A large proportion of Parkinson’s patients suffer from the sporadic form of the disease, in which no gene mutations can be detected. However, in order to develop drugs using cell line and animal models, the much rarer hereditary Parkinson’s disease has been studied so far. Until now. Now there are first promising findings also on the sporadic form of the disease.
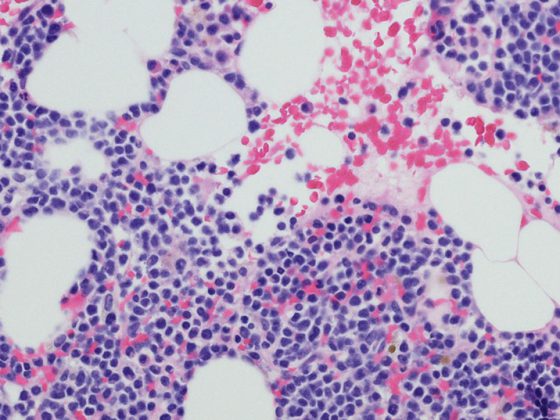
Parkinson’s disease is the second most common neurodegenerative disease after Alzheimer’s dementia, with a prevalence of about 1% of the >60-year-old population and about 15,000 patients in Switzerland. Due to shifts in the age pyramid, the number of disease cases is growing faster than for any other neurodegenerative disease. Death of dopaminergic neurons causes a lack of dopamine, which triggers the typical symptoms such as tremor, rigor or bradykinesis. In addition, there are non-motor complaints that can manifest themselves sensory, autonomic, cognitive and emotional (Fig. 1) . In the majority of cases, the idiopathic form of the disease is present, which is described by Lewy body pathology and is slowly progressive. In approximately 5-10% of affected individuals, a defined monogenic mutation can be detected, causing the mutant protein α-synuclein to be deposited in dopaminergic neurons, ultimately leading to neuronal death. Three autosomal-dominant (PARK-LRRK2, PARK-SNCA, PARK-VPS35) and three autosomal-recessive (PARK-Parkin, PARK-PINK1, PARK-DJ1) inherited genes have now been verified, the mutations of which may lead to the disease.

The disease is primarily diagnosed clinically. Therefore, an MRI should be performed at least once to rule out causes of secondary PD. The diagnosis can be confirmed using imaging techniques in which the synapse density of dopaminergic neurons can be visualized. However, the two forms of Parkinson’s cannot always be distinguished clinically. If monogenic PD is suspected, genetic testing should be used. Alterations in the Parkin and PINK1 genes should be considered especially in patients with disease onset before 40 years of age and in patients with a positive family history.
Maintain independence, alleviate discomfort
The aim of a comprehensive therapy should be to maintain the independence of the affected person as long as possible, to prevent a need for care and to avoid comorbidities. The pharmacological portfolio is now broad and can effectively alleviate motor symptoms in particular. These include the monoamine oxidase B inhibitors (MAO-B inhibitors). Safinamide, rasagiline, or selegiline increase the concentration of dopamine at the dopaminergic synapse by inhibiting degradation and have shown few side effects in pivotal trials. Dopamine agonists replace dopamine directly at the postsynaptic receptor in the striatum and are usually used in a sustained-release form (e.g., piribedil, pramipexole, ropinirole). However, orthostatic hypotension, hallucinosis, pathological daytime sleepiness, leg edema, or impulse control disorders may occur. COMT inhibitors, such as entacapone or opicapone, inhibit a degradation pathway of L-dopa, increasing its concentration in the CNS. They can increase any dopaminergic side effects. L-dopa combined with a decarboxylase inhibitor (benserazide, carbidopa) is converted to dopamine in the CNS, making it available as a transmitter with excretion and reuptake at the synaptic cleft. Nausea, nausea, hypotension, and fatigue may occur during initial therapy. NMDA antagonists and anticholinergics influence the neurotransmitters downstream of dopamine and thus have a positive effect on their balance.
Which preparation is suitable depends on the individual circumstances of the patient. The age, life circumstances, stage of the disease, symptoms and possible concomitant diseases should be taken into account in order to achieve the optimal treatment for the affected person.
Further reading:
- Borsche M, Klein C: Parkinson’s disease. medical genetics 2018; 30: 267-273.
- www.fz-juelich.de/ibi/ibi-7/DE/Forschung/Themen/07MorbusParkinson/parkinson_node.html (last accessed on 05.08.2020)
- Deuschl G, Berg D: Parkinson’s disease: how to control motor symptoms. Dtsch Arztebl 2019; 116(37): [4].
- Laperle AH, Sances S, Yucer N, et al: iPSC modeling of young-onset Parkinson’s disease reveals a molecular signature of disease and novel therapeutic candidates. Nat Med 2020 Jan 27. doi: 10.1038/s41591-019-0739-1. [Epub ahead of print]
- Mullin S, Smith L, Lee K, et al: Ambroxol for the Treatment of Patients With Parkinson Disease With and Without Glucocerebrosidase Gene Mutations: A Nonrandomized, Noncontrolled Trial. JAMA Neurol 2020 Jan 13. doi: 10.1001/jamaneurol.2019.4611. [Epub ahead of print]
- www.neurologen-und-psychiater-im-netz.org/neurologie/erkrankungen/parkinson-syndrom/therapie (last accessed on 05.08.2020)
InFo NEUROLOGY & PSYCHIATRY 2020; 18(5): 25.