Patients with type 2 diabetes have a greatly increased risk of developing cardiovascular disease compared to healthy people in the same age group. The current guidelines published in the European Heart Journal
on the management of cardiovascular disease of the European Society of Cardiology (ESC) contain some important adjustments, including a new risk score and the recommendation to switch therapy to SGLT-2 inhibitors or GLP-1 receptor agonists for all patients with type 2 diabetes and existing cardiovascular disease.
“Patients with type 2 diabetes have a two to four times higher risk of coronary heart disease, stroke, heart failure, atrial fibrillation and peripheral artery disease than patients without type 2 diabetes, and if cardiovascular disease occurs, the prognosis is worse. For example, mortality from cardiovascular disease is 50-90% higher in patients with heart failure and diabetes than in patients with heart failure alone. Therefore, specific recommendations are needed for the prevention and treatment of cardiovascular disease in patients with diabetes. Interdisciplinary, patient-oriented care is essential to reduce morbidity and mortality and improve quality of life,” says the chairman of the guideline task force, Prof. Nikolaus Marx, MD, Director of the Department of Cardiology, Angiology and Internal Intensive Care Medicine, Aachen University Hospital [1,2]. Based on the current data situation, previous recommendations for action have been adapted and updated.
SCORE-2 diabetes for risk assessment
It is estimated that 25-40% of patients with cardiovascular disease (CVD) have undiagnosed diabetes. As the presence of both diseases has a significant impact on prognosis and treatment, the guidelines recommend systematic screening for diabetes in all patients with CVD. It is equally important to screen all patients with diabetes for the risk and presence of CVD.
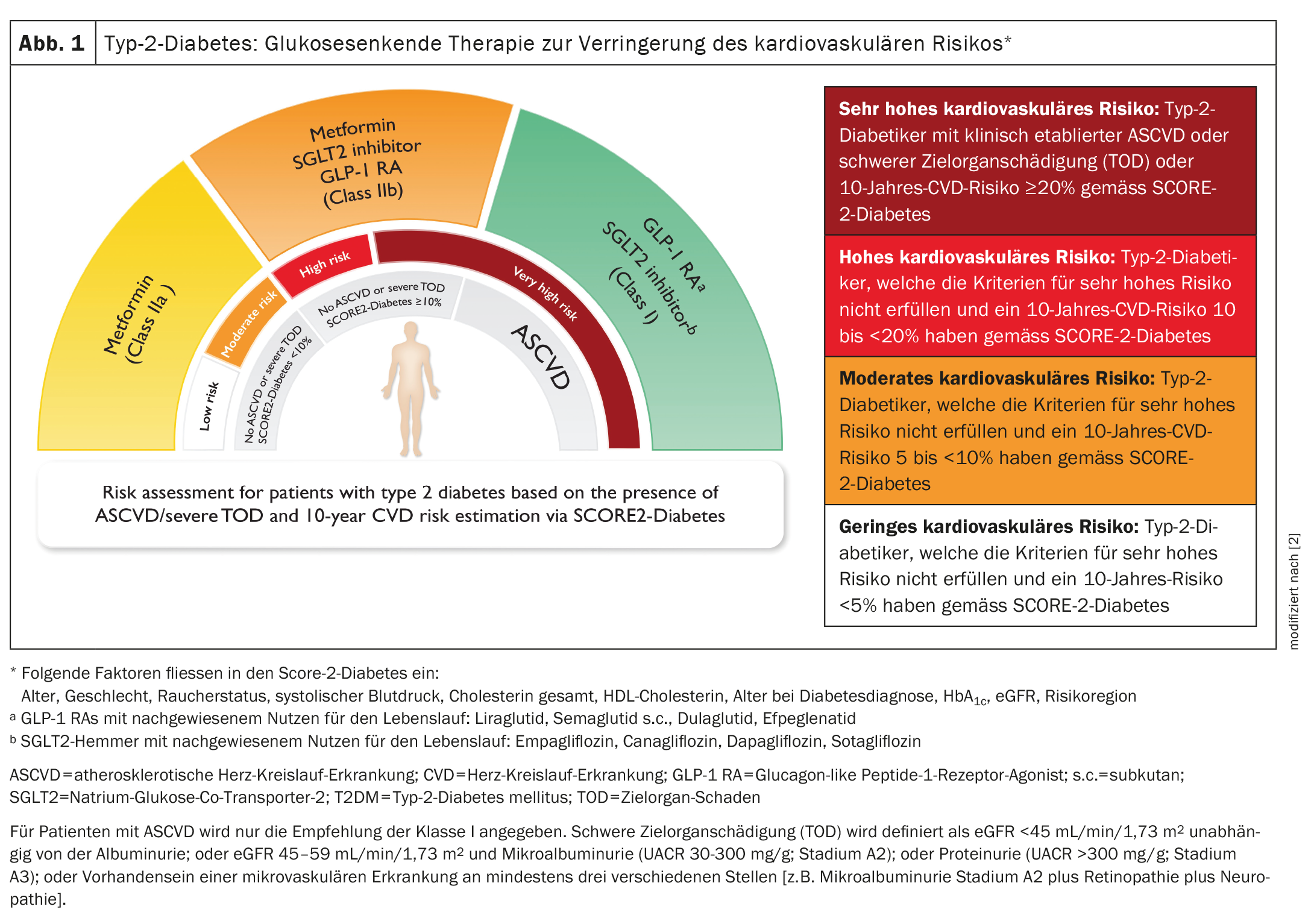
The guidelines introduce a new tool, SCORE-2-Diabetes, which can be used to estimate the 10-year risk of fatal and non-fatal myocardial infarction and stroke in patients with type 2 diabetes. The score classifies patients as low, medium, high or very high risk based on conventional CVD risk factors (age, smoking, blood pressure, cholesterol) and diabetes-specific information (age at diagnosis, blood glucose level, kidney function).
Important recommendations at a glance
The guidelines recommend that all diabetes patients consider lifestyle factors to reduce the likelihood of CVD. For overweight patients, weight reduction is one of the cornerstones of treatment. All diabetics should stop smoking and eat a diet high in unsaturated fatty acids (e.g. Mediterranean diet) to reduce cardiovascular risk. In addition, physical activity of 150 minutes of moderately intensive or 75 minutes of intensive exercise per week is recommended.
The recommendations for patients with diabetes and existing cardiovascular disease have been revised based on the results of large clinical trials (Fig. 1). The guidelines now recommend SGLT-2 inhibitors and/or GLP-1 receptor agonists to reduce the risk of heart attack and stroke in all patients with diabetes and CVD, regardless of glycemic control and concomitant glucose-lowering medication and in addition to standard therapies such as antiplatelet agents, antihypertensive drugs and lipid-lowering drugs. “Just as the presence of type 2 diabetes determines the prescription of other cardioprotective therapies, such as statins, regardless of glycemic considerations, this should now also apply to the prescription of SGLT-2 inhibitors and/or GLP-1 receptor agonists,” said the chair of the guideline task force, Professor Massimo Federici, Director of the Center for Atherosclerosis at the University of Rome [1,2].
Screening for heart failure, atrial fibrillation and kidney damage
A particular focus of the guidelines is the management of heart failure. Diabetics have a two to four times higher risk of developing heart failure than patients without diabetes, and many do not know if they have heart failure. The guidelines recommend systematic screening for signs and symptoms of heart failure at every clinical examination to enable the early use of life-saving therapies. Based on data from large clinical trials, the guidelines recommend that diabetics with chronic heart failure receive SGLT-2 inhibitors to reduce the likelihood of hospitalization for heart failure or cardiovascular death.
Diabetes-related kidney damage is one of the main causes of chronic kidney disease (CKD) worldwide. In patients with diabetes, CKD is associated with a high risk of kidney failure and cardiovascular disease. The guidelines recommend that patients with diabetes should be screened for CKD at least once a year by measuring the glomerular filtration rate and the albumin level in the urine. Patients who have both type 2 diabetes and chronic kidney disease should receive an SGLT-2 inhibitor and/or finerenone, as these agents reduce the risk of cardiovascular disease and kidney failure in addition to standard treatment.
Every year with diabetes increases the risk of atrial fibrillation by 3%, which increases the likelihood of stroke, heart failure and death. For the first time, the guidelines recommend opportunistic screening for atrial fibrillation by pulse measurement or electrocardiogram in patients with diabetes aged 65 and over. Opportunistic screening is also recommended for people under the age of 65, particularly if other risk factors such as high blood pressure are present. Another new recommendation is that all patients with diabetes should have their blood pressure measured regularly in order to detect and treat hypertension and thus reduce the risk of cardiovascular disease.
Literature:
- “Recommendations to reduce cardiovascular risk in patients with diabetes published today”, European Society of Cardiology (ESC), August 25, 2023.
- Marx N, et al: ESC Scientific Document Group. 2023 ESC Guidelines for the management of cardiovascular disease in patients with diabetes. Eur Heart J 2023 Oct 14; 44(39): 4043-4140.
FAMILY PHYSICIAN PRACTICE 2024; 19(1): 32-33