Peripheral arterial tonometry is a modern technique for outpatient sleep medicine diagnostics. Evaluations for sleep architecture analysis can be fully automated and manual. Low patient stress allows multiple measurements to reduce night-to-night variability.
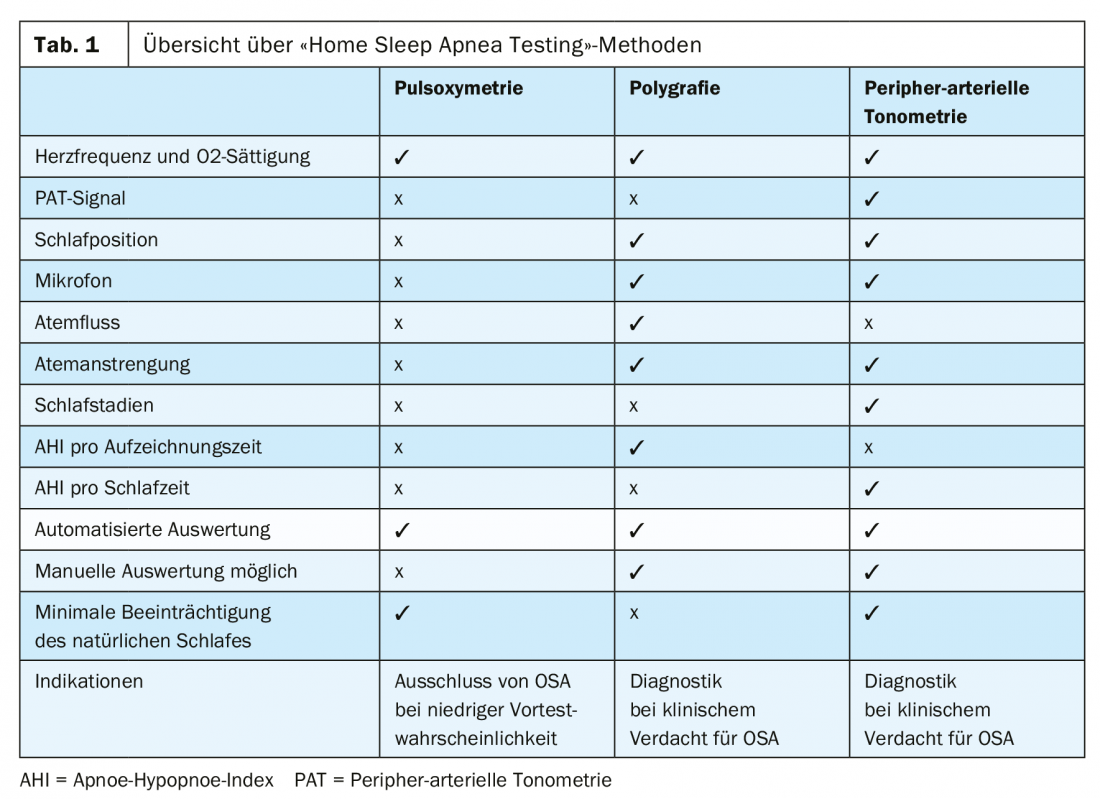
Sleep-related breathing disorders are common. A Swiss study of 2121 participants in Lausanne showed that 49.7% of men and 23.4% of women had an apnea-hypopnea index (AHI) >15/h, corresponding to at least mild obstructive sleep apnea (OSA) [1]. Sleep-disordered breathing is often undiagnosed but has potentially dangerous consequences, such as increased risk of myocardial infarction, stroke, and arterial hypertension [2]. “Home Sleep Apnea Testing” (HSAT) is at the forefront of the diagnosis of obstructive sleep-related breathing disorders. Peripheral arterial tonometry is one of these HSAT procedures (Table 1).
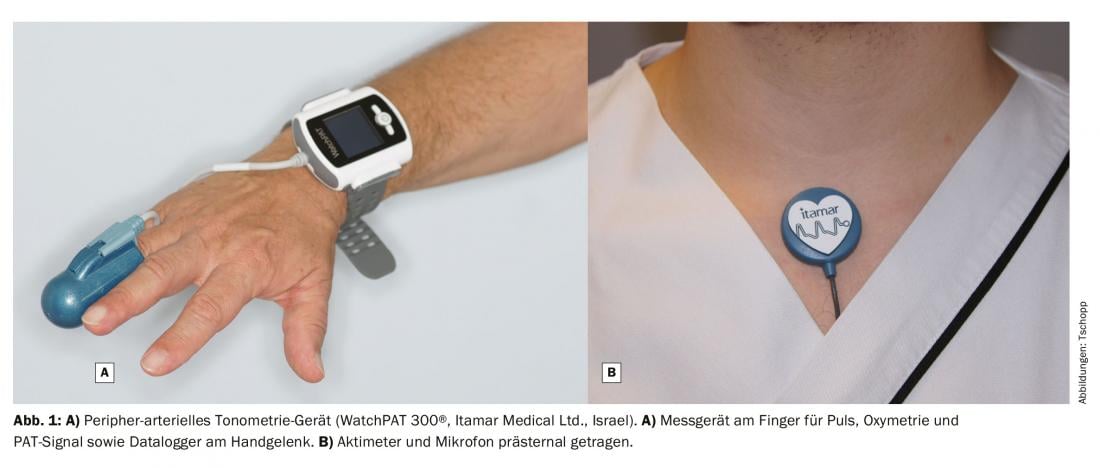
The value of the pulse in medicine was recognized and described centuries ago [3]. Advanced peripheral arterial tonometry (PAT) analyzers were first introduced in 1999 and used to measure peripheral endothelial function as a prognostic parameter for cardiovascular risk [4,5] (Fig. 1). Only later was its value for sleep medicine diagnostics recognized. The first equipment for this was purchased in Switzerland in 2009. Initially, these were used primarily by ENT physicians, but later they were increasingly used by pulmonologists and cardiologists.
Basics of peripheral arterial tonometry
Peripheral arterial tonometry is a precise measurement of the pulsatile volume of the peripheral arteries, which depends on the activity of the sympathetic nervous system in the peripheral vessels. Especially on the acras, such as fingertips and earlobes, there are many vessels innervated by alpha-sympathetic nerve fibers. These are important for thermoregulation, but are also very sensitive to other stimuli such as stress. PAT can detect small changes in the volume of the vessels and thus provide conclusions about the activity of the sympathetic nervous system.
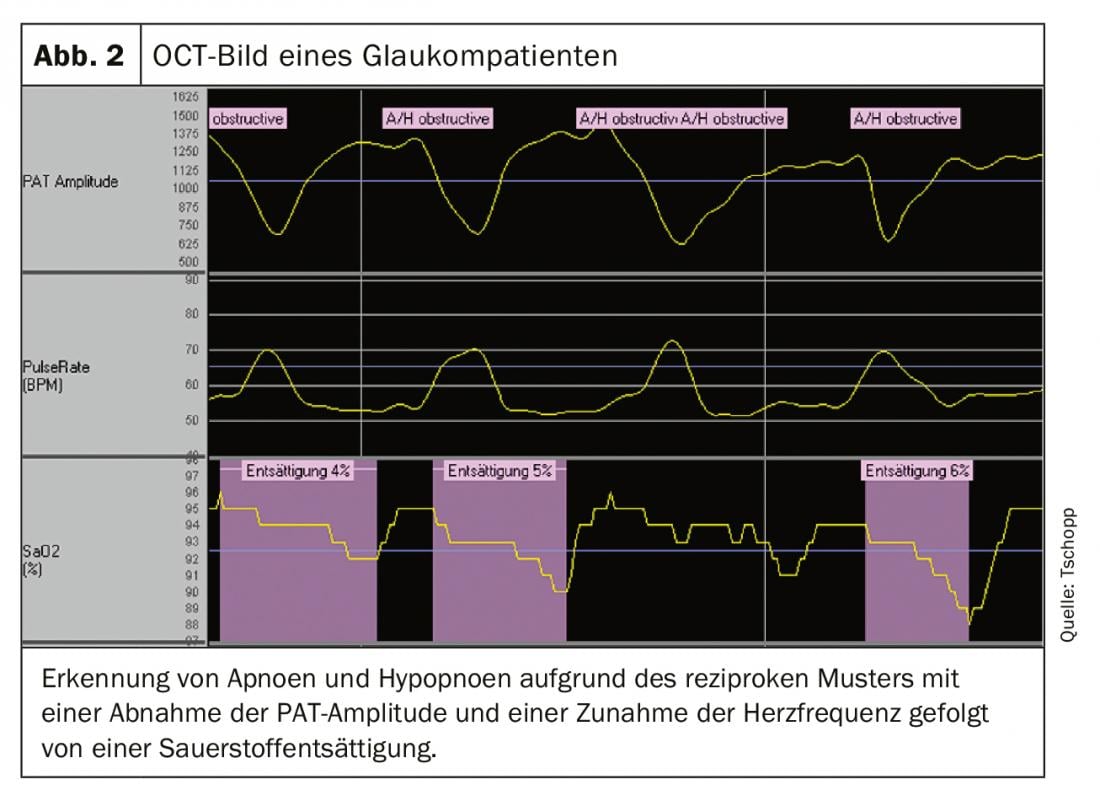
OSA is characterized by upper respiratory tract obstruction leading to repetitive apneas and hypopneas. These, in turn, fragment sleep and are triggers for the typical symptoms of OSA, such as daytime sleepiness, microsleep, depressed mood, and difficulty concentrating [2,6]. Apneas and hypopneas occur in characteristic cycles. These begin during sleep with the relaxation of the muscles that keep the upper airway open while awake. At a certain point, the flow of air is restricted (hypopnea) or even completely interrupted (apnea). This results in O2 desaturation and arise in CO2 in the blood, which triggers activation of the sympathetic nervous system. This leads to an arousal reaction with increased toning of the airway muscles and the apnea or hypopnea ends with a so-called arousal. This process with activation of the sympathetic nervous system is accompanied by vasoconstriction, which can be seen as a reduction in amplitude in the PAT signal and an increase in heart rate. This results in a so-called reciprocal pattern. The drop in peripheral blood oxygen characteristic of hypopneas can also be measured in PAT recordings. Figure 2 shows a sequence of such events with reciprocal pattern of PAT amplitude decrease and pulse increase followed by oxygen desaturation.
When diagnosing OSA with PAT technology, oxygen saturation, heart rate and PAT signal are measured directly. From this, arousals as well as apneas and hypopneas can be inferred. It is therefore a surrogate measurement. PAT technology in sleep medicine derives 7 channels: PAT signal, oximetry, heart rate, actimetry (body position), snoring sound (microphone) and the thorax movement (via the movement of the actimeter).
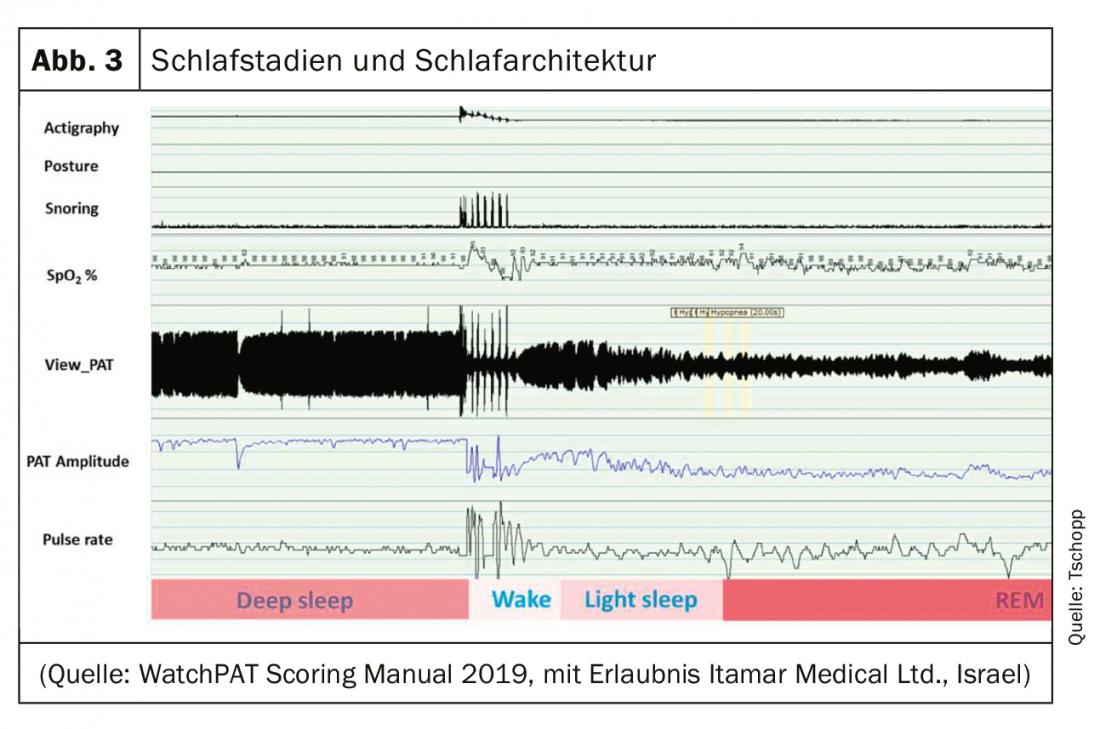
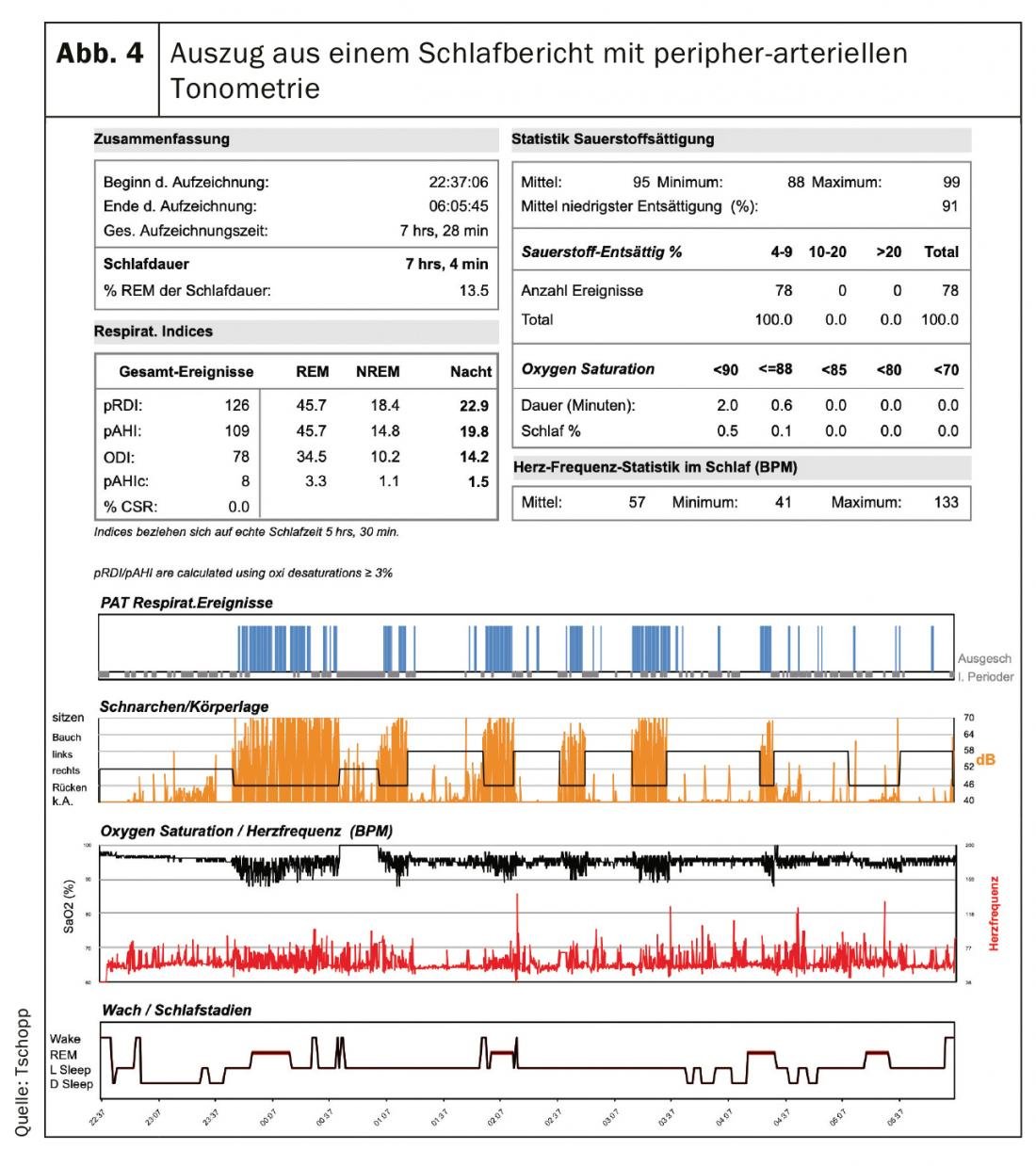
The PAT provides additional information beyond the breathing events. By means of typical PAT characteristics of sleep stages, sleep architecture can be inferred. In REM sleep, heart rate variability is higher than in non-REM sleep, in which heart rate is regulated within tighter limits. Due to a higher activity of the sympathetic nervous system, the PAT amplitude also decreases during REM sleep and shows a high variability [7]. In addition, information from the actimeter (movement) and the microphone (snoring) is used for analysis, so that PAT technology can be used to distinguish between REM sleep, deep sleep, light sleep and wakefulness ( Fig. 3 and 4). This allows an analysis of the sleep architecture with a simplified hypnogram. Apneas and hypopneas can thus be specified per sleep time and not only per measurement time. The PAT can thus become a “home sleep lab light”.
PAT technology is fundamentally different from traditional HSAT methods, such as respiratory polygraphy, which directly measures respiratory motion using abdominal and chest belts.
Evaluation and interpretation
Nocturnal peripheral arterial tonometry can be evaluated fully automatically. This algorithm-based scoring has been validated in several studies by correlation with polysomnography [8,9]. However, this evaluation was criticized insofar as it could not be manually verified so far. In addition, there was evidence that the algorithm has a tendency to “overscore” especially in moderate OSA with AHI 15-30/h [8]. The AASM approved peripheral arterial tonometry as an HSAT method in 2017, but requires that manual scoring of recordings be possible [10]. This has been taken into account in the new software version (zzzPAT®, Itamar Medical Ltd., Israel) has been implemented. It is thus possible to view and interpret the signals and to validate the automatic evaluation by manual scoring. The PAT software is very similar to respiratory polygraph scoring programs. It allows the automatically generated evaluation to be visually inspected and manually scored in a manner analogous to respiratory polygraphy.
Obstructive sleep-disordered breathing manifests in nocturnal PAT as a reciprocal pattern with an increase in heart rate and a decrease in PAT amplitude triggered by the arousal response with increase in sympathetic tone at the end of apnea or hypopnea. Typically, these obstructive breathing episodes result in a sawtooth pattern of decrease and rebound in oxygen saturation (Fig. 2).
The latest PAT technology (Watch PAT central plus and Watch PAT 300, Itamar Medical® Ltd., Israel) enables the distinction between peripheral and central sleep-related breathing disorders. Respiratory motion is measured with the actimeter on the chest.
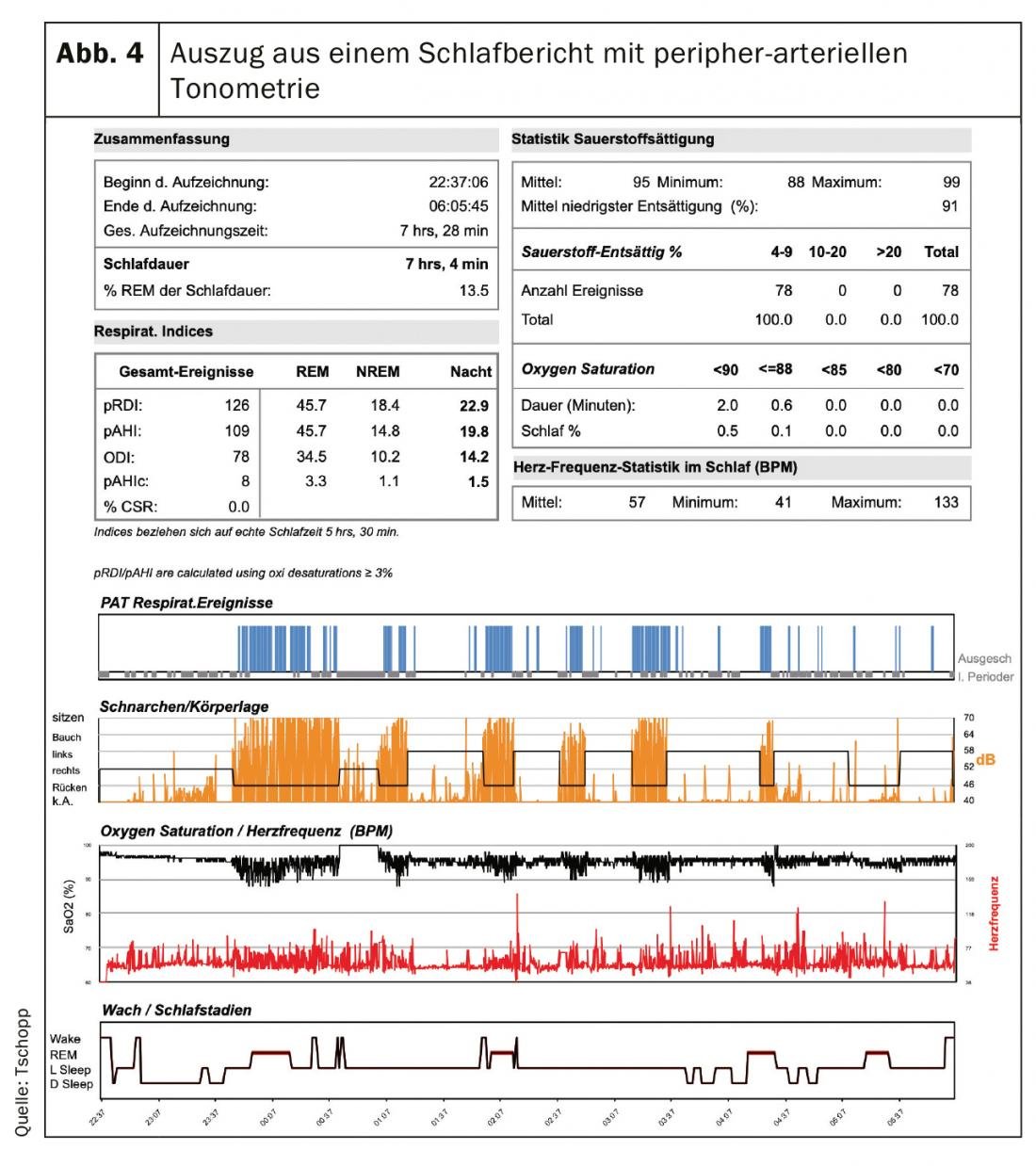
Figure 4 shows an excerpt from a sleep study report as it can be generated fully automated or manually edited with the PAT. In the upper half, the most important statistical key figures of the recorded night are listed. The lower half gives a graphical overview of the night. The top row shows PAT-detected respiratory events, which are associated with heavy snoring in the second row and oxygen desaturations in the third row. In this case, a clear positional dependence can be seen in that the obstructive breathing events occur almost exclusively in the supine position and are accompanied by impressive snoring. At the bottom of the report a simplified hypnogram is given, in which the typical increase of REM sleep in the second half of the night can be seen, which corresponds to the physiological process.
Value of peripheral arterial tonometry in sleep medicine diagnostics.
PAT is very low impact for patients because this method does not require cables in the face or thoracic and abdominal belts. Thus, normal sleep is hardly disturbed by the measurement. In particular, the patient can move freely and does not have the tendency to increasingly assume the supine position due to the measuring device. This is a disadvantage of polysomnography in the sleep laboratory, where “wiring” leads to a significantly higher supine time, a body position in which OSA is often particularly pronounced. Therefore, with polysomnography in the sleep laboratory, the severity of OSA is often overestimated, which is due to this measurement-related increased supine position [11,12].
An HSAT is recommended by the Swiss Society of Otolaryngology as well as that of Pneumology in accordance with the guidelines of the American Sleep Medicine Society when there is a high probability of OSA. Signs of a high likelihood of OSA include loud and irregular snoring, observed pauses in breathing, nocturnal choking episodes, and symptoms typical of OSA, such as increased daytime sleepiness and morning headaches [10]. Table 1 shows an overview of HSAT methods and their advantages and disadvantages. The advantage of respiratory polygraphy is the direct measurement of respiration, but this requires the wearing of chest and abdominal belts and nasal cannulae. Differentiation between apneas and hypopneas is possible. The disadvantage, however, is that the AHI is not related to sleep time but to measurement time. A major advantage of the PAT technology is the low patient discomfort, as the method does not require nasal cannulae or chest and abdominal belts. A simplified hypnogram can be created and the AHI can be given in relation to sleep time. However, it is not possible to differentiate between apneas and hypopneas, which is not essential in clinical practice.
Limitations of the HSAT methods, which also apply to the PAT technology, are that they are not sufficient for the diagnosis of neurological sleep disorders. For neurological sleep disorders, such as “periodic limb movement”, parasomnias or narcolepsy, polysomnography in a sleep laboratory is still required.
Summary
PAT technology is a valuable advancement in outpatient sleep medicine diagnostics. For the first time, sleep architecture can also be assessed in the “home setting” with a simplified hypnogram. The AHI value is no longer given in relation to measurement time, but to sleep time. With the latest version (Watch PAT 300®), central respiratory regulation disorders can also be diagnosed and manual editing and validation of the measurement is possible. PAT technology is thus gaining a high profile in outpatient sleep medicine diagnostics, even among primary care physicians.
Take-Home Messages
- Peripheral arterial tonometry is a modern technique for outpatient sleep medicine diagnostics.
- It allows the analysis of the sleep architecture.
- Indication of the apnea-hypopnea index related to the sleep time and not to the measurement time as in conventional home measurements.
- Hardly burdensome for patients and therefore multiple measurements to reduce night-to-night variability well accepted by patients.
- Fully automated and manual evaluations are possible.
Literature:
- Heinzer R, Vat S, Marques-Vidal P, et al: Prevalence of sleep-disordered breathing in the general population: the HypnoLaus study. Lancet Respir Med. 2015; 3(4): 310-318. doi:10.1016/S2213-2600(15)00043-0.
- Thurnheer R: The obstructive (and central) sleep apnea syndrome. Swiss Med Forum. 2018; 18(23): 482-488. doi: https://doi.org/10.4414/smf.2017.03305
- O’Rourke MF, Mahomed FA: Hypertension. 1992; 19(2): 212-217. doi:10.1161/01.HYP.19.2.212
- Schnall RP, Shlitner A, Sheffy J, et al: Periodic, profound peripheral vasoconstriction – a new marker of obstructive sleep apnea. Sleep. 1999; 22(7): 939-946.
- Süssenbacher A, Frick M, Alber HF: Peripheral endothelial function measurement – use justified in daily clinical practice? J Cardiol. 2012; 19(9-10): 283-288.
- Stuck BA, Maurer JT, Schredl M, Weeß H-G: Practice of sleep medicine. Berlin, Heidelberg: Springer Berlin Heidelberg; 2013. doi:10.1007/978-3-642-34881-5
- Lavie P, Schnall RP, Sheffy J, Shlitner A: Peripheral vasoconstriction during REM sleep detected by a new plethysmographic method. Nat Med 2000; 6(6): 606-606. doi:10.1038/76135
- Penzel T, Kesper K, Ploch T, et al: Ambulatory Recording of Sleep Apnea Using Peripheral Arterial Tonometry. In: The 26th Annual International Conference of the IEEE Engineering in Medicine and Biology Society. Vol 4. San Francisco, CA, USA: IEEE 2004: 3856-3859. doi:10.1109/IEMBS.2004.1404079.
- Yalamanchali S, Farajian V, Hamilton C, et al: Diagnosis of obstructive sleep apnea by peripheral arterial tonometry: meta-analysis. JAMA Otolaryngol Neck Surg. 2013; 139(12): 1343. doi:10.1001/jamaoto.2013.5338.
- Kapur VK, Auckley DH, Chowdhuri S, et al: Clinical Practice Guideline for Diagnostic Testing for Adult Obstructive Sleep Apnea: An American Academy of Sleep Medicine Clinical Practice Guideline. J Clin Sleep Med. 2017; 13(03): 479-504. doi:10.5664/jcsm.6506.
- Ravesloot MJL, de Raaff CAL, van de Beek MJ, et al: Perioperative Care of Patients With Obstructive Sleep Apnea Undergoing Upper Airway Surgery: A Review and Consensus Recommendations. JAMA Otolaryngol Neck Surg. 2019; 145(8): 751. doi:10.1001/jamaoto.2019.1448.
- Vonk PE, Rotteveel PJ, Ravesloot MJL, et al: The influence of position-dependency on surgical success in sleep apnea surgery – a systematic review. Sleep Breath. October 2019. doi:10.1007/s11325-019-01935-y
HAUSARZT PRAXIS 2019; 14(11): 11-14