in more detail with regard to child cognition.
Some physicians recommend splitting high anticonvulsant doses into three daily part doses to buffer potentially teratogenic serum concentration peaks [22]. A clinically relevant effect of such measures is difficult to demonstrate. In addition, there is an increased risk of missed doses when an additional midday partial dose is introduced (forgetting the midday dose, e.g., in women who work full time).
Valproate in pregnancy?
The evidence for a (to some extent dose-dependent) [21,23] negative effect of intrauterine exposure to valproate on infant cognitive development is now clearly established, even in comparison with other and cognitively probably largely harmless agents such as levetiracetam [24], lamotrigine, and carbamazepine [21,25,26]. Also, intrauterine exposure to valproate may predispose to the development of autistic traits [27]. When these findings are read together with the high rate of malformations under therapies with valproate, the question arises whether valproate treatments should not generally be refrained from during pregnancy. In fact, epilepsy societies now advise that valproate be used in childbearing women only in exceptional circumstances. Such an exception would be given, for example, if – as is not uncommon in the presence of idiopathic generalized epilepsy – freedom from seizures can be achieved exclusively by valproate, but not by other first-line drugs. Also, one would probably no longer switch medications if pregnancy has already occurred in epilepsy that is otherwise well treated with valproate: both switching to another agent and (even more so) discontinuing valproate without replacement during pregnancy are associated with an increase in generalized tonic-clonic seizures [28]. In addition, frequent generalized tonic-clonic seizures during pregnancy are also a negative predictor of later academic performance [19]. Due to the complexity of the situation, it is now recommended that standardized educational forms and information brochures be used for decisions about valproate therapy in the affected female target group (available for Switzerland, for example, as a download at www.swissmedic.ch).
Other child health risks
Any health risk to the unborn child from maternal seizures is likely to be predominantly due to the risk of accidents to the mothers caused by seizures. Single seizures – including generalized tonic-clonic events – are unlikely to harm the child selectively; here, the higher oxygen affinity of fetal hemoglobin may be protective. Arguably, however, increased preterm birth and lowered birth weight have been reported specifically in infants born to mothers who experienced generalized tonic-clonic seizures during pregnancy [29]. No clear data are available on the risk of hypoxia-related damage from status epileptici generalized seizures or prolonged or serial grand maux.
Children of women with epilepsy generally show an increased risk of a lowered Apgar Score [30] and low birth weight [4,31]. The risk of intrauterine death (spontaneous abortion or stillbirth) may be increased with polytherapy [32], whereas this has not been clearly demonstrated for monotherapies. The risk of fetal growth retardation is slightly higher in women with epilepsy than in women without epilepsy, and likewise in drug-treated compared with untreated epilepsy [4].
The fact that “major” malformations, i.e. malformations of the heart, genitourinary system, nervous system, face and limbs requiring correction for health or cosmetic reasons, are favored by certain drug treatment constellations is considered certain [11]. Some malformations are found disproportionately frequently with certain anticonvulsants, e.g., cardiac malformations with phenobarbital or clefts with valproate [30]. It is controversial whether and to what extent epilepsy itself is also associated with an increased risk of malformation. In the positive case, one would expect an increased malformation rate even in untreated epilepsies; however, this could not be demonstrated in a larger meta-analysis [33]. On the other hand, it has been argued, especially in older studies, that (1) malformations in children of mothers with epilepsy were also known before the era of drug therapy, and (2) paternal epilepsies in healthy and anticonvulsant-untreated mothers are also associated with increased rates of malformation in the shared children [34]. It is possible that the so-called minor malformations, i.e. the generally minor deviations not requiring correction, such as discrete dysmorphia, microcephaly, etc., are somewhat more common in children of parents with epilepsy, even independently of the medication, while the major malformations are more likely to be favored by the anticonvulsants.
Folic acid supplementation during pregnancy
There is at least weak evidence for a reduction in malformation rates with folic acid supplementation of 0.4-5 mg per day through the first trimester (thus, supplementation should be started before conception) [35]. In this dose range, adverse folic acid effects should not yet occur [36]. Supplementation with 5 mg per day has become common in epileptology, although the specific effect of this relatively high dose is difficult to demonstrate [37]. Recently, there is also evidence for a reduced risk of developing autistic traits through folic acid supplementation [38], and for a possible positive effect on later intelligence development [21].
Dose adjustments of anticonvulsants
During pregnancy, the serum concentrations of some anticonvulsants must be checked regularly, as relevant reductions in serum concentrations may occur due to hormonal interactions and changes in pharmacokinetics, among other factors, and thus seizure recurrences may occur. This includes lamotrigine, levetiracetam, oxcarbazepine, phenytoin, phenobarbital, topiramate, and zonisamide [39,40]. In the case of lamotrigine, the effect of increased clearance due to activated glucuronidation (estrogen) may be added, so that gradual dose increases up to approximately twice the initial dose are often made for this agent to maintain the required serum concentration. Because high-dose therapy is usually not achieved until the second or third trimester, such dose increases appear reasonable. It can be difficult to answer the question of which serum concentration to aim for on an individual basis. Especially for lamotrigine, possibly also for oxcarbamazepine and for levetiracetam, it is often possible to extract such a “guideline value” from the individual medical history (serum concentrations postictal in previous seizures? Serum concentrations in the seizure-free phase?) such a “guideline value” can be extracted, which can then be used as a basis for therapy management during pregnancy.
In general, a pregnancy with epilepsy should be treated as a high-risk pregnancy by gynecology or obstetrics with the appropriate monitoring measures including Fine ultrasound examinations at the scheduled time points.
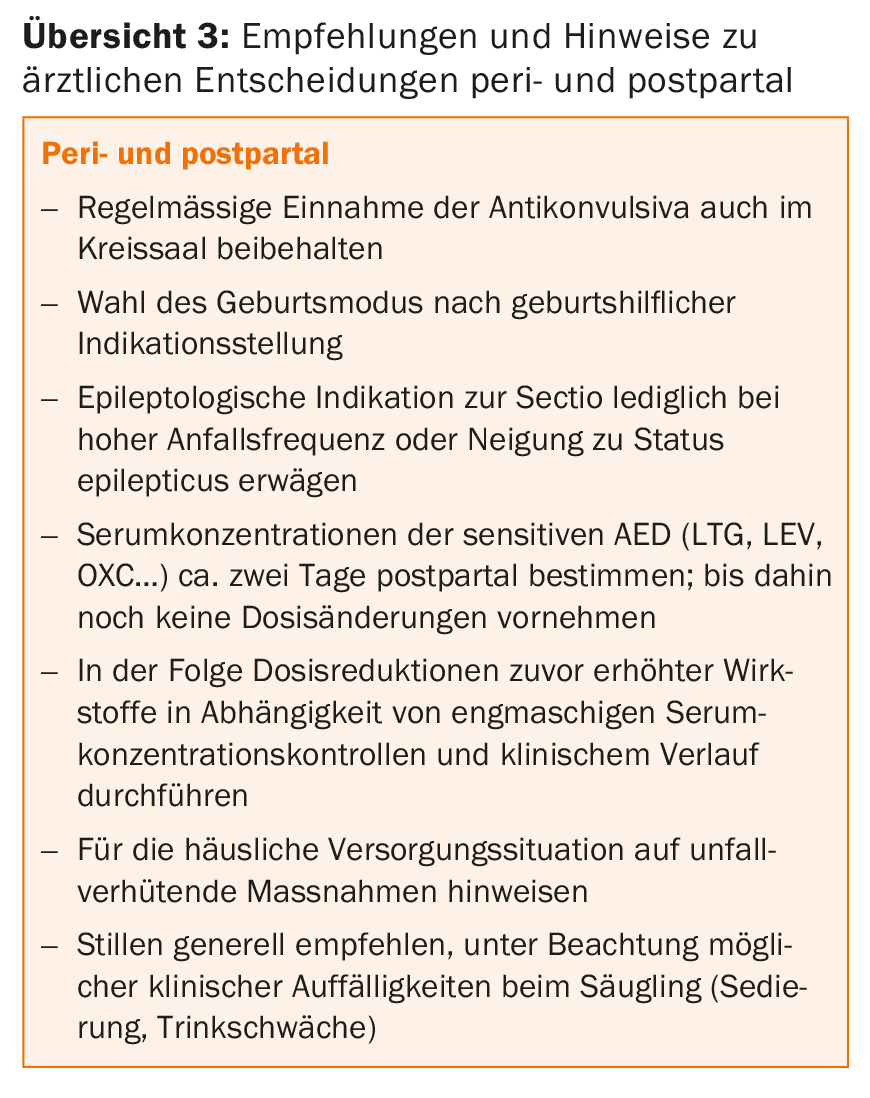
Birth and postpartum period
Peripartum, the risk of seizures is slightly increased in female epilepsy patients. Factors such as sleep deprivation, irregular medication, and emotional and physical stress likely play a role. However, routine administration of anticonvulsant on-demand medication during delivery is not recommended unless a very high seizure frequency is already known.
The mode of delivery can be chosen primarily according to individual obstetric criteria. The presence of epilepsy does not provide a separate indication for a sectio. At most, in cases of very high seizure frequency or known tendency to status epileptici, sectio may be chosen for epileptological indication.
Vitamin K administration to the newborn is performed according to current recommendations [41]. Additional prepartum vitamin K administration to the pregnant woman is therefore only necessary for epileptological indications in the case of combination therapies with several enzyme inducers or in the case of epilepsy-related premature delivery before the 37th week of gestation.
Postpartum maternal anticonvulsant serum concentrations should be checked, especially if dose adjustments have been made during pregnancy. Concentrations of lamotrigine, levetiracetam, and other previously elevated agents can increase, sometimes massively, in the first postpartum weeks, resulting in signs of overdose in the mother and, in the case of breastfeeding, possibly in the infant. Unfortunately, a fixed schedule for postpartum dose reductions with the goal of reaching the prepartum dose cannot be given because the courses are very different. The continuation of the last prepartum dose in the first two postpartum days has proven to be effective, followed by gradual dosage reductions according to close-meshed serum concentration determinations over the next weeks and months. In the case of lamotrigine therapy, even weekly serum concentration determinations are initially helpful postpartum in order to avoid overly cautious but also excessive and hasty dose reductions.
In the home environment, most epilepsy patients are fully capable of caring for newborns independently, provided that they are given this role in the family division of responsibilities. Overly rigid and extensive caregiving restrictions due to epilepsy place stress on the mother and the mother-child interaction. Nevertheless, especially for mothers who are not seizure-free, a few simple rules of conduct should be followed to prevent accidents:
- The mother should not bathe the child unaccompanied because of the risk of drowning during seizures.
- As a precaution, tasks such as changing diapers etc. should be done on the floor, not in an elevated position (risk of falling off the changing table).
- Carrying the child in the arm should preferably be done in a sitting rather than standing position, if possible (risk of falling due to seizures).
Breastfeeding
In general, children of treated epilepsy patients do not have to miss out on the benefits of breastfeeding. The common anticonvulsants differ greatly with regard to the expected infant serum concentrations, which, incidentally, cannot simply be derived from the anticonvulsant concentrations in breast milk [42], since they also depend on the infant’s metabolism. Relatively high serum concentrations in the child may result from breastfeeding under phenobarbital, primidone, and ethosuximide, and to a lesser extent under lamotrigine and possibly zonisamide [43]. Overall, the data on the clinical effects of breastfeeding in drug-treated epilepsies are still insufficient [44]. The agents classified as “safe” or recommended are primarily those whose pharmacokinetics are known and unproblematic and for which no or only minor adverse effects (sedation, weakness in drinking, lack of weight gain) are reported in infants in an adequate number of studies. In a recent review, levetiracetam, carbamazepine, phenobarbital, primidone, and valproate were classified as largely unproblematic, and lamotrigine as usable with reservations, oxcarbazepine, phenytoin, ethosuximide, vigabatrin, topiramate, pregabalin, gabapentin, and zonisamide, and clobazam, mesuximide, rufinamide, felbamate, lacosamide, sultiam, and perampanel [45] as not recommended. In another review [43] carbamazepine, valproate, phenytoin were classified as “safe”, as “largely safe” lamotrigine, oxcarbazepine, levetiracetam, topiramate, gabapentin, pregabalin, vigabatrin, as “potentially risky” phenobarbital, primidone, ethosuximide, felbamate, zonisamide and benzodiazepines (with quite insufficient data for: Perampanel, Lacosamide, Brivaracetam).
Such classifications remain partly theoretical, since among the less problematic active ingredients there are many whose use is generally hardly common (e.g. primidone, phenobarbital, phenytoin) or is not recommended in pregnancy anyway (e.g. valproate, topiramate), so that they will probably not be used in the breastfeeding period either. Thus, the fact that an active ingredient is rated as “safe” or “compatible” does not necessarily mean that it is specifically recommended for breastfeeding.
Data regarding adverse cognitive effects on the infant from postpartum anticonvulsant uptake via breastfeeding still need improvement. Previous studies [46,47] have identified positive rather than negative cognitive effects of breastfeeding among commonly used anticonvulsants; also, an additional negative effect of valproate was not shown for exposure prolonged by breastfeeding.
Conclusion
An unproblematic pregnancy and a good postpartum development of the child are the rule, not the exception, even in epilepsy patients. The epilepsy-specific aspects of treatment and pregnancy management should be adequately addressed in the trialogue between the patient, gynecologist, and epileptologist through all phases. Epileptologic pregnancy planning begins well before conception with preconception counseling of the patient, adjustment to the most pregnancy-compatible medication possible, and initiation of preconceptional folic acid supplementation when pregnancy planning is concrete.
Take-Home Messages
- Even in the presence of epilepsy, most pregnancies proceed without problems for mother and child, adequate therapy planning
- and monitoring are required.
- Prior to the onset of a planned pregnancy, anticonvulsant medication should be established at the lowest possible dose; maternal freedom from seizures remains the primary therapeutic goal.
- If possible, therapies containing valproate should be avoided. In the absence of valproate, combination therapies with current agents are associated with a lower risk of malformation than previously thought.
- The active substances that have been proven to be beneficial for pregnancy are primarily lamotrigine, levetiracetam, carbamazepine and oxcarbazepine, if possible in low daily doses.
- Drug-treated epilepsy patients can breastfeed their children, taking into account possible undesirable effects, which are mainly recognizable by sedation, weakness in drinking and lack of weight gain of the child.
Literature:
- Herzog AG: Disorders of reproduction in patients with epilepsy: Primary neurological mechanisms. Seizure 2008; 17: 101-110.
- Ottman R, et al: Higher risk of seizures in offspring of mothers than of fathers with epilepsy. Am J Hum Genet 1988; 43(3): 257-264.
- Pennell PB, et al: Fertility and birth outcomes in women with epilepsy seeking pregnancy. JAMA Neurol 2018 [E-Pub ahead of Print]
- Viale L, et al: Epilepsy in pregnancy and reproductive outcomes: a systematic review and meta-analysis. Lancet 2015; 386: 1845-1852.
- Harden CL, et al: Management issues for women with epilepsy – Focus on pregnancy (an evidence-based review): I. Obstetrical complications and change in seizure frequency. Epilepsia 2009; 50(5): 1229-1236.
- Katz O, et al: Pregnancy and perinatal outcome in epileptic women: a population-based study. J Matern Fetal Neonatal Med 2006; 19(1): 21-25.
- Helbig I, et al.: Primer Part I – The building blocks of epilepsy genetics. Epilepsia 2016; 57(6): 861-868.
- Pirker S: Women with epilepsy: 7 important aspects. Clin Neurophysiol 2005; 43: 138-143.
- Vajda FJE, et al: The outcomes of pregnancy in women with untreated epilepsy. Seizure 2015; 24: 77-81.
- Morrow J, et al: Malformation risks of antiepileptic drugs in pregnancy: a prospective study from the UK Epilepsy and Pregnancy Register. J Neurol Neurosurg Psychiatry 2006; 77: 193-198.
- Tomson T, Battino D: Teratogenic effects of antiepileptic drugs. Lancet Neurol 2012; 11: 803-813.
- Meador K, et al: Pregnancy outcomes in women with epilepsy: a systematic review and meta-analysis of published pregnancy registries and cohorts. Epilepsy Res 2008; 81(1): 1-13.
- Kaneko S, et al. Congenital malformations due to antiepileptic drugs. Epilepsy Res 1999; 33: 145-158.
- Hernandez-Diaz S, et al: Comparative safety of antiepileptic drugs during pregnancy. Neurology 2012; 78: 1692-1699.
- Tomson T, et al. Comparative risk of major congenital malformations with eight different antiepileptic drugs: a prospective cohort study of the EURAP registry. Lancet Neurol 2018; 17: 530-538.
- Molgaard-Nielsen D, Hviid A: Newer-generation antiepileptic drugs and the risk of major birth defects. JAMA 2011; 305: 1996-2002.
- Nakane Y, et al. Multi-institutional study on the teratogenicity and fetal toxicity of antiepileptic drugs: a report of a collaborative study group in Japan. Epilepsia 1980; 21: 663-680.
- Vajda FJE, et al: The teratogenic risk of antiepileptic drug polytherapy. Epilepsia 2010; 51(5): 805-810.
- Adab N, et al: The longer term outcome of children born to mothers with epilepsy. J Neurol Neurosurg Psychiatry 2004; 75: 1575-1583.
- Gaily E, et al: Normal intelligence in children with prenatal exposure to carbamazepine. Neurology 2004; 62: 28-32.
- Meador KJ, et al: Fetal antiepileptic drug exposure and cognitive outcomes at age 6 ys (NEAD study): a prospective observational study. Lancet Neurol 2013; 12: 244-252.
- Pennell PB: Pregnancy in women who have epilepsy. Neurol Clin 2004; 22: 799-820.
- Baker GA, et al: IQ at 6 years after in utero exposure to antiepileptic drugs. Neurology 2015; 84: 382-390.
- Shallcross R, et al: Child development following in utero exposure. Neurology 2011; 76: 383-389.
- Bromley RL, et al: Early cognitive development in children born to women with epilepsy: A prospective report. Epilepsia 2010; 51(10): 2058-2065.
- Nadebaum C, et al: Language-skills of school-aged children prenatally exposed to antiepileptic drugs. Neurology 2011; 76: 719-726.
- Roullet FI, et al. In utero exposure to valproic acid and autism – a current review of clinical and animal studies. Neurotoxicol Teratol 2013; 36: 47-56.
- Tomson T, et al: Withdrawal of valproic acid treatment during pregnancy and seizure outcome: Oberservations from EURAP. Epilepsia 2016; 57(8): 173-177.
- Rauchenzauner M, et al: Generalized tonic-clonic seizures and antiepileptic drugs during pregnancy – a matter of importance for the baby? J Neurol 2013 ; 260(2) : 484-488.
- Harden CL, et al: Management issues for women with epilepsy – Focus on pregnancy (an evidence-based review): II. teratogenesis and perinatal outcomes. Epilepsia 2009; 50(5): 1237-1246.
- Yerbi M, et al. Pregnancy complications and outcomes in a cohort of women with epilepsy. Epilepsia 1985; 26(6): 631-635.
- Tomson T, et al: Antiepileptic drugs and intrauterine death: A prospective observational study from EURAP. Neurology 2015; 85(7): 580-588.
- Fried S, et al: Malformation rates in children of women with untreated epilepsy: a meta-analysis. Drug Saf 2004; 27(3): 197-202.
- Janz D: On the risk of malformations and developmental disorders in children of parents with epilepsy. Neurologist 1979; 50: 555-562.
- Harden CL, et al: Management issues for women with epilepsy – Focus on pregnancy (an evidence-based review): III. vitamin K, folic acid, blood levels, and breast-feeding. Epilepsia 2009; 50(5): 1247-1255.
- Asadi-Pooya AA: High dose folic acid supplementation in women with epilepsy: Are we sure it is safe? Seizure 2015; 27: 51-53.
- Ban L, et al: Congenital anomalies in children of mothers taking antiepileptic drugs with and without periconceptional high dose folic acid use: A population-based cohort study. PloS 2015; 10(7) Jul 6: e0131130.
- Bjork M, et al: Association of folic acid supplementation during pregnancy with the risk of autistic traits in children exposed to antiepileptic drugs in utero. JAMA Neurol 2018; 75(2): 160-168.
- Reimers A: New antiepileptic drugs and women. Seizure 2014; 23: 585-591.
- Tomson T, et al: Antiepileptic drug treatment in pregnancy: changes in drug disposition and their clinical implications. Epilepsia 2013; 54(3): 405-414.
- Schubiger G, et al: Vitamin K prophylaxis in newborns: New recommendations. Paediatrica 2002; 13(6): 54-55.
- Chen L, et al: Is breast-feeding of infants advisable for epileptic mothers taking antiepileptic drugs? Psychiatry and Clinical Neurosciences 2010; 64: 460-468.
- Veiby G, et al: Epilepsy and recommendations for breastfeeding. Seizure 2015; 28: 57-65.
- Van der Meer DH, et al: Lactation studies of anticonvulsants: a quality review. Br J Clin Pharmacol 2014; 79(4): 558-565.
- Crettenand M, et al: Antiepileptic drugs during breastfeeding. Neurologist 2018; [Epub ahead of print]
- Veiby G, et al: Early child development and exposure to antiepileptic drugs prenatally and through breastfeeding. A prospective cohort study on children of women with epilepsy. JAMA Neurol 2013; 70(11): 1367-1374.
- Meador KJ, et al: Breastfeeding in children of women taking antiepileptic drugs. JAMA Pediatr 2014; 168(8): 729-736.
InFo NEUROLOGY & PSYCHIATRY 2018; 16(5): 18-24.