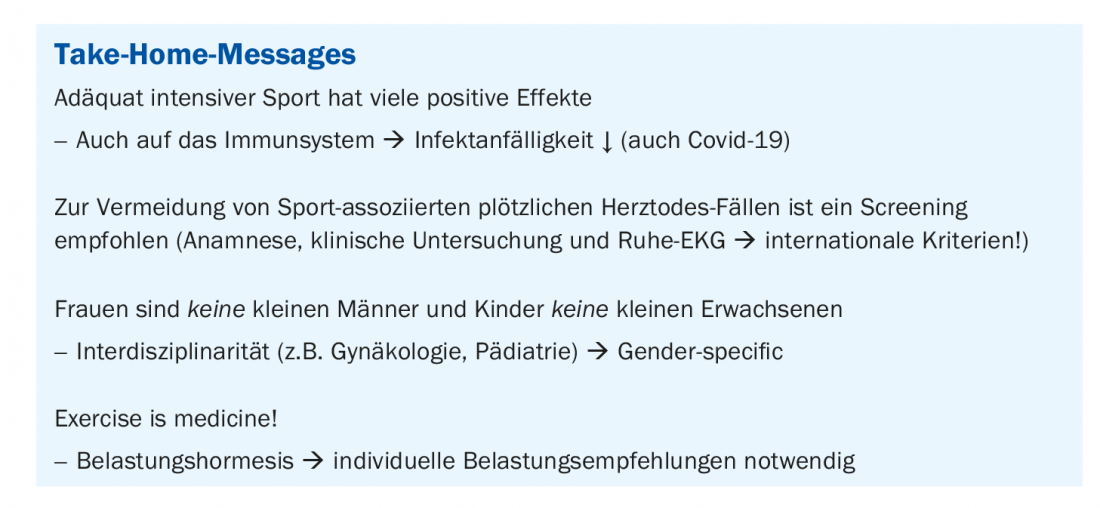
Sport is good for your health, but can too much sport even make you sick? Prof. Dr. Johann Scher, Chief Physician and Head of the University Center for Prevention and Sports Medicine at the University Hospital Basel, explains how much sport is optimal, what sudden cardiac death is all about and how re-integration into sport can be carried out with acceptable risk after infection with SARS-CoV-2.
Physical activity confers a wealth of well-documented health benefits, whereas physical inactivity is a leading risk factor for cardiovascular morbidity and mortality. According to Prof. Johann Scher, MD, the dose of physical activity required to achieve these benefits is relatively modest and corresponds to moderate-intensity exercise ≤60 min, ≤60% VO2max, on a single or regular basis. Most athletes exercise at levels and intensities that are at least 5 to 10 times the general recommendations for physical activity [1].
Immune cells that respond most strongly to exercise and experience acute mobilization into the bloodstream during physical exertion are natural killer (NK) cells. During physical exertion, the concentration of circulating immune cells increases more markedly than the increase in T and B cells. To explain this increase in immune cells, it is hypothesized that catecholamine levels, which also increase with moderate to high intensity exercise, promote the mobilization of immune cells into the bloodstream. At the end of training, the induced myokine levels should influence the redistribution and activation of immune cells. Recently, this strain-dependent mobilization of NK cells was found to play a central role in strain-mediated protection against cancer [2].
Covid-19: Sports and Back-to-Sports
Immune profiling of Covid-19 patients has revealed numerous alterations in innate and adaptive immunity. In one study, the immune profile of patients with mild and severe Covid 19 pneumonia was compared with that of patients without SARS-CoV-2 pneumonia (HAP) and with healthy controls, using longitudinal high-dimensional single-cell spectral cytometry and algorithm-based analysis. Covid-19 and non-SARS CoV-2 pneumonias both showed increased emergency myelopoiesis and had features of adaptive immune paralysis. However, pathological immune signatures indicative of T cell exhaustion occurred only in Covid-19. Integration of single-cell profiles with a predicted binding capacity of SARS-CoV-2 peptides to the HLA profile of patients further linked covid-19 immunopathology to impaired viral recognition. In terms of clinical translation, the frequency of circulating CD56+T cells has been identified as a predictive biomarker for disease outcome [3].
Although athletes are not considered to be in the risk groups for a severe course of covid-19 disease based on current evidence, this does not rule out the possibility that they may still become infected with SARS-CoV-2. Some examples from organized sports show that in individual cases more severe courses are possible in otherwise fit and initially healthy athletes. These can be associated with severe acute and probably chronic health damage. Particularly for affected competitive and ambitious recreational athletes, the question therefore arises as to how the re-integration into sport can be carried out with acceptable risk after infection with SARS-CoV-2. The flowcharts “SARS-CoV-2 – Return to training and competition” can be a first guideline for clarifying the fitness for sports and the re-entry into training and competition after an infection. For example, a SARS-CoV-2 positive athlete with an asymptomatic course should take a five-day break from sports. This five-day rest period should be followed by a history and physical examination, as well as a resting ECG and laboratory testing, because of the possible myocardial involvement in the setting of SARS-CoV-2 infection, which is associated with an increased risk of sudden cardiac death. SARS-CoV-2 positive athletes who are symptomatic must be symptom-free for an additional 48 hours. Furthermore, depending on the clinical symptoms, additional imaging should be performed.
Sudden cardiac death during sports
Occasionally, intense athletic activity has been associated with sudden deaths in athletes who have dormant but potentially terminal heart disease. Despite the publicity of such disasters, the sport’s reputation remains untarnished because most deaths are due to an underlying cardiac abnormality in which the sport is merely a trigger for a fatal arrhythmia and not the actual cause of death.
In athletes ≤35 years of age, possible triggers include diseases of the myocardium, heart valves, aorta, and coronary arteries. For example, changes in the genetic makeup can lead to hypertrophic cardiomyopathy (HCM), and arrhythmogenic right ventricular cardiomyopathy (ARVC/D) can also be the cause of sudden cardiac death. Heart valves that are defective from birth lead to increased backflow of blood into the heart (valvular insufficiency) or increase the pressure in the heart (valvular stenosis). Sometimes coronary arteries are also mislocated. At rest, these diseases usually cause no symptoms; they often go undetected. Under heavy load, on the other hand, the heart muscle is not supplied with sufficient oxygen and dangerous cardiac arrhythmias with fatal consequences can occur. Therefore, current screening recommendations in athletes ≤35 years of age include a medical history, physical examination, and resting ECG.
In athletes ≥35 years of age, atherosclerosis is the most common cause of sudden cardiac death, accounting for approximately 85%. In this process, the coronary arteries narrow more and more due to deposits (plaques) of cholesterol, connective tissue and calcium. If these plaques rupture, blood clots sometimes form and the blood vessel becomes blocked. A heart attack occurs, which can be associated with life-threatening cardiac arrhythmias. Therefore, in addition to the current screening recommendations (history, physical examination, and resting ECG), an exercise ECG is recommended [4].
Although the ECG increases the ability to detect underlying cardiovascular disease associated with sudden cardiac death (SCD), the ECG has limitations as a diagnostic tool in both sensitivity and specificity. In particular, the ECG is unable to detect anomalous coronary arteries, premature coronary atherosclerosis, and aortopathies. In some cases, patients with cardiomyopathies, particularly arrhythmogenic right ventricular cardiomyopathy (ARVC), may also have a normal ECG. Thus, an ECG cannot detect all conditions that predispose to SCD. In addition, interobserver variability among physicians remains a major problem. Therefore, to improve accuracy in detecting potentially life-threatening cardiac disease in athletes while limiting false-positive results, ECG interpretation standards have been adjusted (Fig. 1) [5].

Movement is medicine
However, it is generally accepted that regular physical activity is beneficial for cardiovascular health. Frequent exercise is strongly associated with a decrease in cardiovascular mortality as well as cardiovascular disease risk. Physically active individuals have lower blood pressure, higher insulin sensitivity, and a more favorable plasma lipoprotein profile. In addition, regular physical activity is also associated with the prevention of various neoplastic diseases, depression and dementia. The physiological mechanisms underlying the observed benefits of physical activity have been extensively documented (review 1) [6].
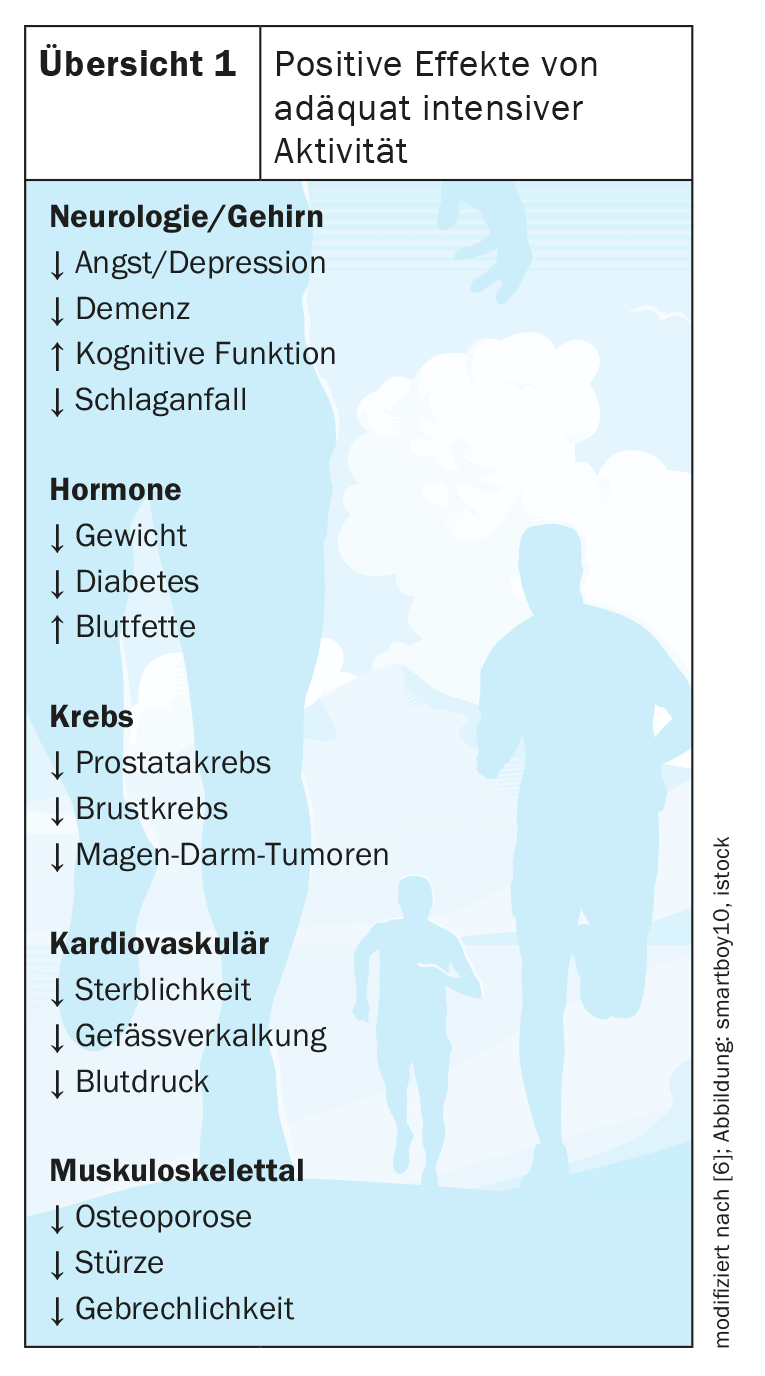
Several in vivo and in vitro studies have shown beneficial effects on fibrinolysis, platelet function, and platelet aggregation, which may explain the lower prevalence of cardiovascular disease with moderate exercise. Sport animal models show that repeated physical activity suppresses atherogenesis and increases the availability of vasodilatory mediators such as nitric oxide. Exercise also ameliorates the age-related decline in left ventricular and aortic compliance and elasticity, which may predispose to cardiovascular morbidity in older age. This is because aging is also an important risk factor for cardiovascular disease beyond simple cumulative exposure to traditional risk factors. In the large arteries, advancing age is associated with biochemical and histological changes that lead to stiffening of the vessels. Such changes in hemodynamics have been associated with dementia and cardiovascular and renal disease. This age-related stiffening of the aorta in a healthy state is reversible by early lifestyle modification with regular aerobic exercise. Cross-sectional studies have shown that lifelong athletes have more distensible peripheral arteries, and that relatively brief (<3 months) supervised aerobic exercise interventions have a positive effect on brachial blood pressure (BP) and peripheral artery stiffness [7].
The dose makes the difference!
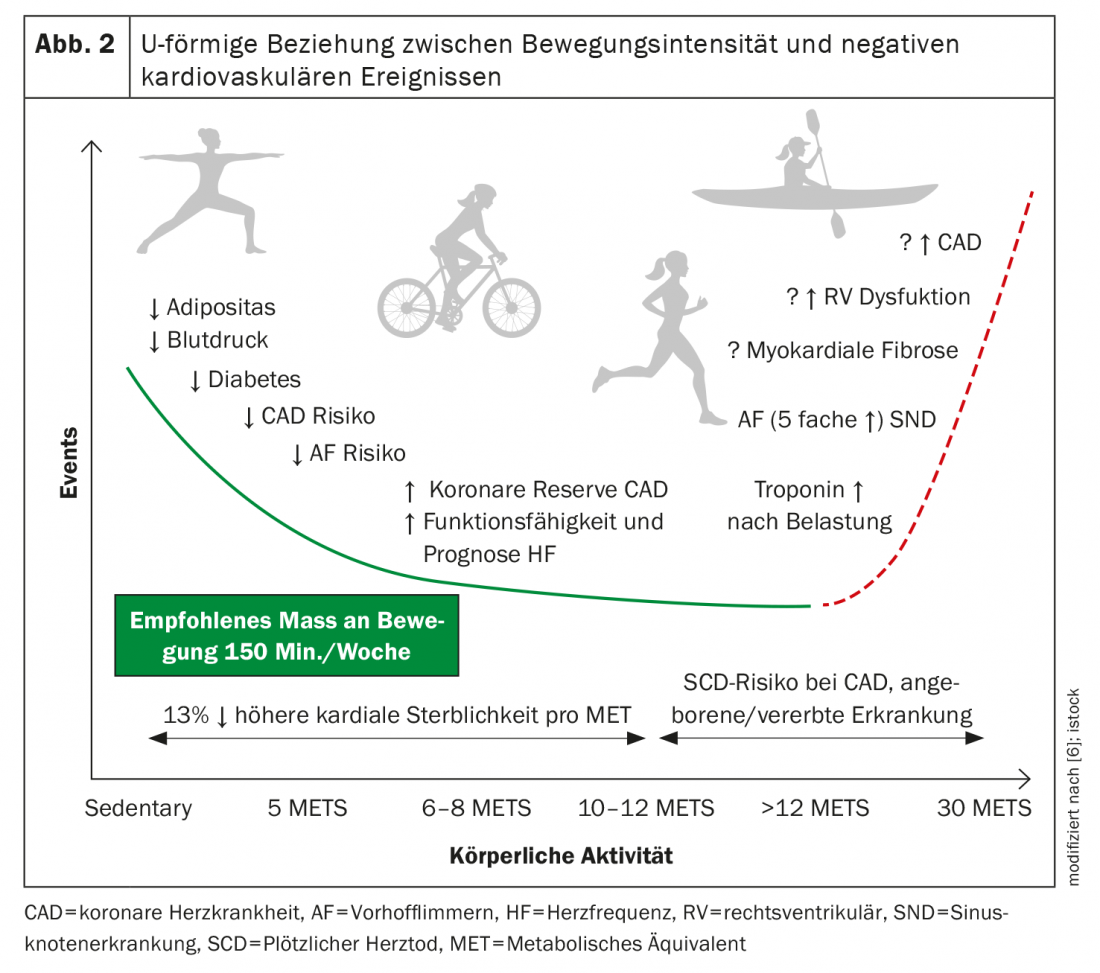
Although moderate levels of physical activity have been found to be consistently associated with a reduction in cardiovascular disease risk, there is evidence that continuous high levels of exercise, such as running a marathon, can have adverse effects on cardiovascular health.
Recent data suggest a U-shaped relationship between exercise intensity and adverse cardiovascular events, with moderate exercise being better than no exercise but vigorous exercise being harmful in some individuals (Fig. 2) [6]. A recent prospective study collected mortality data from more than 1000 apparently healthy joggers aged 20 to 86 years and about 4000 sedentary healthy controls. The researchers described a U-shaped relationship between all-cause mortality and the dose of jogging, expressed by pace, amount, and frequency of jogging. Light joggers who jogged 1 to 2.4 hours per week, divided into three sessions, had lower mortality than sedentary non-joggers, while the mortality rate of more rigorous joggers was not statistically different from that of the sedentary group. Based on this study, it can be concluded that the greatest benefits of physical activity for the cardiovascular system come from relatively light physical activity.
Gender-specific medicine!
Although it has been accepted overall that most musculoskeletal injuries are sport-specific rather than gender-specific, Scherr says it is also important to consider that gender differences in anatomical structure play a role in biomechanical alignment and function. In addition to a difference in skeletal muscle mass, which is approximately 40% higher in males than females, females have a wider pelvis, greater hip and knee valgus, and greater laxity and rearfoot pronation compared to males of the same age. Accordingly, the lower extremity of women seems to be biomechanically less favorable. For this reason, female athletes are also four to eight times more likely to tear their cruciate ligaments than male athletes. However, special prevention programs can help improve trunk stability and strengthen leg axis stability muscularly.
And for some children and young people, too, sport is more than just a hobby. However, depending on their age, children and adolescents are still in the process of physical growth. Incorrect training can cause lasting damage to the bone structure and the risk of injury should not be underestimated in this respect. The Society for Pediatric Sports Medicine is therefore committed to advancing pediatric sports medicine and therapy through sports in childhood and adolescence.
Congress: FomF General Internal Medicine Update Refresher
Literature:
- Prof. Dr. Johannes Scherr: Sports Medicine – The Most Important for Practice. General Internal Medicine Update Refresher, FomF, 05/21/2022.
- Idorn M, Hojman P: Exercise-Dependent Regulation of NK Cells in Cancer Protection. Trends Mol Med 2016; doi: https://doi.org/10.1016/j.molmed.2016.05.007.
- Kreutmair S, et al: Distinct immunological signatures discriminate severe COVID-19 from non-SARS-CoV-2-driven critical pneumonia. Immunity 2021; doi: https://doi.org/10.1016/j.immuni.2021.05.002.
- Pelliccia A, et al: 2020 ESC Guidelines on sports cardiology and exercise in patients with cardiovascular disease: The Task Force on sports cardiology and exercise in patients with cardiovascular disease of the European Society of Cardiology (ESC). Eur Heart J 2021; doi: 10.1093/eurheartj/ehaa605.
- Sharma S, et al: International recommendations for electrocardiographic interpretation in athletes. Eur Heart J 2018; doi: 10.1093/eurheartj/ehw631.
- Merghani A, et al: The U-shaped relationship between exercise and cardiac morbidity. Trends Cardiovasc Med 2016; doi: 10.1016/j.tcm.2015.06.005.
- Bhuva A, et al: Training for a First-Time Marathon Reverses Age-Related Aortic Stiffening. J Am Coll Cardiol 2020; doi: 10.1016/j.jacc.2019.10.045.
HAUSARZT PRAXIS 2022; 17(7): 24-26