Alzheimer’s disease (AD) is one of the most commonly diagnosed neurodegenerative diseases worldwide and the leading cause of dementia. Alzheimer’s disease affects 50–70% of dementia patients worldwide and is characterized by cognitive impairment and a progressive decline in functional abilities. As there is no causal therapy that could prevent the onset or halt the progression of Alzheimer’s disease, the medical community faces one of the greatest challenges of the 21st century.
(red) According to the World Health Organization (WHO), the global cost of treating AD is estimated at around USD 1.3 trillion, and this figure will continue to rise in the coming decades. At the same time, the number of people suffering from Alzheimer’s disease will rise to 152 million worldwide by 2050, a fourfold increase on the current prevalence. Low- and middle-income countries are particularly at risk, as they often have limited access to doctors, advanced diagnostics and expensive medication.
Alzheimer’s is a complex, multifactorial disease characterized by pathophysiological processes such as the deposition of beta-amyloid and tau proteins in the brain, neuroinflammatory processes, oxidative stress and mitochondrial dysfunction. These mechanisms lead to a progressive loss of neurons, which in turn leads to cognitive deficits, behavioral changes and the loss of everyday functions. In addition, genetic factors, such as mutations in the PSEN1, PSEN2 and APP genes, play a decisive role in the pathogenesis of familial Alzheimer’s disease. The currently approved pharmacological therapeutic approaches only aim to alleviate symptoms by promoting cholinergic neurotransmission or inhibiting glutamate excitation. However, these drugs, such as donepezil or memantine, have limited efficacy and are associated with a number of side effects such as nausea, dizziness, insomnia and increased fatigue. As a result, phytotherapy is gaining importance as an alternative or complementary treatment.
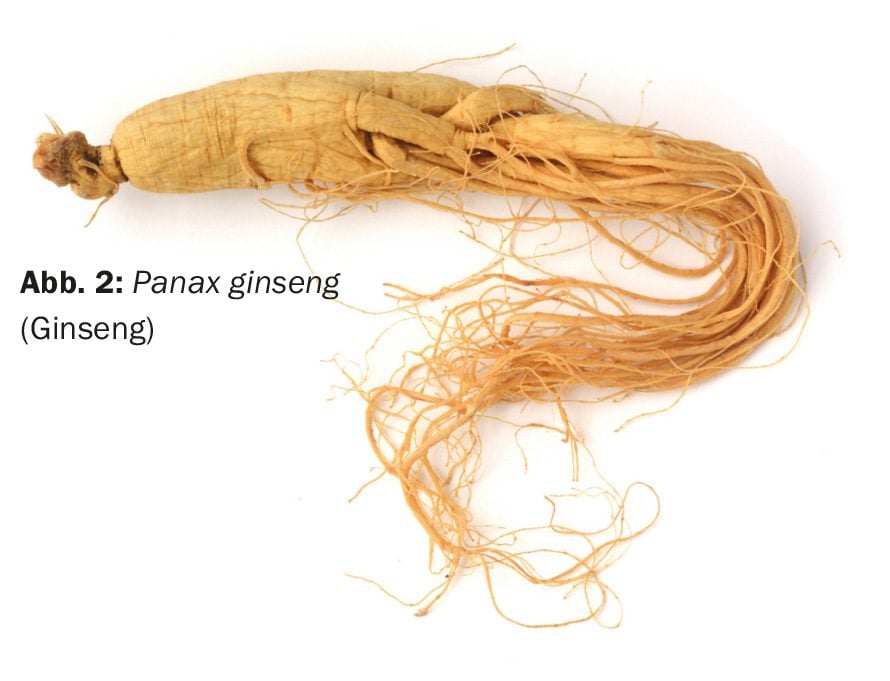
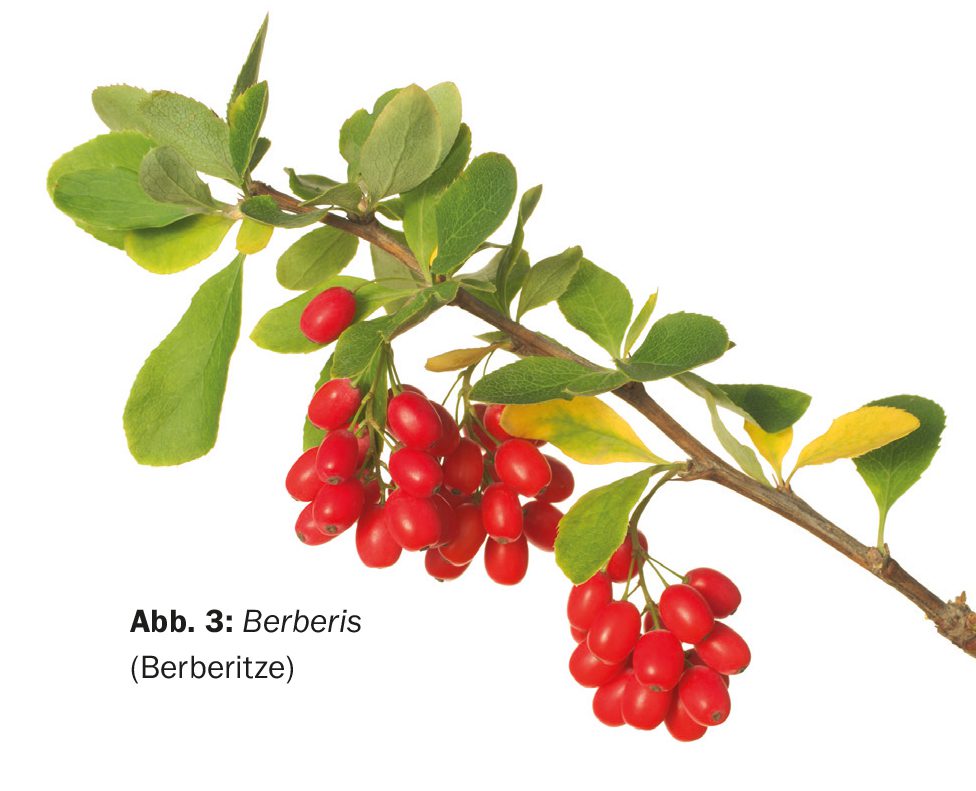
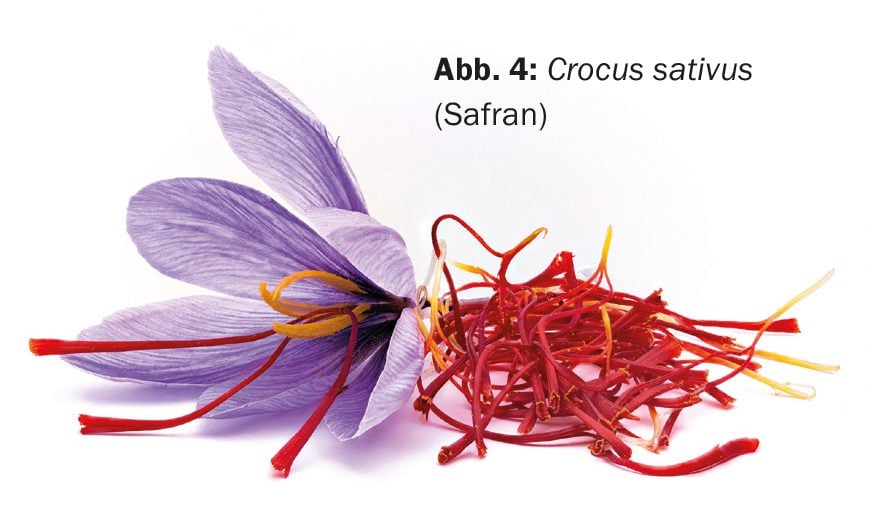
Herbal medicines have proven effective in traditional medicine for centuries, especially in the treatment of neurodegenerative diseases. Herbal compounds such as Curcuma longa (turmeric), Panax ginseng (ginseng), Berberis and Crocus sativus (saffron) have shown promise in Alzheimer’s therapy as they have neuroprotective, anti-inflammatory, antioxidant and anti-apoptotic properties. This article provides a comprehensive overview of the current state of research on these phytochemicals and their potential application in the treatment of Alzheimer’s disease.
Pathophysiological mechanisms of Alzheimer’s disease
Alzheimer’s disease is a progressive neurodegenerative disease that is associated with a variety of pathophysiological mechanisms. One of the best-known hypotheses for the development of Alzheimer’s disease is the beta-amyloid hypothesis. Beta-amyloid (Aβ) is a protein that accumulates in the brain cells of Alzheimer’s patients and forms plaques there. These deposits lead to dysfunction of the neurons and play a central role in the progression of the disease.
Aβ is formed by the cleavage of the amyloid precursor protein (APP) by the enzymes β- and γ-secretase. These pathological processes lead to the formation of neurotoxic Aβ42, which is deposited in the brain in the form of plaques. These plaques not only contribute directly to the damage of neurons, but also activate inflammatory reactions in the brain. In addition to beta-amyloid, the tau protein also plays a decisive role in the pathogenesis of Alzheimer’s disease. Tau proteins normally stabilize microtubules, which ensure axonal transport within the nerve cells. In Alzheimer’s patients, however, hyperphosphorylation of the tau protein occurs, leading to its aggregation and the formation of neurofibrillary tangles. These tangles contribute to synapse dysfunction, neuronal degeneration and memory loss.
Oxidative stress and mitochondrial dysfunction are further central elements in the pathogenesis of Alzheimer’s disease. The overproduction of reactive oxygen species (ROS) leads to damage to the mitochondria, which are responsible for supplying the cells with energy. This process contributes to neuronal dysfunction and promotes cell death. As mitochondrial DNA (mtDNA) is particularly susceptible to damage due to a lack of protective mechanisms, this process is accelerated in older people.
Genetic predispositions also play a significant role. Around 60-80% of the risk of developing Alzheimer’s disease is determined by genetic factors. The apolipoprotein E (APOE) ε4 allele in particular is associated with an increased risk of Alzheimer’s, as it promotes the accumulation of beta-amyloid in the brain. Individuals carrying one copy of the APOE4 gene have up to a sevenfold increased risk of developing Alzheimer’s disease. This complex pathogenesis offers numerous targets for potential therapeutic approaches, including phytotherapy, which relies on the use of plant extracts and their active ingredients to treat disease.
Phytotherapy for Alzheimer’s disease
Phytotherapy refers to the use of herbal medicines for the prevention and treatment of diseases. In relation to Alzheimer’s disease, several plants have been identified in recent years that have the potential to influence neurodegenerative processes. The best-studied plants include Curcuma longa, Panax ginseng, Berberis and Crocus sativus. These plants contain bioactive substances that exhibit antioxidant, anti-inflammatory, neuroprotective and anti-neurodegenerative effects. Here is a detailed look at their potential effects in Alzheimer’s disease.
Curcuma longa (turmeric, Fig. 1): Curcuma longa, commonly known as turmeric, is a spice and remedy that has been used for centuries in traditional Indian medicine. The main active ingredient, curcumin, is a polyphenol that has numerous pharmacological properties, including antioxidant, anti-inflammatory and neuroprotective effects. Curcumin has the potential to cross the blood-brain barrier, which is of particular interest for its use in Alzheimer’s therapy.
Curcumin works by inhibiting beta-amyloid deposition and hyperphosphorylation of tau proteins, two of the main causes of Alzheimer’s disease. Studies show that curcumin can inhibit the activation of microglia, which are involved in the development of neuroinflammatory processes. In addition, curcumin reduces oxidative stress by reducing the production of ROS and activating antioxidant enzymes.
Despite these promising properties, curcumin has a low bioavailability, which means that it is only available in the body to a limited extent after oral ingestion. To overcome this problem, various nanotechnologies have been developed in recent years to improve the solubility and availability of curcumin in the body. In addition, it has been shown that combining curcumin with other plant compounds, such as Ginkgo biloba, can further increase bioavailability.
Panax ginseng (ginseng, Fig. 2): Ginseng is a medicinal plant that has been used in traditional Chinese and Korean medicine for more than 2000 years. The root contains ginsenosides, a group of saponins that have a wide range of pharmacological effects, including antioxidant, anti-inflammatory and neuroprotective effects. In relation to Alzheimer’s disease, studies have shown that ginsenosides inhibit the production of beta-amyloid and improve mitochondrial function.
A particularly promising active ingredient in ginseng is Rg1, a ginsenoside that promotes mitophagy, the process by which damaged mitochondria are broken down. This improves energy production in the cells and reduces the accumulation of harmful proteins such as beta-amyloid. Rg1 also improves memory performance by promoting neurogenesis in the hippocampus and increasing neurotrophic factors such as nerve growth factor (NGF) and brain-derived neurotrophic factor (BDNF).
Berberis (barberry, Fig. 3): Berberis is a genus of plants used in traditional medicine to treat a variety of conditions. The main active ingredient in berberis, berberine, has neuroprotective, antioxidant and anti-inflammatory properties that make it a promising candidate for Alzheimer’s therapy. Berberine works by inhibiting the formation of beta-amyloid plaques and neurofibrillary tangles.
Berberine also influences the cholinergic neurotransmitter circuit by inhibiting the activity of acetylcholinesterase, the enzyme responsible for the breakdown of acetylcholine. This increases the availability of acetylcholine in the brain, leading to an improvement in cognitive function. In addition, berberine has anti-inflammatory properties by reducing the production of cytokines such as IL-1β and TNF-α.
Crocus sativus (saffron, Fig. 4): Saffron is one of the most expensive spice plants and has a long history in traditional medicine. The main active ingredients of saffron, crocin and safranal, have shown neuroprotective and anti-inflammatory effects in studies. Crocin inhibits the formation of beta-amyloid and neurofibrillary tangles, while safranal reduces the activity of acetylcholinesterase, which helps to improve cognitive function in Alzheimer’s patients.
Studies show that saffron achieves similar results to the standard drug donepezil in the treatment of mild to moderate Alzheimer’s dementia, but with significantly fewer side effects. This makes saffron a promising candidate for future Alzheimer’s therapy.
Clinical studies and future developments
Numerous preclinical and clinical studies have shown the potential of herbal medicines in Alzheimer’s therapy. In animal models, curcumin, ginseng, berberine and saffron have shown promising neuroprotective and anti-inflammatory effects. Clinical studies in humans have also shown that these plant compounds can improve cognitive function and slow down the progression of the disease, with fewer side effects than conventional drugs.
Despite these promising results, further long-term studies are needed to confirm the safety and efficacy of these phytotherapeutics. As more and more patients are looking for natural and alternative forms of treatment, it is important to deepen research in this area and develop new phytotherapeutic approaches for the treatment of Alzheimer’s disease.
Conclusion
Phytotherapy offers great potential as an alternative or complementary therapy for the treatment of Alzheimer’s disease. Plants such as Curcuma longa, Panax ginseng, Berberis and Crocus sativus contain bioactive substances that have anti-inflammatory, antioxidant and neuroprotective effects. These plant substances could play an important role in Alzheimer’s therapy in the future, especially in view of the limited effectiveness and numerous side effects of currently available drugs.
However, research in this area is still in its infancy and further clinical trials are needed to confirm the long-term efficacy and safety of these herbal medicines. If the promising results of the studies to date are confirmed, phytotherapy could represent an important pillar in the treatment of Alzheimer’s and other neurodegenerative diseases in the future.
Source: Piekarz J, Picheta N, Burdan O, et al: Phytotherapy in Alzheimer’s Disease-A Narrative Review. Biomedicines. 2024 Aug 9; 12(8): 1812. doi: 10.3390/biomedicines12081812. PMID: 39200276; PMCID: PMC11351709.
PHYTOTHERAPIE PRAXIS 2024; 1(1): 22–23