Pulmonary hypertension is usually a sign of more advanced stage of left heart disease (PH-LHD). The central characteristic of PH-LHD is an elevated pulmonary arterial wedge pressure of >15 mmHg. In highly selected cases, therapy approved for pulmonary arterial hypertension, i.e. phosphodiesterase 5-inhibitors (PDE5i), might be indicated as a bridge to heart transplantation and after left ventricular assist device in case of severe impaired right ventricular function. In cases of moderate to severe mitral regurgitation the treatment options (surgical or transcatheter valve repair) should be evaluated in a heart team including cardiologists, cardiac surgeons and imaging specialists.
Pulmonary hypertension (PH) may be the result of all causes of left heart disease (LHD) and is usually a sign of more advanced stage of LHD (table 1). The progressive symptoms of heart failure with exercise intolerance due to PH-LHD have been shown to result in worse outcome depending on how early and effectively the LHD can be treated [1].
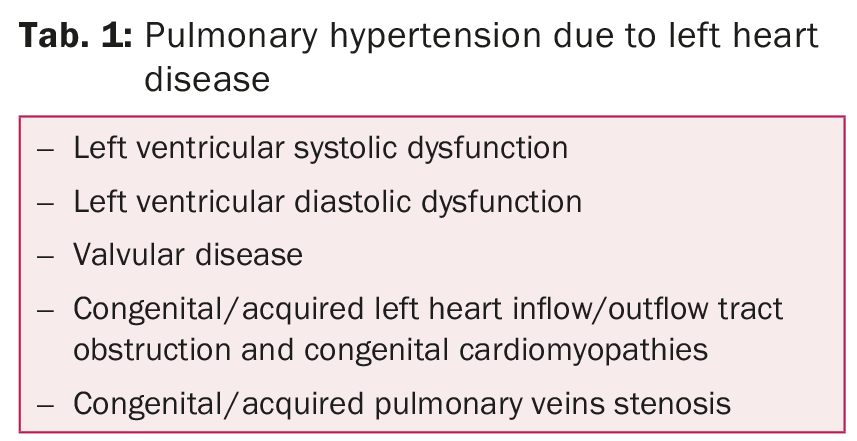
Definition of PH-LHD
PH is generally defined for all the clinical groups as a hemodynamic and pathophysiological state with increased resting mean pulmonary arterial pressure (PAPm) of ≥25 mmHg as assessed by right heart catheterization. The central characteristic of PH-LHD is an elevated pulmonary arterial wedge pressure (PAWP) of >15 mmHg owing to increased filling pressures of the left atrium and post-capillary PH.
The 2009 European Society of Cardiology and European Respiratory Society (ESC/ERS) guidelines for the diagnosis and treatment of PH define the hemodynamic characteristics of PH-LHD according to the transpulmonary gradient (TPG), the difference between PAPm and PAWP [1,2]. Post-capillary PH-LHD is either defined as passive (TPG ≤12 mmHg) or reactive (out of proportion, TPG >12 mmHg). In 10–15% of cases the hemodynamic indicates a combination of pre- and post-capillary PH [1]. However, taking only the TPG into account may lead to misclassification of the PH-LHD, influencing the therapeutic approach of the LHD.
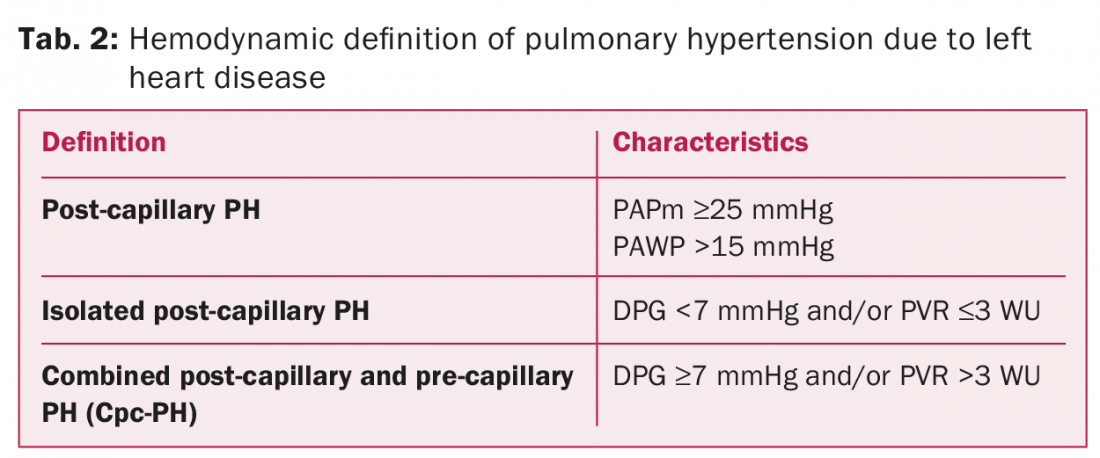
The 2015 PH-guidelines from ESC/ESR define three different hemodynamic states when interpretating PH-LHD (table 2) [3]. The main changes in the characteristics of the PH is the evaluation of the diastolic pressure gradient (DPG), the difference between PAPd and PAWP instead of TPG, and/or the peripheral vascular resistance in order to differentiate an isolated post-capillary PH (Ipc-PH) from a combined post-capillary and pre-capillary PH (Cpc-PH) (table 2).
Patients who have a pulmonary vascular resistance (PVR) exceeding five Wood units (5 WU×80 = 400 dyn×sec×m2×cm-5) or PVR-index >6 WU have an increased risk of post-operative right ventricular failure following heart transplantation [4]. Hence, pharmacological «vasodilator challenges» either directly aimed at the pulmonary arterial vasculature such as prostacyclin or in case of inadequate response, i.e. in case of very high PAWP, afterload reduction on the left heart using nitroprussid or nitroglycerin are necessary to unmask irreversibly «fixed» pulmonary arterial hypertension (PAH).
Patients with fixed, elevated peripheral vascular resistance may have concomitant lung disease, obstructive sleep apnea or chronic pulmonary thromboembolic disease that should be considered in the differential diagnosis and excluded.
Medical treatment
There is established and growing evidence in regard to medical treatment of PAH while data in PH-LHD are lacking. However, drugs with proven efficacy in PAH are increasingly being used for other forms of PH including PH-LHD i.e. phosphodiesterase 5-inhibitors (PDE5i).
The beneficial effects of PDE5i in PAH are thought to result from relatively selective vasodilatory and antiproliferative effects on the pulmonary vasculature, and on the hemodynamic in heart failure [5]. PH represents the main pathophysiological mechanism in right ventricular failure [4]. Small trials in patients with heart failure demonstrated the greatest benefit of PDE5is in patients with PH-LHD and right ventricular failure [5]. This is thought to be the result of the direct effect of PDE5i on the right ventricular myocardial contractility where PDE5 expression has been shown to be up-regulated in impaired right ventricles [6]. PDE5 inhibition may therefore play a role in the improvement of right ventricular function in heart failure and may be clinically justified in some carefully selected patients as a bridge to heart transplantation or after a left ventricular assist device support. This will be discussed in the first case report.
Case 1: A young patient with dilated cardiomyopathy
46 year old patient with known dilated cardiomyopathy since the year 2000 and left ventricular ejection fraction (LVEF) of 20%, normal right ventricular size and function, light mitral regurgitation and absence of PH in the right heart catheterization (fig. 1).
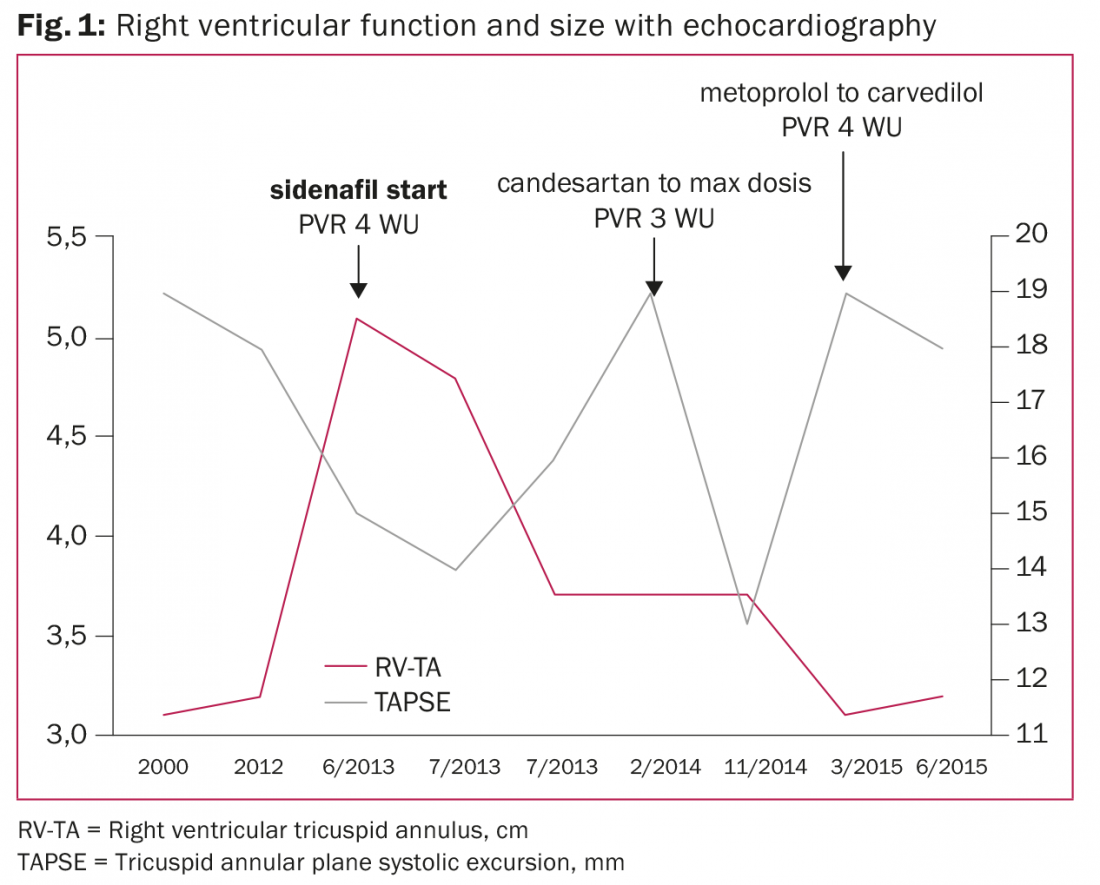
In 2012, a cardiac resynchronization therapy with defibrillator was implanted due to syncope and a new left bundle branch block. In 2013, the patient was referred to the heart failure team for evaluation due to acute biventricular cardiac decompensation, dilated right ventricle and impaired right ventricular function. The TPG was 12 mmHg but DPG was –1 mmHg indicating isolated post-capillary PH and PVR 4,4 WU (352 dyn×sec×m2×cm-5) after ilomedin vasodilation test. No systemic vasodilation pharmacological (i.e. nitroprussid or nitroglycerin) test was performed to exclude Cpc-PH or irreversible PAH. Hence, due to PH with right ventricular failure, sildenafil therapy was initiated. A work-up for heart transplantation was initiated.
Serial right heart catheterizations were performed according to the 2006 guidelines of the International Society for Heart & Lung Transplantation to determine suitability for heart transplantation in order to avoid high risk of right ventricular failure and mortality after heart transplantation [7]. Elevation of PVR was noticed in 2014 (5,7 WU down to 2,8 WU after systemic vasodilation test) and in 2015 (4,3 WU) and thereafter PVR decreased to 1,3 WU (104 dyn×sec× m2×cm-5) after continued optimization of the heart failure therapy.
Early after the initiation of sildenafil, the size of the right ventricle normalized and the right ventricular function improved during the two year period, despite intermittent progression of PH. The patient is clinically stable in NYHA class III with moderate mitral regurgitation and on the waiting list for heart transplantation.
Therapeutic options: Directed to the underlying pathology
If medical and device therapy fails to reduce the PVR <3–5 WU, and the patient remains in NYHA class III–IV, left ventricular assist device might be considered by acceptable right ventricular function [7,8]. According to the 2013 mechanical circulatory support (MCS) guidelines, PDE5i may be considered for management of right ventricular dysfunction in the setting of PH after MCS (Level of evidence IIb, C) [8]. The therapeutic options of PH-LHD should be directed to the underlying pathology of the LHD. New evidence has accumulated, diagnostic techniques and therapeutic options have changed through further development of surgical valve repair and the introduction of percutaneous interventional techniques, mainly transcatheter aortic valve implantation (TAVI) and percutaneous edge-to-edge valve repair. These changes are mainly related to aortic stenosis and mitral regurgitation.
Case 2: A 44 year old woman with dilated cardiomyopathy
The 44 year old female patient has a dilated cardiomyopathy (after alcohol abuse) since the year 2010, LVEF 30%, normal right ventricular size and moderate impaired right ventricular function. PH in the right heart catheterization (PAPm 33 mmHg) with isolated post-capillary PH (DPG 4 mmHg). The mitral regurgitation was severe (effective regurgitation orifice area 54 mm2 [reference ≥40], regurgitation volume 66,1 ml/beat [reference ≥60], pulmonary venous flow reversal) with enlargement of left ventricular end diastolic diameter (61 mm) and left atrium (47 mm).
The valve was morphologically intact, hence, fulfilling the echocardiographic criteria of a functional mitral regurgitation [9]. Heart failure therapy was initiated, and an implantable cardioverter-defibrillator (ICD) was implanted. The mitral regurgitation improved to moderate grade.
At the end of 2011, the patient was referred to the heart failure team for further evaluation due to acute pulmonary oedema and repeated ICD shocks due to non-sustained ventricular tachycardia. The mitral regurgitation was severe. The pharmacological therapy achieved was submaximal due to hypotension, the patient received instruction to discontinue alcohol consumption and adhere to strict volume/salt intake management. As shown in figure 2, during the following year 2012, the patient was hospitalized four times due to LH decompensation achieving stabilization inbetween, however with continuing severe mitral regurgitation. Due to poor compliance heart transplantation or left ventricular assist device therapy was relatively contraindicated.
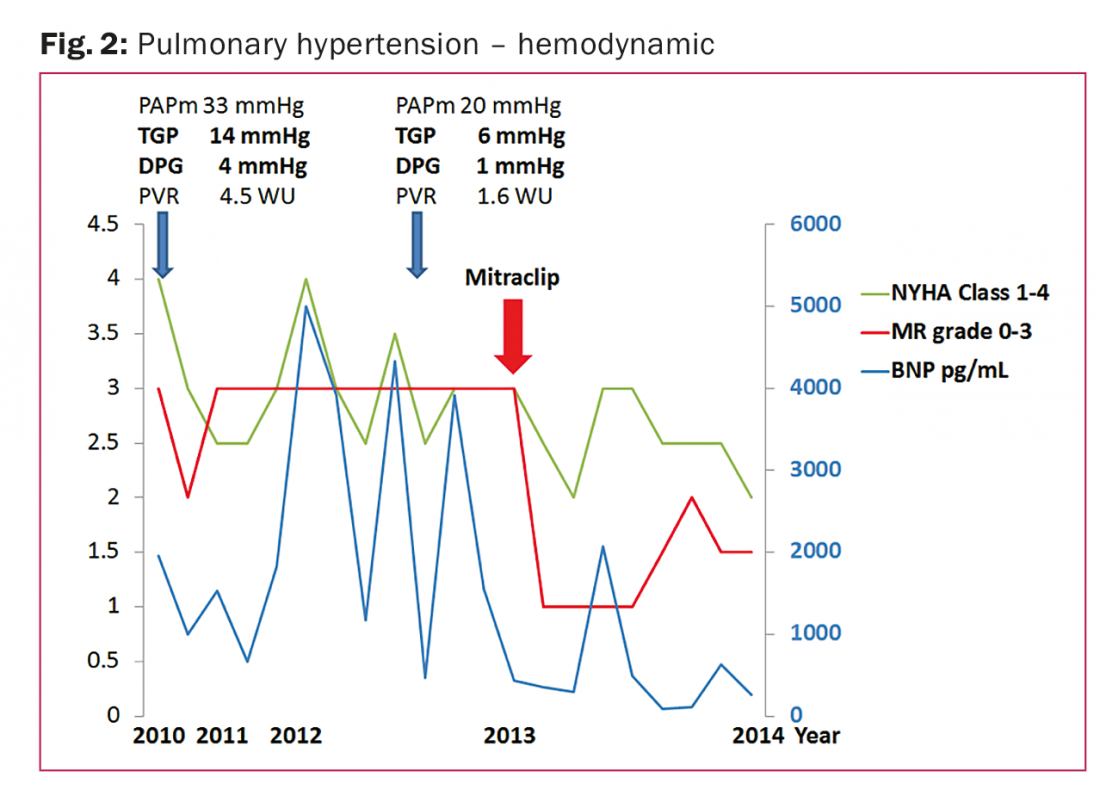
In 2013 a percutaneous edge-to-edge repair using the Mitraclip was successfully performed reducing immediately the mitral regurgitation to light grade. In the following year, no further hospitalizations due to LH decompensation occurred. The patient is clinically stable in NYHA class II, with low BNP levels and light mitral regurgitation.
Management of mitral regurgitation
Echocardiography is the principal examination for mitral regurgitation evaluation and must include a careful assessment of the valve anatomy, the mitral regurgitation severity, its mechanisms (i.e. functional vs. degenerative mitral regurgitation) and addresses the question of valve repairability. The consequences of mitral regurgitation are assessed by measuring left atrium diameter, left ventricular diameter, LVEF, and systolic pulmonary arterial pressure. Current ESC guidelines for diagnosis and therapy of chronic heart failure highlight the importance of re-evaluation of the mitral regurgitation first after several months of stable and maximal tolerated pharmacological therapy [10]. The re-evaluation should always be performed in a cardiac compensated state (optimal volume status) of the patient.
If the mitral regurgitation is still moderate to severe, particularly in the management of high-risk patients, the treatment options (surgical or transcatheter valve repair) should be evaluated in a heart team including cardiologists, cardiac surgeons and imaging specialists [9]. The evaluation should include risk stratification according to symptoms (related to valvular disease), concomitant atrial fibrillation, age, relevant co-morbidities, left ventricular function, PH, need for concomitant surgical intervention (i.e. revascularization), and the suitability of the valve repair which are the most important predictors of post-operative outcome [10]. Operative mortality can be estimated by various scoring systems i.e. STS or EuroSCORE II, including in particular indices aimed at assessing functional and cognitive capacities and frailty in the elderly. The final decision for the optimal treatment option should be made with the patient and family.
Mitraclip therapy
Mitraclip therapy has been successfully used to treat either functional or degenerative mitral regurgitation. The Mitraclip has been evaluated in the multicenter randomized controlled trial EVEREST, that only enrolled operable patients [11]. The majority of patients included into EVEREST had degenerative, but every forth patient had functional mitral regurgitation. In this context, the results from ACCESS-EU, a prospective, multicenter, non-randomized trial in Europe, are of importance, mainly including high-surgical-risk patients (NYHA III–IV and LVEF ≤40% in 85%; EuroSCORE: 23±18,3), primarily due to functional etiology (n=393/510) [12]. Thirty-day mortality rate was 3,4% and the stroke rate 0,7%, with no cases of intra-procedural deaths or clip embolization.
Summary
In summary, PH is an important sign of advanced LHD with worse outcome. The main therapeutic approach should be directed to the origin of the LHD after a careful evaluation. In highly selected cases, therapy approved for PAH, i.e. PDE5i, might be indicated as a bridge to heart transplantation and after left ventricular assist device in case of severe impaired right ventricular function. Since there is still lacking evidence of efficacy from large-scale, long-term placebo-controlled trials, the use of PAH drugs for other forms of PH outside expert centers is discouraged.
Reference list:
- Vachiery JL, et al.: Pulmonary hypertension due to left heart diseases. J Am Coll Cardiol 2013; 62(25 Suppl): D100–108.
- Galie N, et al.: Guidelines for the diagnosis and treatment of pulmonary hypertension. The Task Force for the Diagnosis and Treatment of Pulmonary Hypertension of the European Society of Cardiology (ESC) and the European Respiratory Society (ERS). Eur Heart J 2009; 30(20): 2493–2537.
- Galie N, et al.: 2015 ESC/ERS Guidelines for the diagnosis and treatment of pulmonary hypertension. The Joint Task Force for the Diagnosis and Treatment of Pulmonary Hypertension of the European Society of Cardiology (ESC) and the European Respiratory Society (ERS). Eur Heart J 2016; 37(1): 67–119.
- Ghio S, et al.: Independent and additive prognostic value of right ventricular systolic function and pulmonary artery pressure in patients with chronic heart failure. J Am Coll Cardiol 2001; 37(1): 183–188.
- Lewis GD, et al.: Sildenafil improves exercise capacity and quality of life in patients with systolic heart failure and secondary pulmonary hypertension. Circulation 2007; 116(14): 1555–1562.
- Shan X, et al.: Differential expression of PDE5 in failing and nonfailing human myocardium. Circ Heart Fail 2012; 5(1): 79–86.
- Mehra MR, et al.: Listing criteria for heart transplantation: International Society for Heart and Lung Transplantation guidelines for the care of cardiac transplant candidates–2006. J Heart Lung Transplant 2006; 25(9): 1024–1042.
- Feldman D, et al.: The 2013 International Society for Heart and Lung Transplantation Guidelines for mechanical circulatory support. Executive summary. J Heart Lung Transplant 2013; 32(2): 157–187.
- Vahanian A, et al.: Guidelines on the management of valvular heart disease (version 2012). The Joint Task Force on the Management of Valvular Heart Disease of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS). Eur J Cardiothorac Surg 2012; 42(4): S1–44.
- McMurray JJ, et al.: ESC guidelines for the diagnosis and treatment of acute and chronic heart failure 2012. The Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2012 of the European Society of Cardiology. Eur J Heart Fail 2012; 14(8): 803–869.
- Feldman T, et al.: Percutaneous mitral repair with the MitraClip system. Safety and midterm durability in the initial EVEREST (Endovascular Valve Edge-to-Edge REpair Study) cohort. J Am Coll Cardiol 2009; 54(8): 686–694.
- Maisano F, et al.: Percutaneous mitral valve interventions in the real world. Early and 1-year results from the ACCESS-EU, a prospective, multicenter, nonrandomized post-approval study of the MitraClip therapy in Europe. J Am Coll Cardiol 2013; 62(12): 1052–1061.
CARDIOVASC 2016; 15(2): 11–15