Surgical treatment of localized prostate cancer is standard in patients with a life expectancy of more than ten years. Surgery is aimed not only at tumor control, but also at preserving continence and erectile function. Laparoscopic robotic-assisted prostatic vesiculectomy (Da-Vinci®) allows the surgeon to accurately and precisely dissect the tissue, resulting in excellent outcomes in terms of tumor-free survival, continence, and preservation of erectile function.
Prostate cancer is the most frequently diagnosed tumor disease in men worldwide. In Switzerland, the diagnosis is made in about 6000 men per year. The peak age is beyond 50 years of age, and more than half of the men with the disease are older than 70 years [1].
Surgical treatment of localized prostate cancer remains the therapeutic standard in patients with a life expectancy of more than ten years. There are basically three goals with surgery: Tumor control, preservation of continence, and the possible preservation of erectile function [2]. Radical prostatic vesiculectomy is currently the only treatment option that shows an advantage over conservative therapy in terms of overall survival as well as tumor-specific survival [3]. To achieve these set goals, careful patient and tumor selection is essential.
Estimation of life expectancy as the basis for a therapy decision
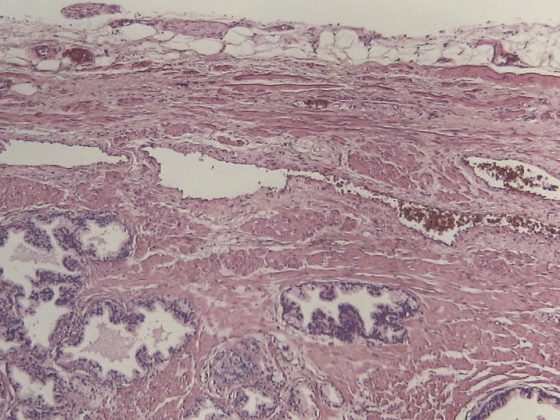
Initial decision-making aids other than the PSA value are the digital-rectal examination and transrectal ultrasound. In addition, a suspected tumor must be confirmed in every case with a systematic prostate punch biopsy. This provides information about the tumor volume and the aggressiveness of the tumor by means of the Gleason score.
With the help of these data, the urologist can already estimate the postoperative healing rate preoperatively using nomograms. The physician has various aids at his disposal in the form of the so-called Partin charts and the Kattan nomogram [4]. In addition, the patient’s age, comorbidities, and the resulting estimated life expectancy play a crucial role in the decision regarding the choice of therapy.
Since clinically localized prostate cancer is usually slow growing, life expectancy should be at least ten years. With the help of a comorbidity score, the life expectancy of a 75-year-old man can be estimated: Without comorbidities this is 11.9 years, with a comorbidity score of 2 still 6.3 years and with a score of 3 statistically only 1.9 years [5].
High survival rates after radical prostatectomy
Tumor-free survival can be expected in a high proportion of patients after radical prostatectomy, assuming appropriate patient and tumor selection. A tumor-specific survival rate of 82% at 15-35 years was reported by Gibbons et al. described [6]. Schiavina et al. showed a biochemical recurrence-free rate of 80% five years and of 55.8% ten years after radical prostatectomy [7]. Porter et al. report a cancer-specific, postoperative survival rate of 96% at ten years, 91% at 15 years, and as high as 82% at 25 years [8].
The PSA level should remain below the detection limit after radical prostatectomy in patients with localized prostate cancer. Most patients experience recurrence within the first five years after surgery [9]. Important prognostic factors for postoperative outcome include local tumor stage, Gleason score, carcinoma volume, and surgical settling margin (positive or negative settling margin).
Preservation of continence
Preservation of continence is another critical goal in surgical therapy of localized prostate cancer. Publications show a significant range of continence rates. Reasons for these differences include the method of data collection (face-to-face interview or standardized questionnaires), the different definition of incontinence, and the timing of the interview after surgery. Likewise, the surgical technique plays a decisive role.
Schiavina et al. distinguish between complete continence in 78.5% of patients and use of safety templates in 13.8% of patients after radical prostatectomy [7]. Michl et al. report an incontinence rate of 9.8% after nerve-preserving radical prostatectomy compared with an incontinence rate of 22.4% without preservation of the vascular-nerve bundle [10]. Thus, even in patients with preoperative erectile dysfunction, bilateral preservation of the vascular-nerve bundle is reasonable if oncologically and surgically feasible.
Preservation of erectile function
An important factor for patients with localized prostate cancer that influences decision making regarding therapy is preservation of erectile function. When Hugh Hampton Young first reported perineal radical prostatovesiculectomy more than 100 years ago, he was certainly far from preserving the patient’s potency. Even when Millin first performed a radical prostatectomy retropubically in 1947, potency preservation was not the main goal of the operation [12].
In recent years, a better understanding of anatomy and ever-improving surgical treatment techniques have led to the radicality of prostatic vesiculectomy being associated with a reduction in perioperative morbidity on the one hand, and improved postoperative outcome and quality of life on the other.
Data collection is one of the biggest problems in erectile function. Many published papers have assessed postoperative erectile function using patient interviews. It makes sense to assess erectile function using the International Index of Erectile Function questionnaire prior to nerve-vessel bundle preservation. A study already published in 2002 by Noldus et al. reported preservation of erectile function (one year after surgery) in 90% of patients after bilateral nerve sparing and in 56% of patients after unilateral nerve preservation [11]. With the aid of PDE-5 inhibitors, most patients with primarily nonsexual erections were able to achieve one.
Laparoscopic robot-assisted prostatic vesiculectomy (Da-Vinci®) is a consistent further development of laparoscopy. This technique allows the surgeon to accurately and precisely dissect the tissue, resulting in excellent outcomes. Thus, Ficarra et al. show biochemical recurrence-free survival at three, five, and seven years of 96.3, 89.6, and 88.3%, respectively. 80% of patients were continent postoperatively, 11% required one safety presentation per day, and only 9% of patients operated on were incontinent. Forty-seven percent of patients after robot-assisted radical prostatic vesiculectomy had sexually active erections without further aids, and in another 37% this could be achieved with PDE-5 inhibitors [13].
Conclusion
Radical prostatic vesiculectomy is the surgical gold standard in the treatment of localized prostate cancer. The goal is optimal tumor control, combined with preservation of potency and continence and thus a good quality of life.
Historically, radical prostatic vesiculectomy has been associated with a high rate of intraoperative and postoperative complications, such as high blood loss, increased incontinence rates, and erectile dysfunction. Although direct comparison of the different surgical methods is difficult, recent studies show excellent survival, continence, and potency rates achievable with robotic-assisted surgery. Thus, a high quality of life of patients after surgery can be achieved.
Literature:
- Krebsliga Schweiz, Zahlen zu Krebs 2012: https://assets.krebsliga.ch/downloads/krebszahlen_2012_d.pdf.
- Bianco FJ Jr, Scardino PT, Eastham JA: Radical prostatectomy: long-term cancer control and recovery of sexual and urinary function (“trifecta”). Urology 2005; 66(5 Suppl): 83-94.
- Bill-Axelson A, et al: Radical prostatectomy versus watchful waiting in early prostate cancer. N Engl J Med 2011; 364(18): 1708-1717.
- Ross PL, ScardinoPT, Kattan MW: A catalog of prostate cancer nomograms. J Urol 2001; 165: 1562-1568.
- Albertsen PC, et al: The impact of co-morbidity on life expectancy among men with localized prostate cancer. J Urol 1996; 156: 127-132.
- Gibbons RP, et al: Total prostatectomy for clinical localized prostatic cancer: long-term results. J Urol 1989; 141: 564-566.
- Schiavina R, et al: Survival, Continence and Potency (SCP) recovery after radical retropubic prostatectomy: A long-term combined evaluation of surgical outcomes. EJSO 2014 Jul 18.
- Porter CR, et al: 25-year prostate cancer control and survival outcomes: A 40-year radical prostatectomy single institution series. J Urol 2006; 176(2): 569-574.
- Partin AW, et al: Serum PSA following anatomical radical prostatectomy: The Johns Hopkins experience after 10 years. Urol Clin North Am 1993; 20: 713-725.
- Michl U, et al: Prospective analysis of continence and micturition following nerve sparing and non nerve sparing radical retropubic prostatectomy. Significant impact of the nerve sparing procedure on continence. J Urol 2001; 165 (Suppl).
- Noldus J, et al: Patient-reported sexual function after nerve-sparing retropubic radicalprostatectomy. Eur Urol 2002; 42: 118-124.
- Millin T: Retropubic Urinary Surgery. London, Livingstone, 1947.
- Ficarra V, et al: Long-term evaluation of survival, continence and potency (SCP) outcomes after robot-assisted radical prostatectomy (RARP). BJU Int 2013; 112(3): 338-345.
InFo ONCOLOGY & HEMATOLOGY 2014; 8(2): 6-8.