For the first time ever, a randomized trial compares a catheter-based procedure with standard therapy for pulmonary embolism. The treatment option appears promising, according to data from the ULTIMA trial presented at the ACC Annual Meeting in San Francisco.
For the past two years, an ultrasound catheter has been used in Bern for the treatment of pulmonary embolism, combining the local use of thrombolytic agents with a mechanical thrombolytic procedure. With success, as shown by the results of the ULTIMA study announced in Cardiology Update and presented at the annual meeting of the American College of Cardiology (ACC) in San Francisco.
The ULTIMA (Ultrasound Accelerated Thrombolysis in Pulmonary Embolism) study compared ultrasound-assisted thrombolysis with i.v. heparin therapy alone in patients with symptomatic pulmonary embolism. Of the 363 patients hospitalized with pulmonary embolism between November 2010 and January 2013, 59 patients met eligibility requirements for the phase II study. This included a hemodynamically largely stable, radiologically confirmed, paracentral or central pulmonary embolism and a dilated right ventricle with an RV/LV ratio >1.
After randomization, 29 patients received the previous standard treatment with i.v. heparin. The remaining 30 subjects were administered an additional 10 mg of rtPA per ultrasound catheter over 15 hours. The primary endpoint of the study was the decrease in RV/LV ratio.
As the results showed 24 hours after the start of treatment, the RV/LV ratio had decreased from 1.28 to 0.99 under ultrasound-assisted thrombolysis, compared with a reduction from 1.20 to 1.17 under standard treatment (Fig. 1).
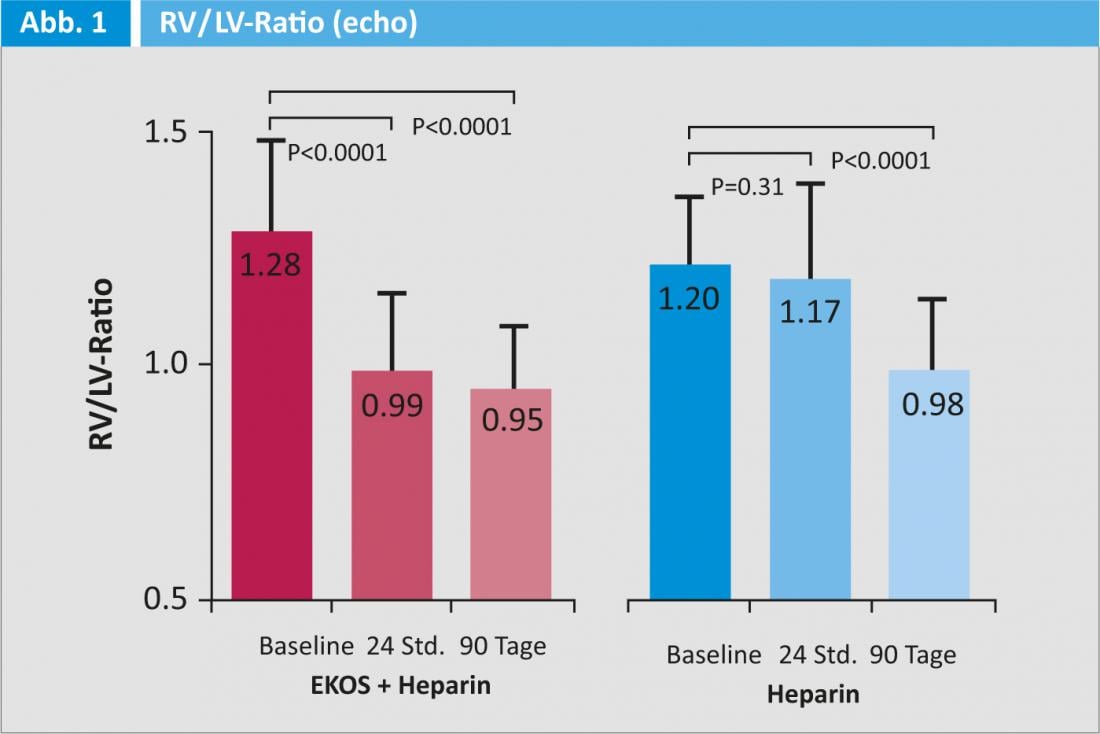
After 90 days, the RV/LV ratio was similar in the two groups. However, the difference from baseline was still significantly greater in the intervention group (0.38 versus 0.22). Although more subjects in the intervention group initially had severe right ventricular dysfunction, they recovered more rapidly than those in the heparin group. Regarding the safety of the compared therapeutic strategies, no serious bleeding was observed in either the intervention or the control group. Interestingly, despite the relatively low bleeding risk, the reduction in RV/LV ratio observed with ultrasound-assisted thrombolysis was comparable to that observed with high-dose systemic lysis.
Source: ACC Annual Meeting in San Francisco, March 9-11, 2013.











