Psoriatic arthritis (PsoA) is a common comorbidity of psoriasis. Despite the high prevalence, arthritic symptoms often remain undiagnosed. In addition to the CASPAR classification (“Classification Criteria for Psoriatic Arthritis”), there are certain genetic factors which are associated with joint involvement. The human leukocyte antigen (HLA) system plays an important role, with HLA-B-27, B-39, and B-07 in particular associated with PsoA.
It is now known that psoriasis is a heterogeneous disease with different variants [1]. According to the literature, the proportion of psoriasis patients who develop psoriatic arthritis (PsoA) during the course of the disease is up to 30%, depending on the source [2]. It is believed that over 10% of patients with psoriasis suffer from undiagnosed PsoA [3]. Detecting a preclinical phase of psoriatic arthritis remains a challenge. Among others, certain clinical manifestations of different psoriasis phenotypes are associated with an increased risk of developing PsoA. Careful assessment of the affected areas of the body may be helpful to identify any subclinical PsoA and then initiate further investigations. In particular, scalp and nail infestation is correlated with the development of PsoA [4]. That there are certain genetic biomarkers associated with an increased risk of developing psoriatic arthritis has been known for some time, and numerous recent findings confirm this.
Major histocompatibility complexes (MHCs) targeted
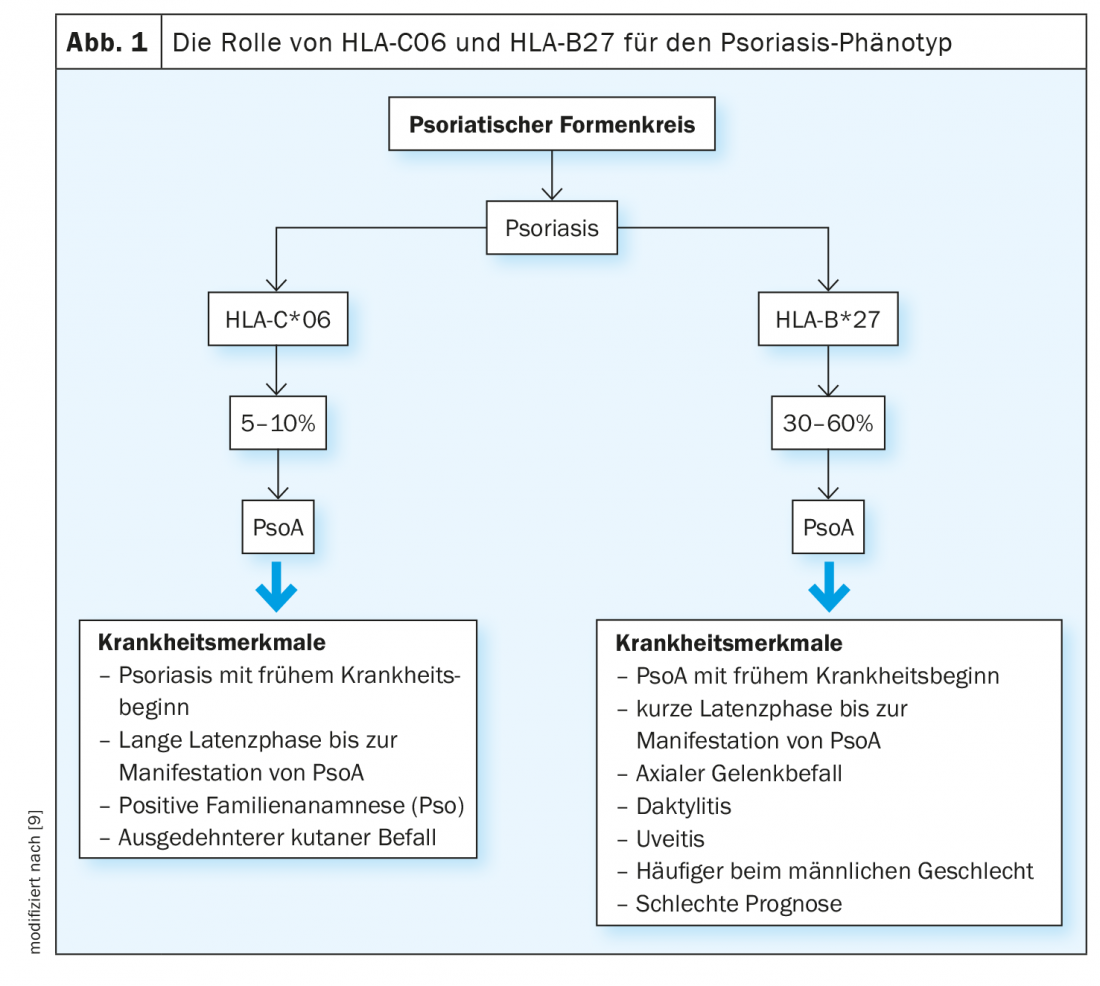
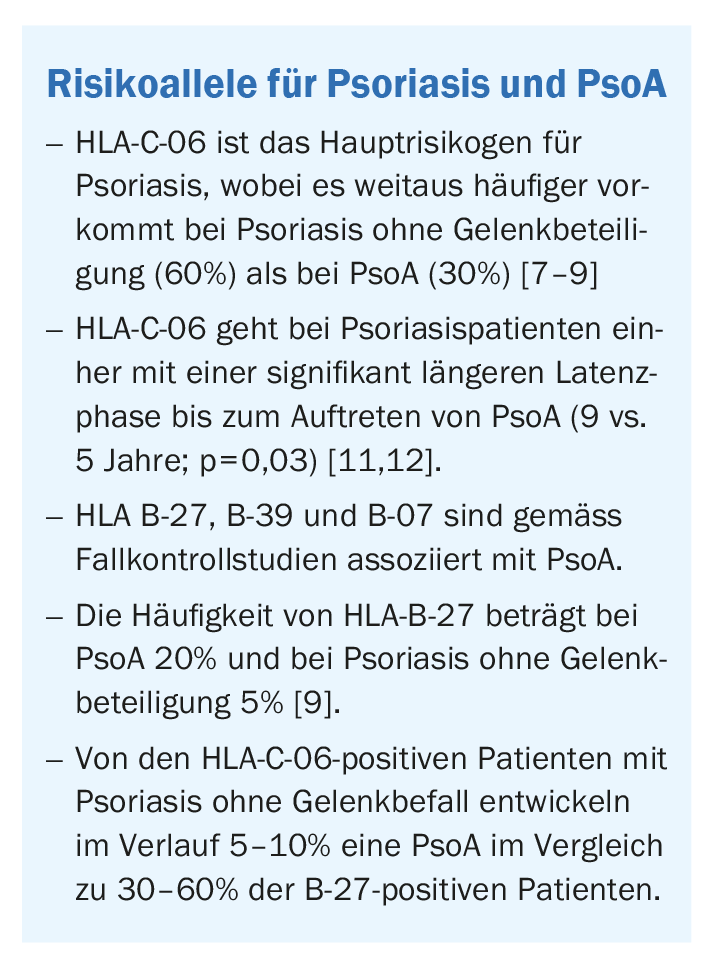
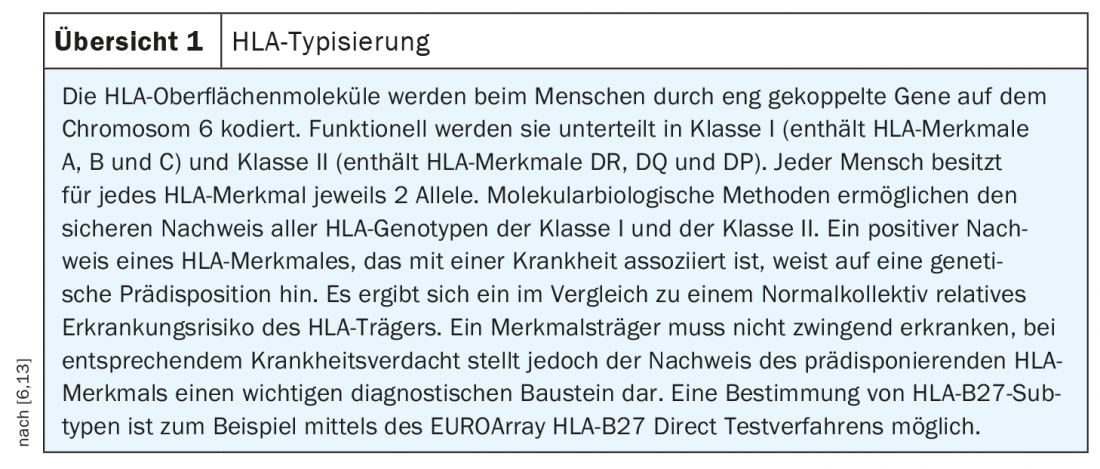
As is known from prospective studies, it usually takes several years before psoriatic arthritis develops [5]. The CASPAR classification (“Classification Criteria for Psoriatic Arthritis”) is used to diagnose PsoA. This diagnostic tool captures sacroilitis, enthesitis, dactylitis, and nail infestation as clinical subphenotypes. As genetic analyses showed [5], these clinical features correlate with the individual HLA (human leukocyte antigen) type. The HLA system is controlled by genes on chromosome 6 and encodes cell surface molecules that present endogenous and exogenous antigen peptides to the cellular immune system. HLA traits are an important biomarker for psoriasis and other autoimmune diseases. Based on the complex of HLA molecule and antigen, lymphocytes react with an immune response or tolerate the presented antigen as endogenous [6]. The major risk gene for psoriasis is the HLA class I allele HLA-C*06:02 (Fig. 1) [7]. To determine whether the frequency of the HLA-C*06:02 allele differs between patients with psoriasis without joint involvement and those with PsoA, DNA-based allele typing was performed [5,8]. The psoriasis cohort (n=214) had no features of arthritis, spondylitis, or enthesitis, whereas the psoriatic arthritis cohort (n=359) presented to a rheumatology department in association with joint symptoms. In the psoriasis cohort, 57.5% had an HLA-C*06:02 allele compared with 19.3% in a control population (OR 6.61, p<0.0001), consistent with previous findings. In the psoriatic arthritis cohort, the frequency of HLA-C*06:02 was only 27.9%, which is significantly lower than in the psoriasis cohort (OR 0.30, p <0.0001), but significantly higher compared to the control population (OR 1.9, p<0.0001). The question of which HLA alleles are present in PsoA patients who do not have C*06:02 was the subject of further investigation. The evaluations showed that HLA-B*27:05:02, HLA-B*39:01:01, and B*38:01:01 are susceptibility alleles for PsoA, as shown by previous findings, but are not high risk alleles for psoriasis without joint involvement. Since HLA-B-27 (Fig. 1) correlates with an early phase of PsoA, it may play an important role in early detection [9]. The membrane-bound HLA-B-27 protein is associated with other autoimmune diseases, such as ankylosing spondylitis or reactive arthritis. Further studies are needed to make more concrete statements on implications of HLA-B-27 for the early detection of PsoA. As it turned out, there are certain differences even within PsoA subphenotypes. For example, HLA-B-27 was shown to be particularly highly correlated with axial PsoA [10]. An overview of the HLA system characterized by high polymorphism is included in the allele database IPD-IMGT/HLA as part of the International ImMunoGeneTics project [14, 15]. HLA typing involves the determination of different classes of major histocompatibility complex (MHC) localized to chromosome 6 gene loci (Overview 1) .
Literature:
- Savage L, et al: Defining Pre-Clinical Psoriatic Arthritis in an Integrated Dermato-Rheumatology Environment. J Clin Med 2020; 9(10): 3262.
- Chicken CK, et al: Skin inflammation with arthritis, synovitis, and enthesitis. JDDG 2019; 17(1): 43-66.
- Villani AP, et al: Prevalence of undiagnosed psoriatic arthritis among psoriasis patients: Systematic review and meta-analysis. JAAD 2015; 73: 242-248.
- Wilson FC, et al: Incidence and clinical predictors of psoriatic arthritis in patients with psoriasis: A population-based study. Arthritis Rheum 2009; 61, 233-239.
- Winchester R: A simple guide to the interpretation of the significance of the association of a disease with a particular HLA allele. Swiss Med Wkly 2019; 149: w20128.
- IMD Laboratory Berlin, www.imd-berlin.de
- Casciano F, et al: T Cell Hierarchy in the Pathogenesis of Psoriasis and Associated Cardiovascular Comorbidities. Front Immunol 2018; 9: 1390.
- Winchester R, et al: HLA associations reveal genetic heterogeneity in psoriatic arthritis and in the psoriasis phenotype. Arthritis Rheum 2012; 64(4): 1134-1144.
- Queiro R, et al: HLA-B27 and psoriatic disease: a modern view of an old relationship. Rheumatology 2016; 55(2): 221-229.
- Chandran V: Genetic determinants of psoriatic arthritis. PhD thesis, Institute of Medical Sciences, University of Toronto, Toronto, ON, Canada, 2013.
- Eder L, et al: Human leucocyte antigen risk alleles for psoriatic arthritis among patients with psoriasis. Ann Rheum Dis 2012; 71: 50-55.
- Queiro R, et al: HLA-C locus alleles may modulate the clinical expression of psoriatic arthritis. Arthritis Res Ther 2006; 8: R185.
- EUROIMMUN Switzerland AG, www.euroimmun.ch
- IPD-IMGT/HLA, www.ebi.ac.uk/ipd/imgt/hla
- The international ImMunoGeneTics Information System, www.imgt.org
DERMATOLOGY PRACTICE 2020; 30(6): 34-36