The treatment goal for intracranial aneurysms is to eliminate the aneurysm. The main treatment methods consist of clipping and coiling. Several aneurysm- and patient-specific factors must be considered when making treatment decisions.
The goal of intracranial aneurysm treatment is to completely and as permanently as possible separate the aneurysm from the bloodstream to prevent future rupture or re-rupture with subarachnoid hemorrhage (with the lowest possible risk of morbidity and mortality). Various surgical and minimally invasive treatment techniques are available for this purpose, in particular direct microsurgical clipping, endovascular treatment with coils with or without additional devices (e.g. intracranial stents), or a combination of these techniques. In the following, we will outline the advantages and disadvantages of each treatment method with a focus on the “decision to clip (microsurgical therapy) or coiling (endovascular therapy).”
Microsurgical clipping
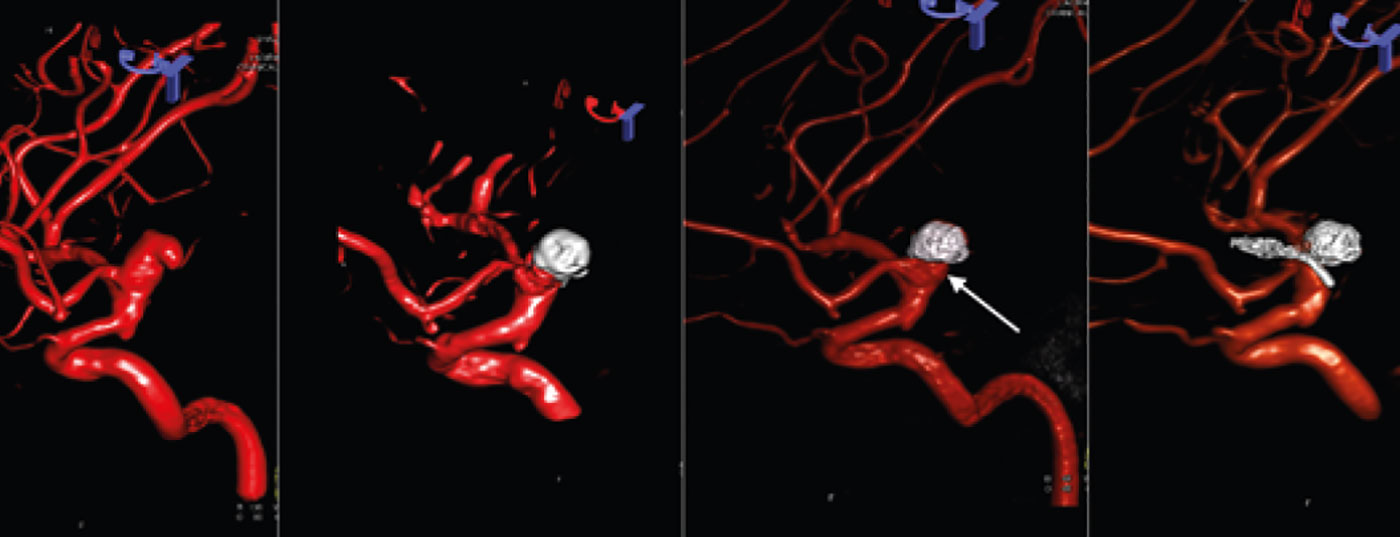
Microsurgical clipping involves placing a small metallic clip over the neck or base of the intracranial aneurysm during an open craniotomy. This method was first introduced in the USA by Walter Dandy in 1937. Since then, a variety of clips with different shapes and sizes have been developed. The clip is selected depending on the size, configuration and location of the intracranial aneurysm. A spring mechanism allows the placed clip to exclude the aneurysm from the supporting vessel, thus preventing a possible rupture (Fig. 1).
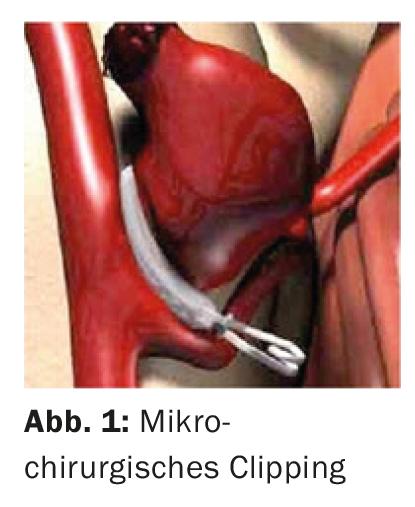
Intraoperative angiography [1], electrophysiological monitoring, tailored craniotomies, and indocyanine green videoangiography [2] have significantly improved the results of the surgical method. Also, cardiac frequency overstimulation and adenosine are used to induce asystole and relative hypotension to provide a better view of the clip over the aneurysm neck for optimal placement.
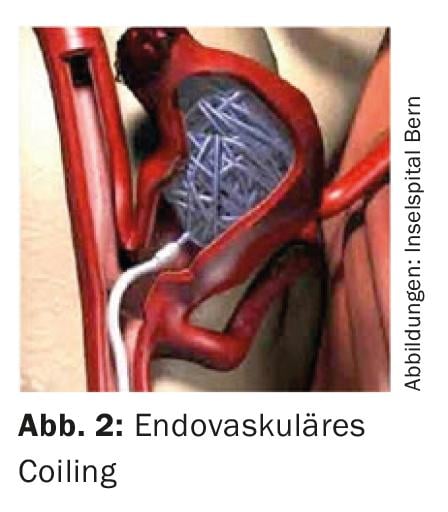
Endovascular treatment (coiling)
Minimally invasive endovascular treatment of intracranial aneurysms with electrolytically detachable coils was introduced clinically by Guido Guglielmi and colleagues in 1991 as an alternative to microsurgical clipping [3]. Through a minimally invasive transfemoral approach, the aneurysm is catheterized with a microcatheter under fluoroscopic guidance and stuffed with platinum coils. The coils thereby lead to intra-aneurysmal thrombosis and thus to the elimination and closure of the aneurysm (Fig. 2). Since their introduction in the 1990s, endovascular treatment techniques have undergone rapid development – from so-called balloon and stent-assisted coiling to flow-diverting stents (“flow diverters”) and currently intra-saccular occlusion systems (“intrasaccular flow disruptors”), which are increasingly expanding the spectrum of intracranial aneurysms that can be treated endovascularly.
Clipping versus Coiling
Currently, three prospective randomized trials comparing microsurgical versus endovascular therapy for ruptured intracranial aneurysms are available [4–6], with the ISAT (International Subarachnoid Aneurysm Trial) study in particular being a landmark study. Randomized studies of incisional nonruptured intracranial aneurysms are not yet available. There are a number of prospective studies demonstrating the efficacy and safety of endovascular treatment.
Despite different methodologies in the three randomized trials of ruptured intracranial aneurysms, similar results were found in favor of better clinical outcome in patients treated with endovascular therapy. A meta-analysis of the three trials [7] demonstrated a significantly lower rate of poor neurological outcome 12 months after treatment in a total of 2723 included patients (risk ratio 0.75; 95% CI 0.65-0.87), with an absolute risk reduction of 7.8% with respect to severe disability or death (NNT 13). The rate of rebleeding within the first month was higher in patients with coiling, but there was no statistical difference in mortality between the two groups. Although endovascular therapy has shown an advantage in the short to medium term in the treatment of intracranial aneurysms in several studies, its disadvantage lies in the higher rates of aneurysm recanalization (approximately 10-20%) and the associated higher rates of retreatment (approximately 10%), as well as the higher risk of rebleeding compared with microsurgical therapy.
In contrast to endovascular therapy, reperfusion of the aneurysm occurs less frequently after microsurgical clipping, so clipping appears superior to endovascular therapy in terms of long-term occlusion rate. The CARAT study of re-ruptures of intracerebral aneurysms after treatment showed a re-rupture rate of 1.8%, similar to the ISAT study of 1.7% [8]. However, the long-term data of the ISAT trial [9] show that the initial treatment effect in ruptured aneurysms is nevertheless maintained for more than ten years. Further long-term data, especially on endovascular treatment of unruptured aneurysms, are therefore needed to evaluate the stability of endovascular aneurysm treatment and long-term protection against aneurysm rupture.
Based on these studies, endovascular therapy is considered the first-line therapy for ruptured aneurysms if simply possible.
Choice of treatment method and patient selection
In the case of an intracranial aneurysm, various factors must be considered and weighed against each other to determine the optimal treatment strategy for the individual patient (Table 1). Aneurysm-specific factors include anatomic location, size, morphology, especially the positional relationship of outgoing vessels to the aneurysm, partial thrombosis, and wall calcifications. Patient-specific factors include patient age, comorbidities, and clinical neurologic status.
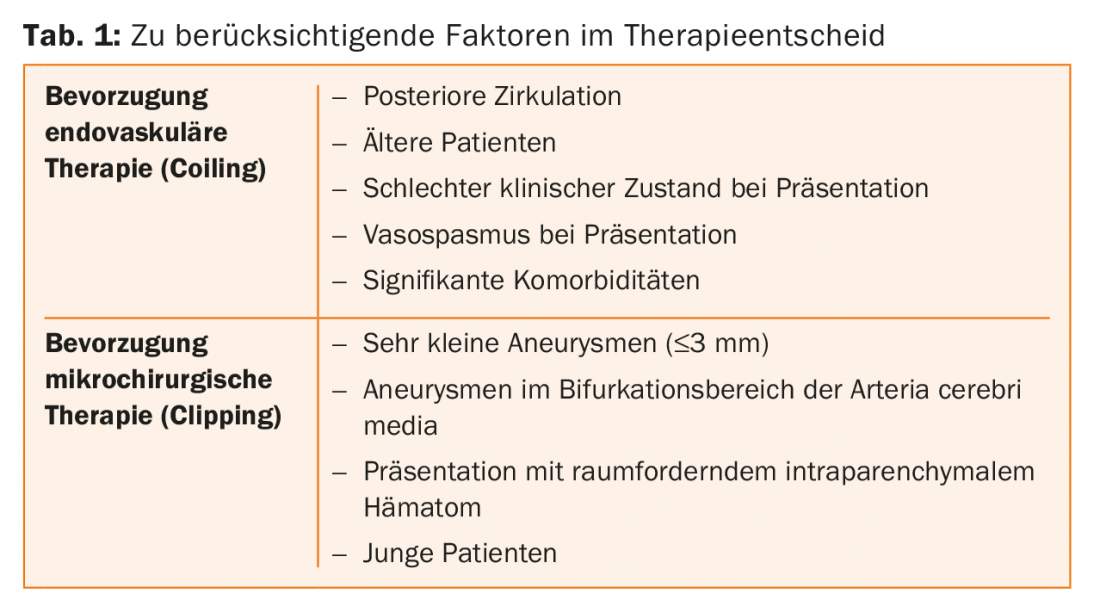
Size and morphology of the aneurysm: The morbidity of both endovascular and surgical treatment is related to the size of the aneurysm. With the surgical method, morbidity is directly proportional to the size of the aneurysm; with endovascular treatment, the success rate is lower for extremely large aneurysms. Regarding the size of an intracranial aneurysm, the limitation of endovascular therapy in very small aneurysms is whether a coil of appropriate size (smallest available coil 1× 1 mm) can be placed in the aneurysm or whether a stent or “flow diverter” must be used.
Anatomical location of the aneurysm: The anatomical location of the aneurysm plays a major role in the decision between clipping and coiling, as it influences the safety and efficacy of both treatment modalities. The complication rate of microsurgical treatment is higher for aneurysms of the posterior cerebral vessels than for aneurysms of the anterior circulation of similar size. Most published series on microsurgical clipping report mortality between 3-30% and morbidity between 7-40% [10]. In contrast, the complication rate of endovascular treatment is similar for anterior and posterior cerebral aneurysms. For both ruptured and nonruptured intracranial aneurysms of the posterior circulation, several studies have shown a better outcome for endovascularly treated patients, with morbidity rates of 3.7-5.1% and mortality rates of 4.9-9.4%. On the other hand, aneurysms in the bifurcation region of the middle cerebral artery are on the whole more likely to be clipped microsurgically than coiled. This is mainly due to the frequent broad-based anatomy of the aneurysms as well as the frequent inclusion of outgoing branches from the aneurysm neck. These are morphologic factors that make endovascular treatment with coils more difficult without additional devices such as remodeling stents (which is why higher recanalization rates or higher peri-interventional risk should be expected). From a surgical point of view, on the other hand, aneurysms in the bifurcation region of the middle cerebral artery are usually easy to reach for microsurgical clipping, and precise clip application while keeping the outgoing branches open is possible.
Special circumstances: Although most aneurysms can be treated with microsurgical or endovascular therapy, there are also rare aneurysms that require a special treatment approach: These are giant calcified aneurysms, large aneurysms with intraluminal thrombus, aneurysms in which the vessel drains directly from the aneurysm, and dissecting, fusiform, and mycotic aneurysms. These can be treated by microsurgery or endovascular treatment, depending on the clinical indication, and in some circumstances a bypass may also be necessary. Treatment of partially thrombosed intracranial aneurysms-especially when they are large-can be challenging for both therapeutic modalities. Endovascular therapy has the disadvantage that a tight and stable closure of the aneurysmal lumen is difficult if the intraluminal thrombus changes over time. In these cases, microsurgery is a good alternative if the aneurysm neck is easily accessible for clip application. Wall calcifications in the neck area are often a contraindication for clipping, as correct placement of the clip at the aneurysm neck is difficult here due to the calcium shell.
Patient-specific factors: Several studies have shown that patient age is an important determinant of outcome of aneurysm treatment, with older patients being more likely to benefit from less invasive endovascular treatment. A subgroup analysis of the previously mentioned ISAT trial showed an increased rate of disability or death in elderly patients with ruptured intracranial aneurysms in the microsurgical compared with the endovascular treatment group (43.9% vs. 39.9%). On the other hand, in rather younger patients, especially with incisional unruptured as well as partially ruptured aneurysms, microsurgical therapy seems to offer advantages – this due to the presumably more stable long-term occlusion rate and generally less frequent peri-operative complications (compared with older patients).
Patients in poor clinical-neurologic status after severe subarachnoid hemorrhage and patients with vasospasm present are more likely candidates for endovascular treatment.
If patients require emergency surgical hematoma evacuation after aneurysm rupture with additional space-occupying intraparenchymal hematoma, it is usually reasonable to also clip the ruptured aneurysm during the same operation.
In patients with both ruptured and unruptured intracranial aneurysms with severe comorbidities, endovascular therapy is more preferred because of the lower peri-operative risks.
Recanalization of the aneurysm
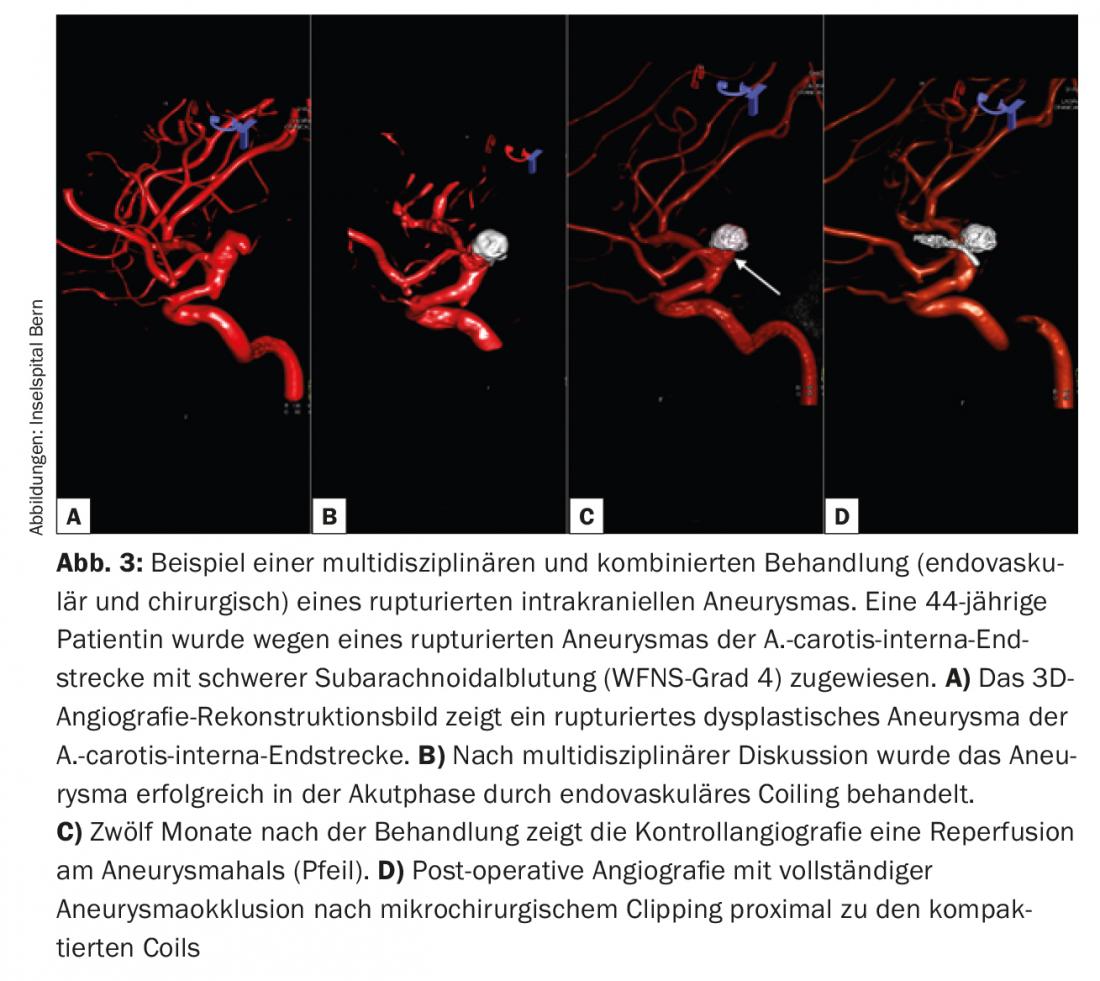
The ISAT study showed that 17% of patients needed follow-up treatment for incomplete occlusion or recurrence, of which 54% required surgical intervention (Fig.3). The CARAT trial showed an annual re-treatment rate for endovascularly treated patients in the first, second, and subsequent years of 13%, 4.5%, and 1.1%, respectively-compared with 2.6% in the first and 0% in the later years for those who underwent microsurgical clipping [8].
Competence and multidisciplinarity
Other decisive factors in the choice of therapy for intracranial aneurysms are the experience and the treatment volume of a center or a hospital. Of the individual neurosurgeon and interventional neuroradiologist on the treatment team. Several studies have shown an association between low morbidity and mortality rates and treatment at high-volume centers and by skilled surgeons for both microsurgical and endovascular treatment of ruptured and unruptured intracranial aneurysms [11]. Therefore, to ensure the most optimal treatment with the least morbidity and mortality, patient selection and an individualized choice of treatment modality should be made in an interdisciplinary manner between treating neurosurgeons and interventional neuroradiologists at a dedicated neurovascular center. Accordingly, microsurgical clipping and endovascular treatment methods are basically complementary and noncompeting treatments for intracranial aneurysms.
Take-Home Messages
- The treatment goal for intracranial aneurysms is complete and, if possible, permanent elimination of the aneurysm.
- The main treatment modalities consist of direct microsurgical clipping and various endovascular therapies, particularly coiling.
- Randomized trials are available for the treatment of ruptured intracranial aneurysms but not for incisional unruptured aneurysms.
- When deciding on a treatment method, various aneurysm-specific as well as patient-specific factors must be considered.
- Patient selection and an individualized choice of treatment modality should be made on an interdisciplinary basis at a dedicated neurovascular center. Accordingly, microsurgical clipping and endovascular treatment methods are basically complementary and not competing procedures.
Literature:
- Chiang VL, et al: J Neurosurg 2002; 96: 988-992.
- Raabe A, et al: J Neurosurg 2005; 103: 982-989.
- Guglielmi G, et al: J Neurosurg 1991; 75(1): 8-14.
- Vanninen R, et al: Radiology 1999; 211(2): 325-336.
- Molyneux A, et al: Lancet 2002; 360(9342): 1267-1274.
- McDougall C, et al: J Neursurg 2012; 116(1): 135-144.
- Lanzino G, et al: AJNR 2013; 34(9): 1764-1768.
- Johnston SC, et al: Stroke 2008; 39: 120-125.
- Molyneux A, et al: Lancet 2015; 385(9969): 691-697.
- Wirth FP, et al: Neurosurgery 1983; 12: 507-511.
- Berman M, et al: Stroke 2003; 34(9): 2200-2207.
InFo NEUROLOGY & PSYCHIATRY 2017; 15(5): 12-16.