The most common causes of chronic kidney disease (CKD) include diabetes and hypertension. Regular screening is recommended if there is an increased risk of CKD. In addition to the eGFR, albuminuria should also be determined. To counteract the occurrence and progression of CKD as part of a multimodal treatment concept, innovative active substances such as SGLT-i and finerenone are now available in addition to RAAS inhibition.
In Switzerland and Germany, one in ten adults is affected by chronic kidney disease ( CKD), although there is a high number of unreported cases [1,2,9]. Chronic kidney damage has various possible causes and can result in a variety of cardiovascular changes. CKD accelerates the development and progression of arteriosclerosis and atherosclerosis, reported Dr. Frederic Bauer, Chief Physician at the Clinic for Nephrology and Dialysis at the Elisabeth Hospital in Essen (Germany). While atherosclerosis describes a disease of the intima, arteriosclerosis of the Mönckeberg type primarily affects the media. “Chronic renal insufficiency is an important cardiovascular risk factor in its own right,” emphasized the speaker [1,3]. As a result, many CKD patients die due to cardiovascular events. “We want to reduce the significantly increased cardiovascular risk by making all the necessary adjustments and the prerequisite for this is that we make the diagnosis at an early stage,” says the speaker. As CKD is often asymptomatic, it is significantly underdiagnosed. People at high risk should therefore be screened [2].
Increased albuminuria is a risk factor even with normal eGFR
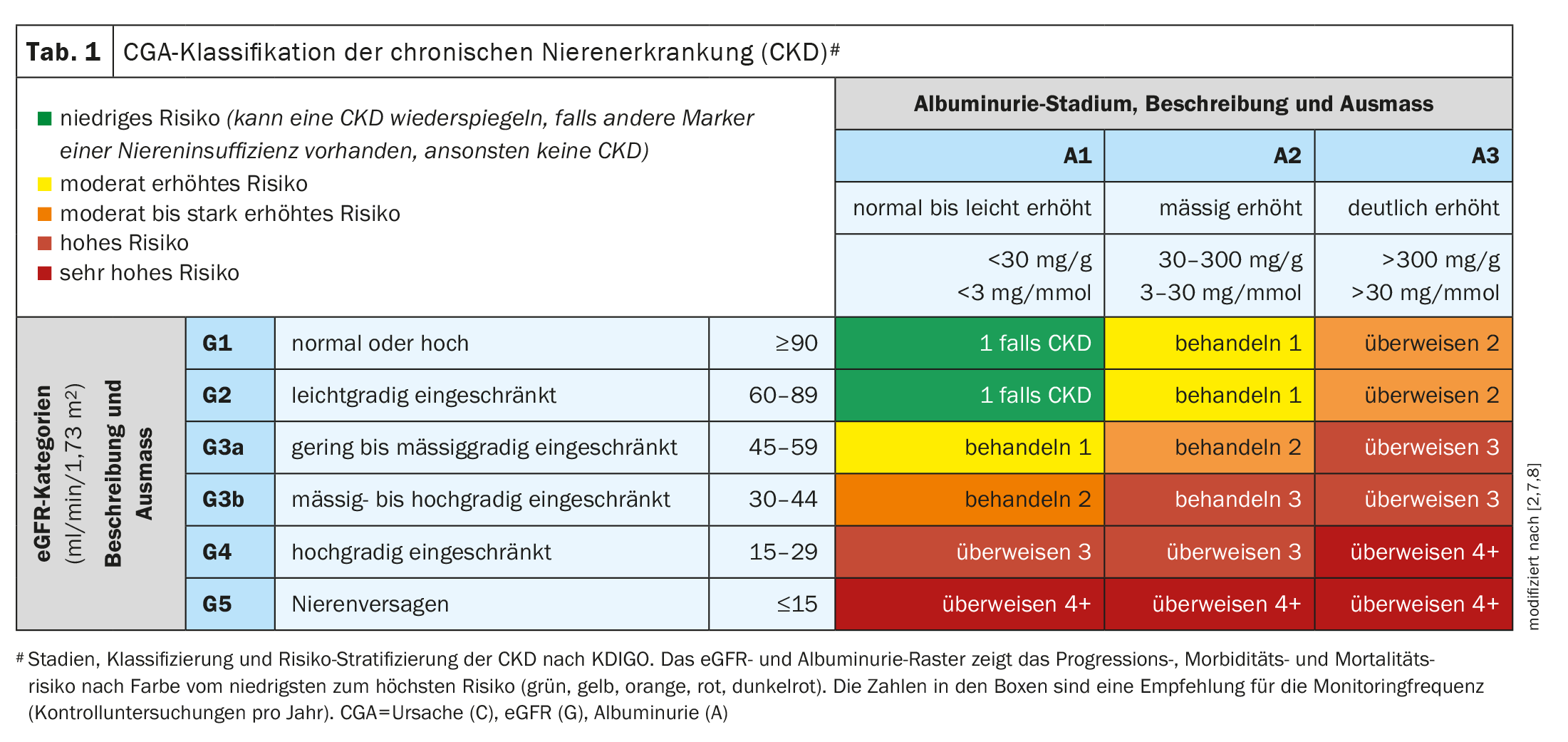
According to KDIGO (Kidney Disease: Improving Global Outcomes) , CKD is defined by a structural or functional disorder of the kidney with implications that are relevant to health that has persisted for >3 months. CKD is classified according to the “CGA” scheme: cause (C), glomerular filtration rate (GFR, G) and albuminuria (A). The CGA staging of CKD according to KDIGO is shown in Table 1 . Dr. Bauer emphasized that both a reduced eGFR and albuminuria (UACR ≥30 mg/g) are relevant for chronic renal insufficiency [1]. “Both are important and independent predictors of overall mortality,” emphasized the speaker. For albuminuria (albumin-creatinine ratio in urine, UACR), 24-hour urine collection is not required, but spontaneous urine is sufficient [1].
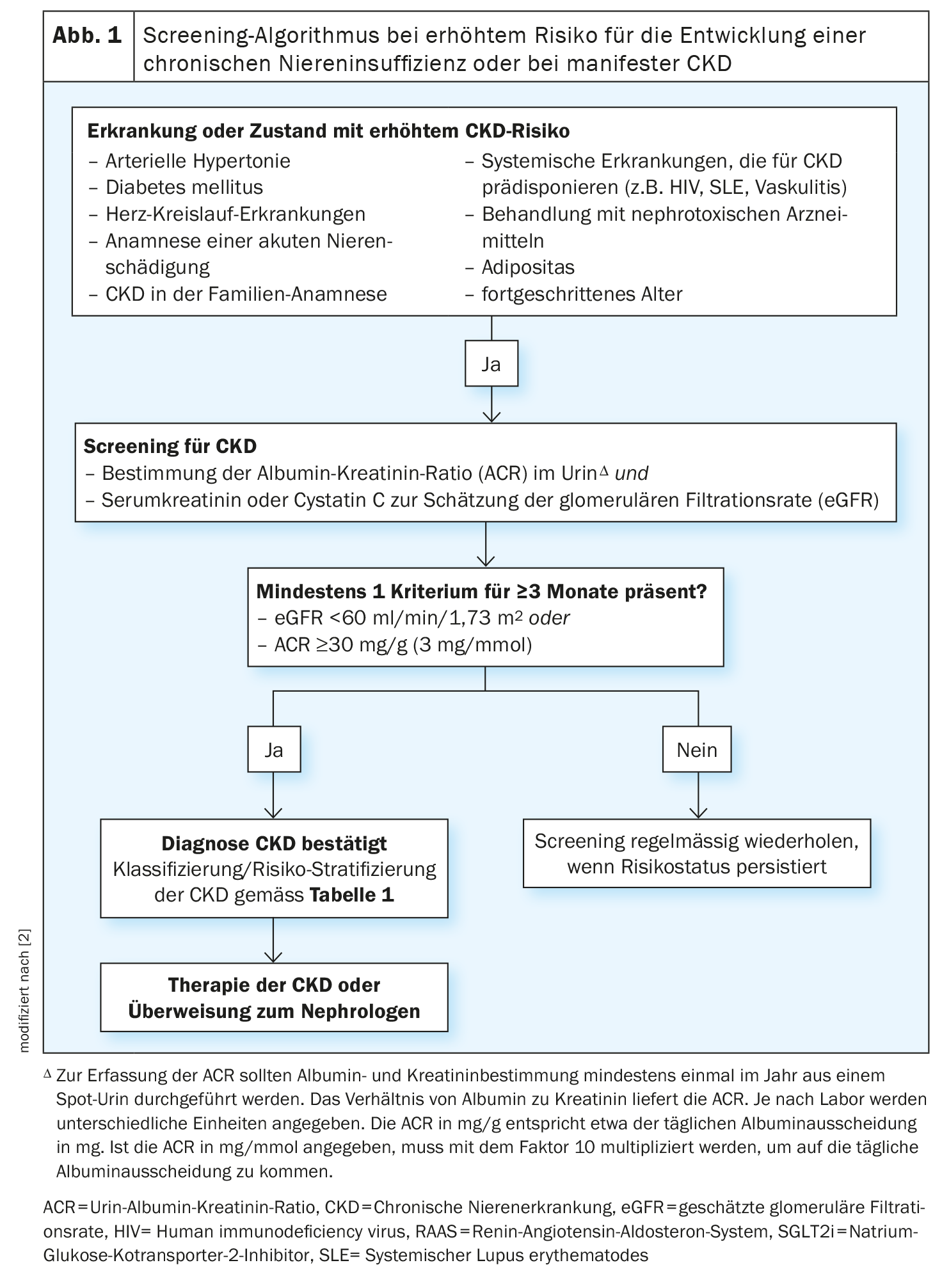
Cardiovascular risks, hospitalization rates and mortality increase sharply from an eGFR <60 ml/min/1.73m2, according to Dr. Alexander Beck, specialist in internal medicine and cardiology in Essen (Germany) [1]. The Swiss Society of Nephrology’s guidelines on screening and identification of CKD therefore recommend that patients with arterial hypertension, diabetes mellitus and cardiovascular disease should be tested at least once a year for the presence of CKD (eGFR and UACR) [2]. Dr. Beck advised that patients with a positive family history of CKD or a documented history of significant deterioration in kidney function should also be screened from time to time [1]. “If we recognize these patients early and treat them early, we not only reduce the risk of dialysis, but also the cardiovascular risk,” emphasized the speaker [1]. CKD stages 3-4 account for almost half of all CKD patients. According to Dr. Beck, this offers great potential for prevention and the avoidance of cardiovascular events [1]. There are individual fluctuations in the eGFR, while the UACR is actually the more stable parameter. If there are any abnormalities in the CKD screening, structural changes in the kidney must be ruled out by ultrasound. Patients at high and very high risk should be referred to a nephrologist (Fig. 1) [1].
Progression inhibition with RAAS inhibition, SGLT-2-i and finerenone
In the second part of the symposium, Dr. Bauer explained a multimodal approach to slowing the progression of renal insufficiency [1]. With regard to lifestyle modification, the recommendations for patients with high proteinuria and low eGFR largely coincide with those for hypertensive and diabetic patients: weight control, blood pressure control, exercise, salt reduction, smoking cessation [1]. Nephrotoxic drugs (e.g. non-steroidal anti-inflammatory drugs, NSAIDs) should also be avoided if possible. In addition to the proven treatment of high blood pressure and reduction of albuminuria with renin-angiotensin system (RAAS) inhibitors such as angiotensin-converting enzyme (ACE) inhibitors or angiotensin II receptor blockers (ARBs), there are now two other progression-inhibiting substance classes, SGLT-2 inhibitors and finerenone. “RAAS inhibition is the classic nephroprotective therapy, especially for patients with albuminuria,” said the speaker [1]. The pressure in the glomerulus is reduced, thus reducing hyperfiltration. Almost all CKD patients have glomerular hyperfiltration, which damages the filter units of the kidney in the long term. Patients should be informed that creatinine levels may deteriorate slightly during RAAS inhibition. Maximum RAAS inhibition can reduce mortality and, if necessary, a nephrologist should be consulted, says Dr. Bauer.
The fact that SGLT-2 inhibition with dapagliflozin in addition to RAAS blockade leads to a significant reduction in renal endpoints in both CKD patients with and without diabetes was impressively demonstrated in the DAPA-CKD study, among others [4]. In addition to Forxiga®, fixed combinations of dapagliflozin with metformin and/or saxagliptin are also approved for diabetics in Switzerland. In addition to dapagliflozin, empagliflozin is now also approved, which demonstrated nephroprotective effects in the EMPA Kidney Study [5]. In addition to Jardiance®, fixed combinations with metformin and or linagliptin are also available.
SGLT-2 is a carrier protein that reabsorbs about 90% of the filtered glucose in the proximal tubule of the kidney. If this is reduced by the SGLT-2 inhibitors, the sodium concentration at the macula densa increases and the tubulo-glomerular feedback leads to a constriction of the afferent arterioles at the glomerulus and thus also to a reduction in glomerular hyperfiltration. In acute disease, SGLT-2 inhibitors should be discontinued due to a slightly increased risk of ketoacidosis.
Finerenone (Kerendia®) is also available for patients with CKD and diabetes. Finerenone is an active substance from the group of aldosterone antagonists. The effects are based on the selective antagonism of mineral corticoid receptors. Finerenone demonstrated nephroprotective and cardioprotective effects in diabetics in the FIDELIO-CKD and FIGARO-CKD studies [6]. Studies are still ongoing for CKD patients without diabetes [1].
Congress: FomF General Medicine Refresher
Literature:
- “CKD – Screening, early diagnosis and modern therapy – nephro- cardioprotection in primary care practice”, Symposium, AstraZeneca GmbH, FOMF General Medicine Refresher Cologne, January 17-20, 2024.
- Swiss Society of Nephrology, Guidelines on screening and identification of chronic renal insufficiency for general practitioners and internists, www.swissnephrology.ch/wp/wp-content/
uploads/2023/01/161121_SGN_Pocketguide_CKD_Web_A4_e_WZ.pdf, (last accessed 26.01.2024) - Gansevoort RT, et al: Chronic kidney disease and cardiovascular risk: epidemiology, mechanisms, and prevention. Lancet 2013; 382: 339-352.
- Heerspink HJL, et al; DAPA-CKD Trial Committees and Investigators. Dapagliflozin in Patients with Chronic Kidney Disease. NEJM 2020; 383(15): 1436-1446.
- The EMPA-KIDNEY Collaborative Group; Herrington WG, et al: Empagliflozin in Patients with Chronic Kidney Disease. NEJM 2023; 388(2): 117-127.
- Agarwal R, et al: FIDELIO-DKD and FIGARO-DKD Investigators. Investigating new treatment opportunities for patients with chronic kidney disease in type 2 diabetes: the role of finerenone. Nephrol Dial Transplant 2020.
- Kidney Disease: Improving Global Outcomes (KDIGO) CKD Work Group. Kidney Int 2013; 3(Suppl): 1–150.
- American Diabetes Association. Diabetes Care 2021 Jan; 44: 10.2337/dc21-S005
- Ogna VF, et al: Prevalence and determinants of chronic kidney disease in the Swiss population. Swiss Med Wkl 2016;146: w14313.
HAUSARZT PRAXIS 2024; 19(2): 26-27 (published on 18.2.24, ahead of print)