Increasingly, AID (Automated Insulin Delivery) systems are being used for automated or semi-automated insulin dosing in the treatment of type 1 diabetes. Through pump and sensor technology coupled with control algorithms, AID systems can help achieve stable, normoglycemic metabolic control, reduce the risk of acute severe metabolic derailments, and significantly improve glucose management in type 1 diabetes.
A good example of a partially automated AID system is provided by the “KidsApp” research project for children up to the age of seven. At the same time, it fills a treatment gap. Automated pumps that regulate insulin delivery in type 1 diabetes have been available primarily for older children and adolescents. Several European study centers, including the University of Cambridge, the Medical Universities of Innsbruck, Graz and Vienna (A) have collaborated on this project. The closed-loop (AID) system, which was tested in 74 children between the ages of 1 and 7, works through CamAPS FX, an app developed at the University of Cambridge, connected to a glucose sensor for continuous glucose measurement and an insulin pump like an artificial pancreas. Based on recorded and predicted glucose values, the amount of insulin delivered is automatically adjusted. Young children with type 1 diabetes often have pronounced blood glucose fluctuations, putting them at high risk for dangerously low blood glucose levels (hypoglycemia) that can lead to unconsciousness and seizures, as well as dangerously high blood glucose levels (hyperglycemia) that increase the risk for acute severe metabolic derailments and for the development of diabetic ketoacidosis. The children’s blood sugar must be measured several times around the clock. To ensure that glucose and insulin requirements are adjusted safely and without gaps, insulin is administered to the children at mealtimes by caregivers. During the rest of the time, the algorithm ensures that the programmed glucose target value (usually 100 mg/dl) is reached and remains stable. This will provide significant relief for families.
To assess the safety and efficacy of the hybrid AID system, it was compared with sensor-assisted insulin pump therapy in a trial. Participating children initially used the app-controlled system for 16 weeks and then used conventional sensor-assisted insulin pump therapy for 16 weeks. Analysis of the data showed that the time in the glucose target range (70-180 mg/dl) could be significantly increased with the partially automated AID system. The children’s glucose levels were in the target range for an additional 125 minutes per day. This resulted in a 0.7 percent reduction in HbA1c in young patients who were already well controlled. In addition, the time with elevated blood glucose levels was reduced by 9 percentage points. The improvement in glucose control occurred without an increase in hypoglycemia.
AID systems on their way into standard therapy
It is estimated that 50% of patients with type 1 diabetes will be using an AID system in just under 9 years, and as many as 90% in about 17 years, explained Dr. Jens Kröger, a diabetologist from Hamburg and chairman of the board of diabetesDE – Deutsche Diabeteshilfe. Even very young children under the age of seven can be helped by systems such as CamAPS FX. However, the evidence is higher in adults and children and adolescents older than seven years.
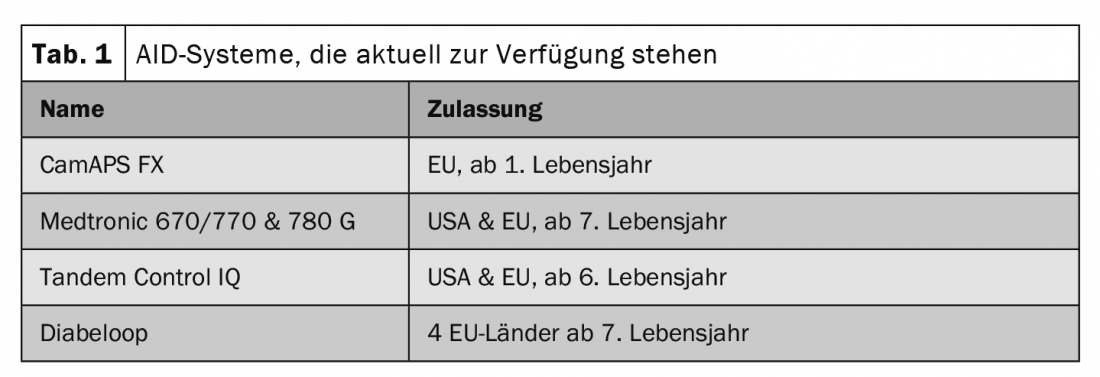
In principle, AID systems should be offered to all patients with type 1 diabetes, but especially to people with suboptimal glucose control, problematic hypoglycemia, and/or significant glucose variability and reduced quality of life (Table 1). The systems were also suitable for people with moderate to high for severe hypoglycemia and hypoglycemic unawareness (Table 2).
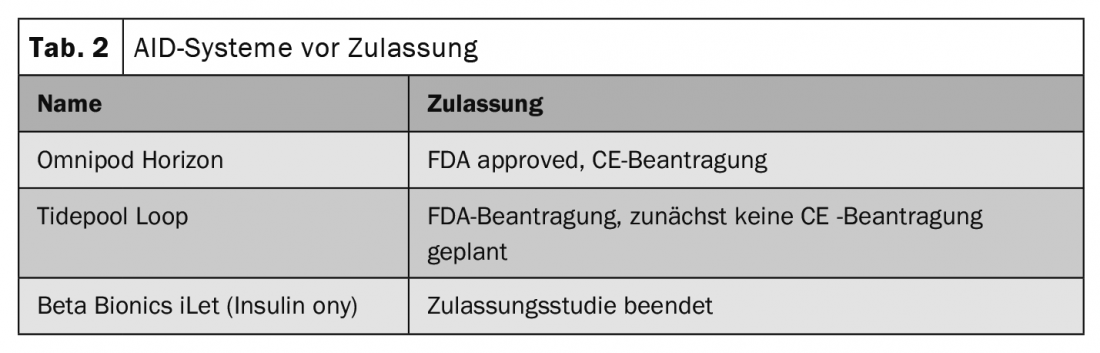
The individual systems differ in terms of their useful life per sensor and the type of algorithm. Not all of them have a correction bolus output. AID systems may favorably influence prognosis because they work in most people with type 1 diabetes, although this does not yet predict efficacy. Furthermore, there are no clear differences between subjects with optimal/suboptimal glycemic control in terms of effect. However, a shorter duration of diabetes and a higher level of education are advantageous for the prognosis. In addition, success depends on individualized configuration and also on patient care.
AID systems not without training
On the part of health care providers, Kroeger said, any social and/or racial biases that may exist should be recognized and overcome with regard to individual, family, psychological characteristics necessary for effective use of Aid systems. This is the only way to ensure fair and equitable access to AID systems, he said. Patients require pre-training in general diabetes self-management, basic knowledge of insulin pump and rtCGM therapy, individualized technical introduction to the system, and follow-up care. This is important, among other reasons, because difficulties in dealing with the AID system are often behind treatment discontinuations. These include, to name a few, problems calibrating the sensor, too many alarms, the system interfering at night, too much time spent. The perceptions regarding the success of the therapy are also different. The predicate “successful” could refer to a TIR >70%, HbA1c value, avoidance of severe hypoglycemic events, or even positive psychosocial functioning. According to Kröger, success here should not be defined by clinical parameters alone.
Congress: DDG 2022
CARDIOVASC 2022; 21(3): 28-29