Actinic keratosis is already one of the most frequent clinical pictures in dermatological oncology. However, due to increasing life expectancy, a further increase in the number of affected patients can be assumed. For the first time, an S3 guideline has now been published that makes recommendations for diagnosis and therapy.
Based on the S2k guideline on squamous cell carcinoma and the S1 guideline on actinic keratosis (AK), the German Dermatological Society (DDG), the Working Group of Dermatological Oncology (ADO) and the German Cancer Society (DKG) have developed the new S3 guideline “Actinic keratosis and squamous cell carcinoma of the skin”. The guideline, published this summer, is based on results of a systematic literature search and review through 2018 and reflects the evidence- and consensus-based recommendations of the interdisciplinary panel.
Clinical diagnostics
The diagnosis of AK is basically made by clinical examination and inspection of the affected area. In addition, dermoscopy, confocal laser microscopy and optical coherence tomography are performed if required. In case of unclear appearance, necessary differential diagnosis (e.g. Bowen’s disease) or resistance to therapy, a biopsy should be performed. Data for prognostic factors, i.e., predicting which AK lesion will develop and how and how quickly it will progress to squamous cell carcinoma, are still insufficient. Further research is needed here to be able to make clear statements. For lack of alternatives, the Olsen classification is therefore currently still used.
Early and consistent treatment indicated
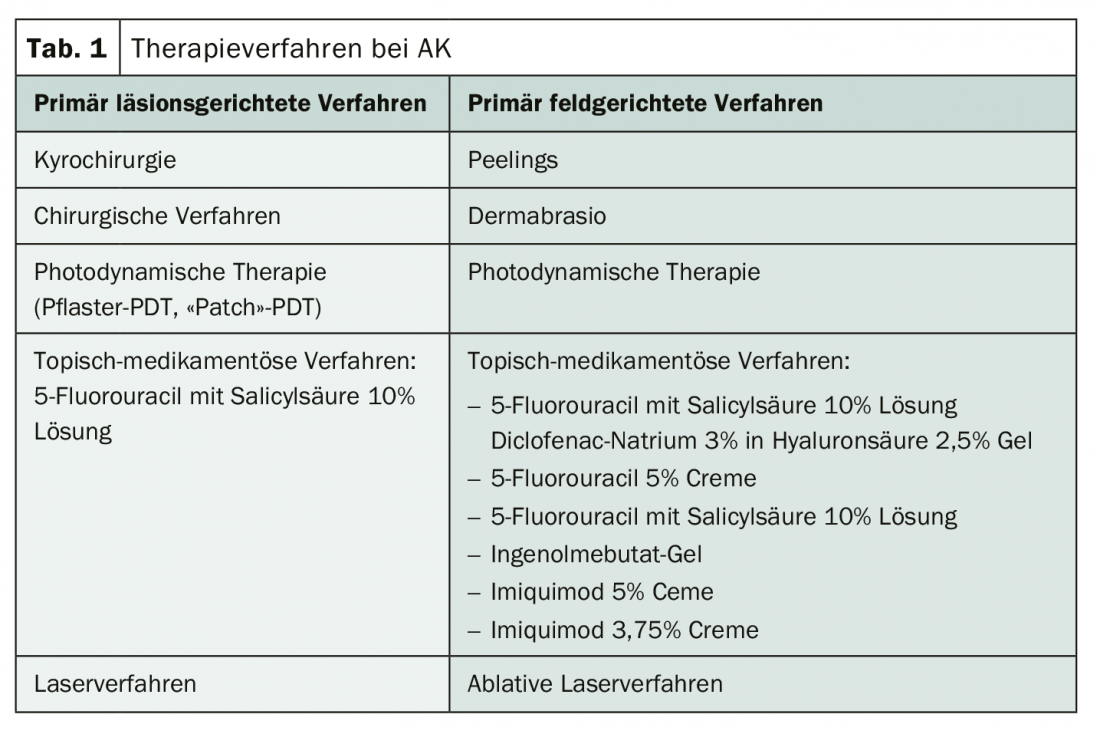
Since progression cannot be predicted, therapy should be given early and consistently. Several options are available based on the number and distribution of lesions as well as patient-related factors such as age, treatment preference, comorbidities, and risks. Particular attention should be paid especially to the field chancellery. According to the guideline, this comprises an area of skin with multiple AKs surrounded by visible UV-related skin damage. For this purpose, exclusive destruction of visible individual lesions would not be sufficient (Tab. 1). In addition to monotherapies, treatment combinations are also used. However, these have not yet been extensively studied systematically. Therefore, there are isolated possible concepts, but an algorithm is still missing. The use of UV protection products is recommended as a preventive measure and a sensible supplement to all therapy concepts.
Further reading:
- www.awmf.org/uploads/tx-szleitlinien/032-022OLI_S3_Aktinische_Keratosen-Plattenepithelkarzinom-PEK_2019-07.pdf
InFo ONCOLOGY & HEMATOLOGY 2019; 7(6): 22.