At Medidays in Zurich, Prof. Dr. med. Christoph Berger from the University Children’s Hospital showed the innovations that have taken place in the Swiss vaccination schedule in recent years. In particular, he addressed the vaccination protection of young infants (and thus also of pregnant women and their relatives). He also discussed the recommendations for at-risk groups.
(ag) The incidence of invasive diseases caused by Haemophilus influenzae type b (e.g. meningitis or epiglottitis) has decreased sharply in Switzerland since the introduction of vaccination: Between 1988 and 1990, it was approximately 200 cases/per year, whereas between 1997 and 2003, it was 5-13. A similar incidence peak in early childhood (less than one year of age) is shown by invasive pneumococcal disease. “So if you’re going to do these vaccinations, you should do them early in any case,” said Prof. Christoph Berger, MD, of the University Children’s Hospital in Zurich. Conjugate vaccines against invasive bacterial infections are indicated in early infancy and early childhood according to the 2014 vaccination schedule (Table 1).
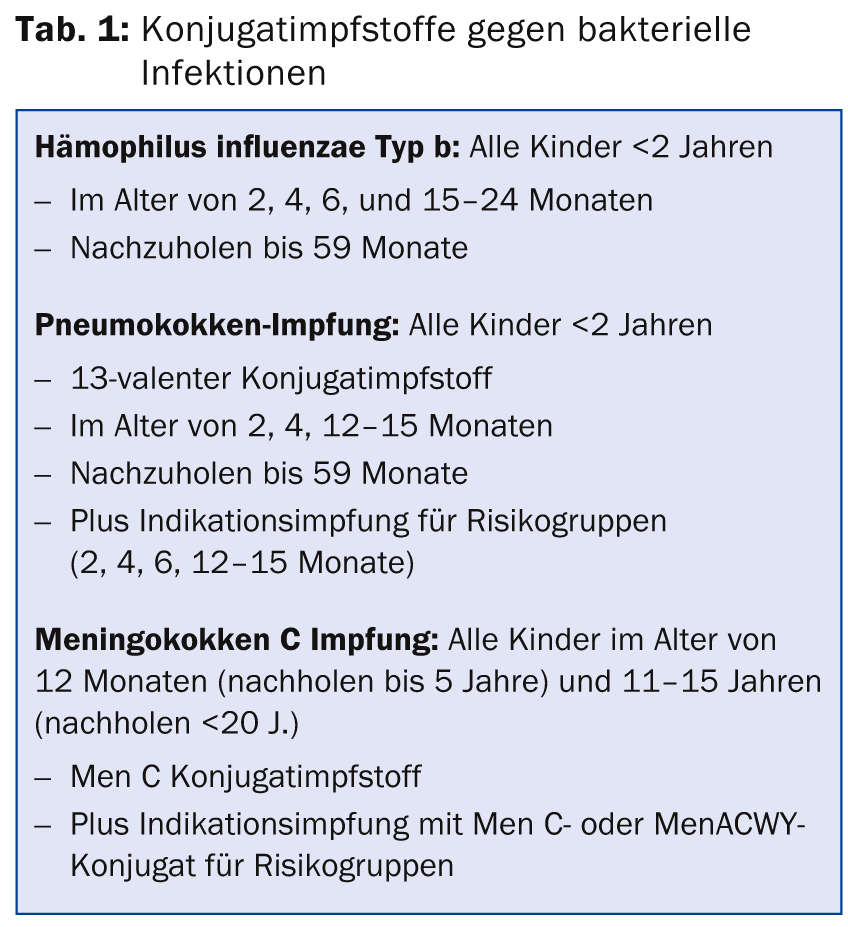
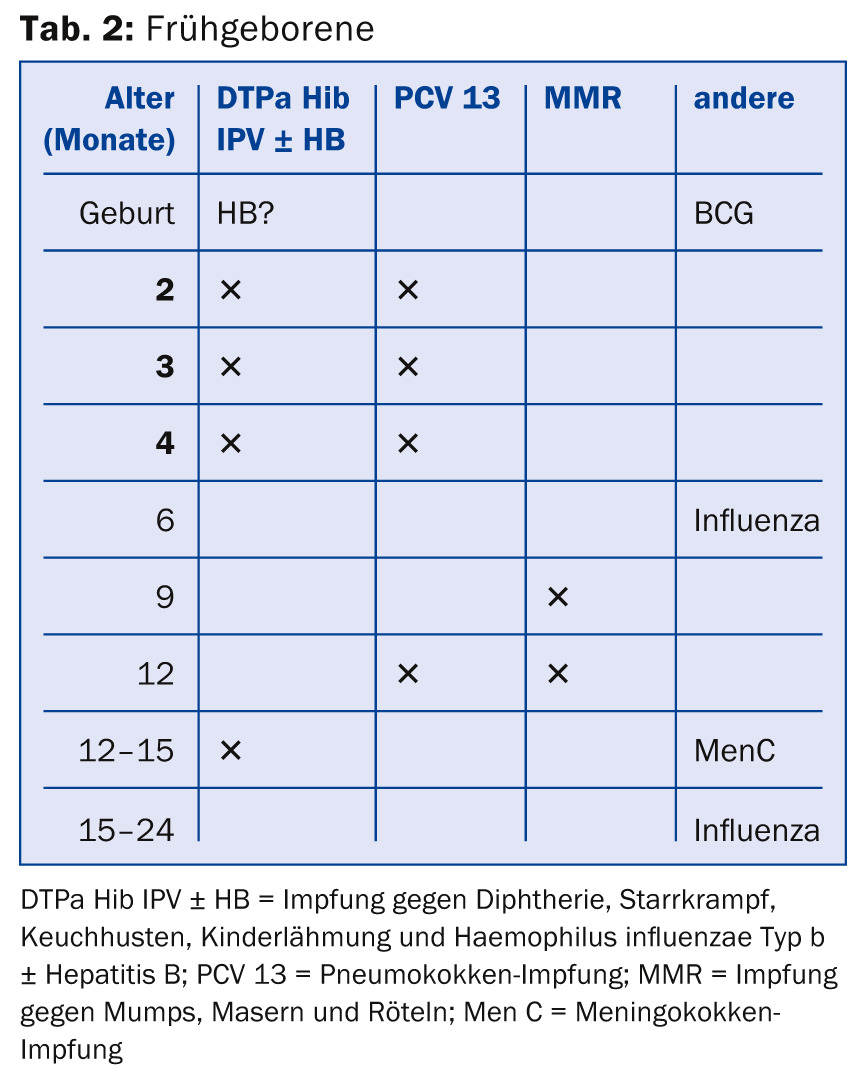
In particular, preterm infants (<32 weeks of gestation, <1500 g) require timely vaccination because they have a higher risk of disease, fewer maternal antibodies, a less good immune response, and only short-lasting antibody titers (Table 2). Immunity of close contacts against pertussis, influenza and varicella is also useful, as parents and siblings bring the diseases home.
Pertussis in infants
“The incidence rate of pertussis is particularly high in newborns: the peak occurs before two months of age and thus cannot be prevented by vaccination in the infant (after all, infants under two months of age are too young to be vaccinated). The solution? You have to vaccinate the sources of infection,” the expert explained. “This is so important because a particularly high number of pertussis deaths occur in the first year of life – and here especially in the first 20 weeks – . 89% of all hospitalizations for pertussis involve infants. The most likely source of infection is parents and siblings (accounting for about 50%).”
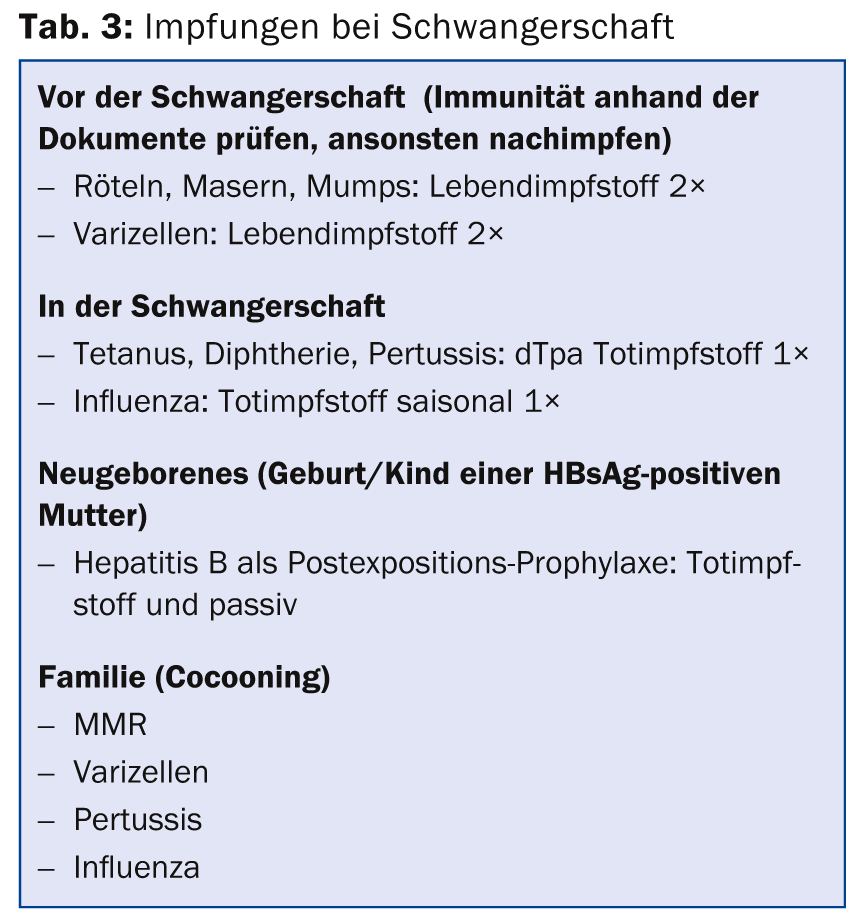
The goal of pertussis vaccination in the 2014 vaccination schedule is thus: Protect infants most at risk – on the one hand, by vaccinating children with the combination vaccine DTPa at 2, 4, 6, 15-24 months of age (in daycare centers at 2, 3, 4, and 12-15 months of age, so that the child is already protected at four months in the daycare center and does not infect anyone) plus a booster at 4-7 and 11-14 years of age. On the other hand, and this is new, just also by vaccinating young adults (generally all 25- to 29-year-olds and all contacts of infants under six months of age, i.e. specifically pregnant women, parents, caregivers) with one-time dTpa vaccination. According to the speaker, this poses no danger during pregnancy. What other vaccinations should be given during pregnancy?
Influenza in pregnancy
Influenza vaccination (inactivated vaccine) is recommended for every pregnant woman, safe as well as effective and easily feasible. “Influenza is more likely to be severe during pregnancy for the pregnant woman and make more complications. In addition, there is an increased risk of prematurity and influenza infection in the young infant. Seasonal influenza vaccination should thus be recommended to every pregnant woman,” Prof. Berger elaborated. In infants, vaccination is not approved until six months of age.
Table 3 summarizes again the recommended vaccinations in pregnancy.
Chronic hepatitis B
If hepatitis is transmitted from mother to child, the risk of chronic hepatitis is much higher, leading in the worst case to carcinoma and death. Therefore, screening for HBs antigen is necessary in every pregnancy (if not done: emergency at birth). If the newborn and mother have antigens, passive and active HB vaccination follow (within twelve hours post partum) (together >90% protection). Thereafter, revaccination is given after one, six, and seven to twelve months (plus complete serology). Breastfeeding does not have to be abandoned; in addition, all family members should be clarified and, if necessary, vaccinated.
Measles
“We need to vaccinate against measles on time and everywhere. Also, every chance to get a catch-up vaccination should be taken so that there is less measles circulating overall,” the speaker said. The MMR vaccine is a live vaccine against measles, mumps and rubella. After one vaccination (at age ≥1 year), 90% of vaccinated individuals develop antibodies (5% vaccination failure); 99% have vaccine antibodies after two vaccinations. It should be vaccinated with a minimum interval of ≥4 weeks (e.g., 12 and 15-24 months) (children at increased risk of exposure starting at 6-9 months and second dose at 12 months). Repeat vaccination is appropriate for all non-vaccinated individuals younger than 1963.
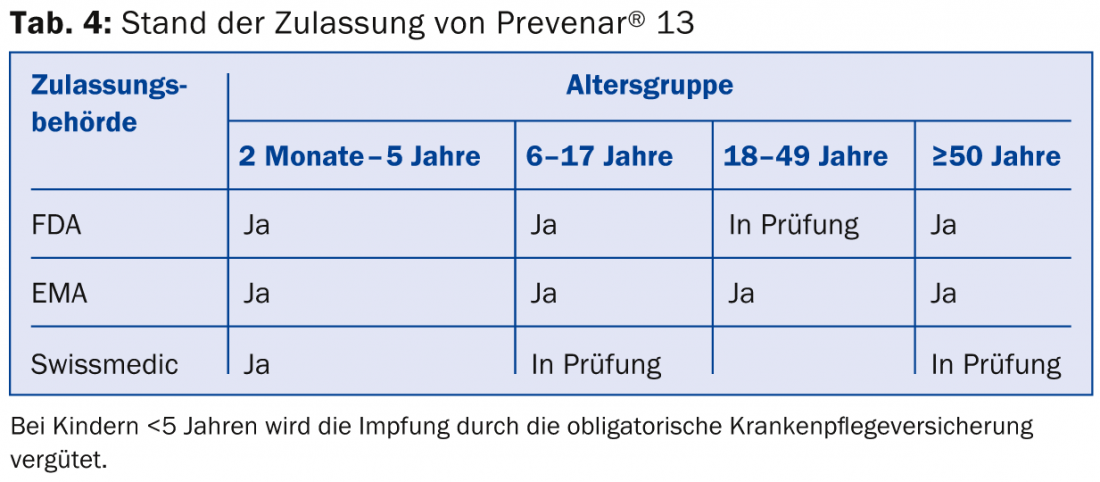
Pneumococcal conjugate vaccine for risk groups
The 2014 vaccination schedule recommends one dose of PCV13 for all persons over two years of age with underlying disease and increased risk for invasive pneumococcal infection. Because the recommendation is off-label for individuals five years of age and older (Table 4), the costs cannot be covered by mandatory health insurance for this age group.
Basic diseases are e.g.: chronic diseases (heart, lung, kidney, liver, spleen, blood), neoplasms, immune disorders. Basic vaccination of all those over 64 is no longer part of the recommendation, since many of them belong to a risk group anyway.
- Vaccination should be administered as soon as possible after diagnosis (i.e. urgently in time).
- Booster vaccinations or additional vaccinations with PPV23 are not (no longer) recommended
- In persons already vaccinated with PPV23, PCV13 should be administered only after an interval of one year
- PCV13 booster vaccination is not recommended (for now).
Transplant Recipient
For transplant recipients before and after solid organ transplantation, give live and dead vaccines whenever possible before transplantation. Vaccination status must be collected early and the respective catch-up vaccination determined. If the rapid vaccination schedule is followed, a complete vaccination status can be achieved before transplantation: To be administered are basic vaccinations (incl. Varicella, hepatitis B, human papilloma viruses in >9-year-olds), risk vaccinations (PCV13, influenza, hepatitis A), and vaccinations depending on individual risks, such as for pre-planned trips (TBE, hepatitis A, yellow fever, rabies).
Source: “Neues im Schweizerischen Impfplan”, presentation at Medidays, September 1-5, 2014, Zurich.
HAUSARZT PRAXIS 2014; 9(12): 42-45











