Once joint damage has occurred in the course of rheumatoid arthritis, it can no longer be reversed with medication. Therefore, it is important to use basic therapeutics as early as possible. If conventional substances do not have sufficient effect or are not tolerated, biologics are used. The following article provides an overview of therapeutic strategies.
In rheumatoid arthritis (RA), inflammation-related joint destruction begins very early in the course of the disease, usually in the first few months. The joint damage or secondary arthrosis (Fig. 1) is irreversible and cannot be reversed with medication. The earlier basic therapeutics are used, the better the response.
Interdisciplinary collaboration with physical and occupational therapy and sometimes rheumatologic surgery is essential for good management. Care must be taken to coordinate treatment interventions within these areas, especially in the interaction between the primary care provider and the rheumatologist.

Early diagnosis
Today, full remission is a quite realistic goal and can be achieved more easily early than late in the course. Because basic therapy should ideally be initiated within the first three months after symptom onset, early diagnosis is central. At the beginning of the disease, it takes a lot of experience to make the diagnosis correctly by means of the typical symptoms, the joint involvement pattern and the additional examinations (laboratory with autoantibodies, arthrosonography, X-rays).
Treatment approaches
Basic medications: Basic medications are essential for adequate control of disease activity in most cases. In the longer term, they are much less toxic than glucocorticoids, provided they are used skillfully. They not only reduce the symptoms of inflammation, but ideally slow down and stop the erosive-destructive process. With conventional synthetic substances, the effect usually sets in with a latency of about two to three months.
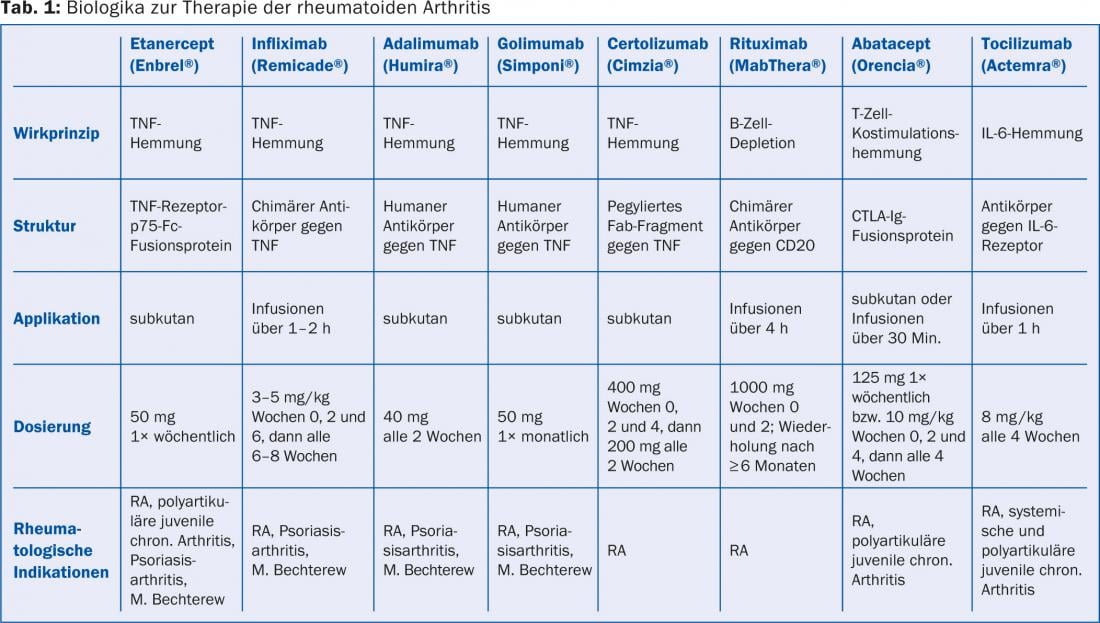
The range of basic therapeutics is constantly increasing. Commonly used conventional synthetic base drugs include methotrexate, leflunomide (Arava® and generics), sulfasalazine (Salazopyrin® EN), and hydroxychloroquine (Plaquenil®). Recently, the selective synthetic drug tofacitinib (Xeljanz®) has also become available, which inhibits intracellular enzymes, namely the so-called Janus kinases. It is used perorally with or without conventional base medications (e.g., methotrexate). In addition, there are the biologics (Tab. 1), which have led to a real revolution in the therapy of RA in the last 15 years: Today, a well effective and tolerable medication can be found for most patients, but often combinations are necessary. Today, achieving remission is a thoroughly realistic goal.
Matching therapy to individual patient needs is challenging. It requires a lot of experience. Therefore, the treatment should always be carried out together with a specialist in rheumatology.
Methotrexate is usually the first choice, although it is best given together with, for example, hydroxychloroquine, leflunomide or biologics (two-drug combinations). Combinations of three or even four are also possible. The different mechanisms of action of the individual substances achieve an additive and in some cases even synergistic effect, which allows the dosage of the individual substances to be kept lower (fewer side effects). Combination therapies require a lot of experience, including monitoring.
Methotrexate, leflunomide, tofacitinib and all biologics have an immunosuppressive effect. To avoid an excessive increase in the risk of infection, combination therapies should not contain more than two of these immunosuppressants or more than one biologic. High steroid dosages should also be avoided. Instructing the patient to promptly report any symptoms suspicious of infection and to stop any biologic is essential. If a suspected infection is corroborated by a CRP rise, prompt hospitalization is appropriate if the focus of infection remains unclear or parenteral antibiotic therapy or monitoring is required.
Biologics specifically intervene in the inflammatory process at the molecular level. Possibilities include inhibition of TNF (TNF inhibitors) or T-cell costimulation (abatacept), reduction in activity of interleukin-6 (tocilizumab), and B-cell depletion (rituximab). The longest experience has been with TNF inhibitors. Clinically, these are only slightly more effective than methotrexate in monotherapy, but their onset of action is much faster: systemic (humoral) inflammatory activity is suppressed within only two days, which often manifests itself in an abrupt improvement of general symptoms (fatigue, exhaustion, and inappetence).
The antierosive effect of TNF inhibitors is clearly superior to that of methotrexate. They can also be combined very well with synthetic basic drugs and especially methotrexate, which on average leads to an even better clinical and anti-erosive effect.
TNF inhibitors are injected subcutaneously or infused intravenously. For the most part, they are well tolerated. The main side effects include skin reactions at the injection site or infusion reactions. The risk of infection is approximately doubled under TNF inhibition, and opportunistic infections are possible, especially with intracellular pathogens. Because tuberculosis reactivation can occur, prior screening for tuberculosis is necessary. Pneumococcal and annual flu vaccinations are useful. Possible ports of entry, such as periodontitis or skin lesions (including mycoses), must be eliminated before starting therapy.
After failure of conventional baseline therapy, abatacept and tocilizumab may be considered instead of TNF inhibitors. Another indication of these two substances as well as of rituximab is the insufficient effect of anti-TNF therapy. Abatacept has an excellent tolerability profile. Tocilizumab suppresses systemic (humoral) inflammatory activity the most of all biologics. Rituximab has the advantage that its cycles of therapy need not be more frequent than six months, and it works best in rheumatoid factor- and anti-CCP antibody-positive patients. Similar precautions apply to abatacept, tocilizumab, and rituximab as to TNF inhibitors, but opportunistic infections occur less frequently. To be noted: An infection-related CRP increase may be inhibited by tocilizumab (CAVE underestimation of severity of infection).
Biologics are expensive due to their complex production, which is why they are only approved if a previous therapy with conventional substances has proven to be insufficient. A cost approval must be obtained from the health insurance company in advance.
Glucocorticoids: Steroids are indicated only for short-term bridging until the onset of action of the basic medications and for long-term low-dose use (for example, prednisone ≤ 7.5 mg/d) when the effectiveness of the basic therapeutics is insufficient. A sustained-release form of prednisone (Lodotra®) has recently become available. This is taken before bedtime and releases prednisone with a delay of several hours, making it fully effective when the patient gets up in the morning. The rapid and strong anti-inflammatory effect does tempt people to use glucocorticoids in higher doses for longer periods. However, monotherapy with glucocorticoids is obsolete today because prolonged use at higher doses is associated with severe toxicity (e.g., osteoporosis). If individual joints are dominant, intraarticular steroid injections are appropriate.
Monitoring for therapy optimization
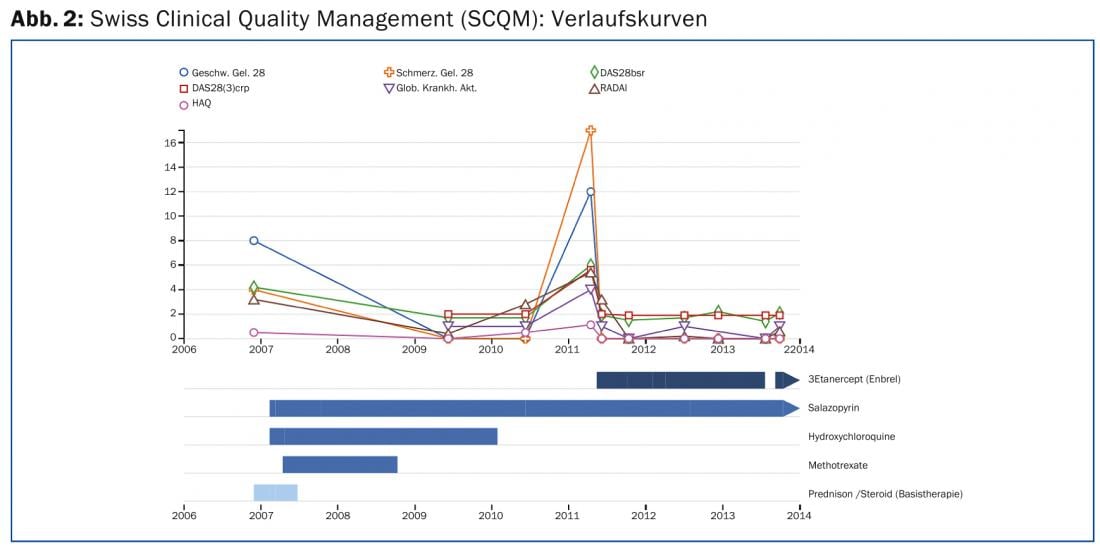
In any case, continuous monitoring and adjustment of the medication together with a specialist in rheumatology is necessary, which is best done within the framework of quality management. For this purpose, the Swiss Clinical Quality Management in Rheumatic Diseases (SCQM) registry is available in Switzerland (www.scqm.ch). As a measurement improvement system, the SCQM is readily useful in practice, and it provides valuable “real life” register data. By means of questionnaires, which are regularly completed by the patient and rheumatologist on the Internet or on paper, the course of inflammatory activity, joint damage and the effects of the disease can be recorded in a standardized manner. X-ray and laboratory tests are also part of the assessment. The centralized evaluations allow the therapy to be continuously optimized (Fig. 2) . The guidelines of the Swiss Society of Rheumatology (www.rheuma-net.ch/Richtlinien) provide a summary of the necessary monitoring measures for the individual basic drugs.
Comorbidities
Osteoporosis and arteriosclerosis are the most significant comorbidities. Bisphosphonates are used under continuous steroid therapy already when moderate to severe osteopenia is present, i.e., not only when there is evidence of osteoporosis (recommendations “Steroid Osteoporosis” at www.rheuma-net.ch/Richtlinien). In RA, there is an acceleration of atherosclerosis. Cardiovascular events occur about twice as often as in the normal population, so risk factors (diabetes, smoking, hypertension, and hypercholesterolemia) should be targeted and aggressively addressed.
Adrian Forster, MD
Literature:
- Schneider M, Krüger K: Rheumatoid arthritis – early diagnosis and disease management. Dtsch Ärztebl Int 2013; 110: 477-484.
- Smolen JS, et al: EULAR recommendations for the management of rheumatoid arthritis with synthetic and biological disease-modifying antirheumatic drugs: 2013 update. Ann Rheum Dis 2014; 73: 492-509.
- Bykerk VP, Schoels MM: Treatment strategies for early rheumatoid arthritis. Curr Opin Rheumatol 2013; 25: 375-383.
- Gramling A, O’Dell JR: Initial management of rheumatoid arthritis. Rheum Dis Clin North Am 2012; 38: 311-325.
CONCLUSION FOR PRACTICE
- Starting basic therapy as early as possible is central to prognosis. The goal of treatment is remission.
- If conventional basic drugs do not have enough effect, biologics or tofacitinib are indicated.
- Monotherapy with steroids is out.
- It is crucial that the risk of concomitant diseases such as osteoporosis or arteriosclerosis is detected and reduced at an early stage.
A RETENIR
- Un traitement de base instauré le plus tôt possible est crucial pour le pronostic. Le but du traitement est la rémission.
- Si les médicaments de base classiques ne sont pas suffisamment efficaces, les agents biologiques ou le tofacitinib sont indiqués.
- La monothérapie par des stéroïdes n’est plus d’actualité.
- Il est crucial d’appréhender le risque de comorbidités telles que l’ostéoporose ou l’artériosclérose et de le réduire.
HAUSARZT PRAXIS 2014; 9(4): 12-15











