Coronary artery bypass grafting (CABG) with heart-lung machine is the gold standard of myocardial revascularization. The results of off-pump surgery and percutaneous intervention (PCI) should be measured against this. Bypass openness rates after CABG depend on multiple factors. The algorithm for graft selection (internal thoracic artery, radial artery, or venous graft) is becoming more complex with increasing clinical evidence. The modern concept of coronary surgery includes minimized extracorporeal circulation (mini-ECC or MECC). Modifications to the classic CABG surgery improve clinical outcomes (“improving the gold standard”). Modern coronary surgery can be performed in the elective setting with very low mortality (<1%).
In stable coronary artery disease (CAD), myocardial revascularization by aortocoronary artery bypass grafting (CABG) is the gold standard of therapy. A recently published large meta-analysis summarizing 100 randomized trials involving nearly 100 000 patients clearly demonstrates that CABG significantly reduces the risk of death, myocardial infarction, and repeat revascularization compared with drug treatment. In contrast, evidence for a survival benefit after percutaneous intervention (PCI) is shown only when the newer generation of drug-eluting stents is used [1].
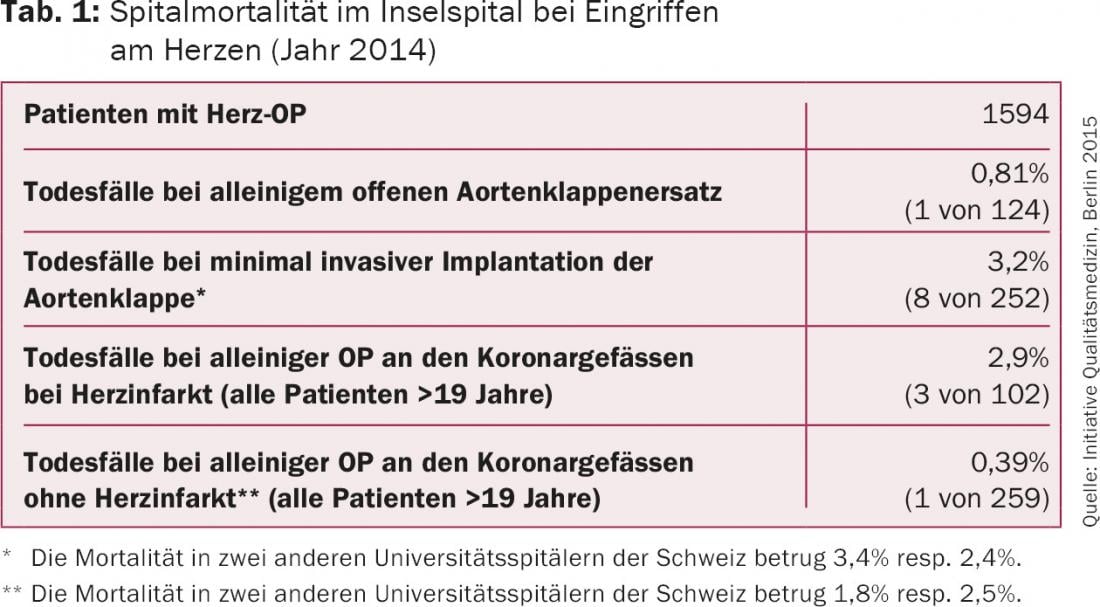
The procedure of PCI became much more effective in the past decades, first with the introduction of stents and then with drug-eluting stents, improved (peri-)procedural technique, and intensified antiplatelet therapy. Comparative studies between treatment options (CABG vs. PCI) now make an evidence-based choice possible, which is differentially reflected in the current guidelines for myocardial revascularization (Table 1) [2]. An overview of this has already been presented in two articles in the last issue of this journal [3,4].
PCI measures up to the gold standard of CABG. The number of affected vessels and the complexity of coronary stenoses important criteria for the therapeutic decision. Here, the more complex the CHD, the more CABG offers advantages over PCI.
The SYNTAX study
The SYNTAX trial was seminal in this regard, as it differentiated advantages and disadvantages of treatment options in patients with coronary three-vessel disease and/or main stem stenosis. In the 5-year analysis, the combined primary endpoint (all-cause mortality, myocardial infarction, coronary re-intervention, and stroke) was significantly more frequently achieved after PCI than after CABG (37.3% vs. 26.9%; p<0.0001) [5]. When considered individually, cardiac mortality at five years was significantly higher after PCI (9.0% vs. 5.3%; p=0.003). The rate of myocardial infarction was significantly higher after PCI (9.7%) than after CABG (3.8%; p<0.001), and coronary reinterventions were needed about twice as often after PCI than after CABG (25.9% vs. 13.7%; p<0.001). After one year there was a significant difference in stroke rate in favor of PCI (0.6% vs. 2.2%; p=0.003) – a complication that must be prevented by cardiac surgery with all efforts! – -, although this difference in cumulative numbers was no longer significant after five years (2.4% vs. 3.7%; p=0.09).
To more accurately describe the patient cohort, which included more than 1800 patients in the SYNTAX study, a coronary stenosis complexity score was developed, called the SYNTAX score. Patients with intermediate and high SYNTAX scores showed clear advantages of CABG over PCI. The difference in patients with low SYNTAX scores and less complex stenoses was not significant, making PCI an acceptable treatment alternative in this patient group. In conclusion, after five years of SYNTAX trial, in toto the goal of non-inferiority of PCI over CABG was not achieved [5].
Looking at the patient groups of the SYNTAX study as well as other large comparative studies such as FREEDOM, BEST, PRECOMBAT, etc. (key statements of these studies compiled in [3]), which showed advantages of CABG over PCI in the patient group with multivessel coronary disease, it is striking that these results were achieved although some aspects of modern coronary bypass surgery were not consistently applied (e.g., only limited number of arterial revascularizations). Coronary surgery is evolving, and the proven good results are constantly being improved (as with PCI) by modification. Because these changes are less well known, some principles of a modern concept of coronary surgery will be described here.
Choice of graft material
Conventionally, CABG uses the left internal thoracic artery (IMA) as the graft material, which is the ideal conduit for bypass to the anterior interventricular ramus (RIVA). In addition, segments of the great saphenous vein are used to perform complete revascularization of other affected coronary vessels. IMA bypass to the RIVA is clearly superior to other arterial and venous bypass grafts. In comparison, larger studies for venous grafts show significantly inferior open rates of about 75% after ten years, whereas IMA bypasses have open rates of >90% for the same observation period. The survival advantage of CABG over drug treatment and also PCI is particularly associated with the high openness rate of the IMA graft on the RIVA.
The use of both internal mammary arteries (BIMA) has shown further treatment benefit in several studies [6]. It should be noted, however, that in the presence of additional risk factors (e.g., obesity, diabetes mellitus, pulmonary disease, immunosuppression), the incidence of sternal wound complications due to microcirculatory disturbances may be increased. However, with adequate patient selection and adapted preparation technique (so-called skeletonized technique), the number of sternal wound complications should be only insignificantly increased.
The radial artery (RA) of the nondominant hand is used as an alternative arterial graft for bypass grafting in up to 50% of patients. A prerequisite for harvesting is a performed Allen test demonstrating an open palmar arch and adequate supply to the hand via the ulnar artery alone. RA as a bypass graft has been shown in several studies to be superior to venous bypasses with higher openness rates and also a survival benefit. The RA is a muscular-type artery and may be prone to vasospasm. Therefore, drug therapy with nitrates or calcium antagonists is often performed after the use of an RA. However, morphological studies indicate that this is only necessary for the initial period (weeks) after CABG, as remodeling of the vessel wall toward elastic artery type occurs after integration into the coronary circulation [6].
Today, although pure arterial revascularization is generally recommended, the algorithms for graft selection are infinitely more complex than they were 10-15 years ago due to increasing evidence regarding other factors that influence the bypass graft openness rate (Fig. 1). It has been clearly demonstrated that bypass opening rates also depend substantially on the characteristics of the coronary target vessel, with the upstream degree of stenosis, the size and downstream nature of the target vessel, and the corresponding myocardial territory being important factors. Of course, the surgical exactness of the anastomotic passage between the bypass graft and the coronary graft should not go unmentioned either. With only borderline stenosis of the coronary artery, the openness of a bypass is more limited by competitive flow in RA than when a vein graft is used – again, depending on the myocardial supply territory (ie, whether the bypass is to the RIVA, the ramus circumflexus, or the right coronary artery). For IMA-RIVA bypass, recent analysis of more than 1500 control coronarographies in a larger study (PREVENT) shows that graft failure (stenosis ≥75% or occlusion) is associated with only moderate-grade RIVA stenosis and also with placement of a vein graft on a side branch (diagonal branch) of the RIVA [7].
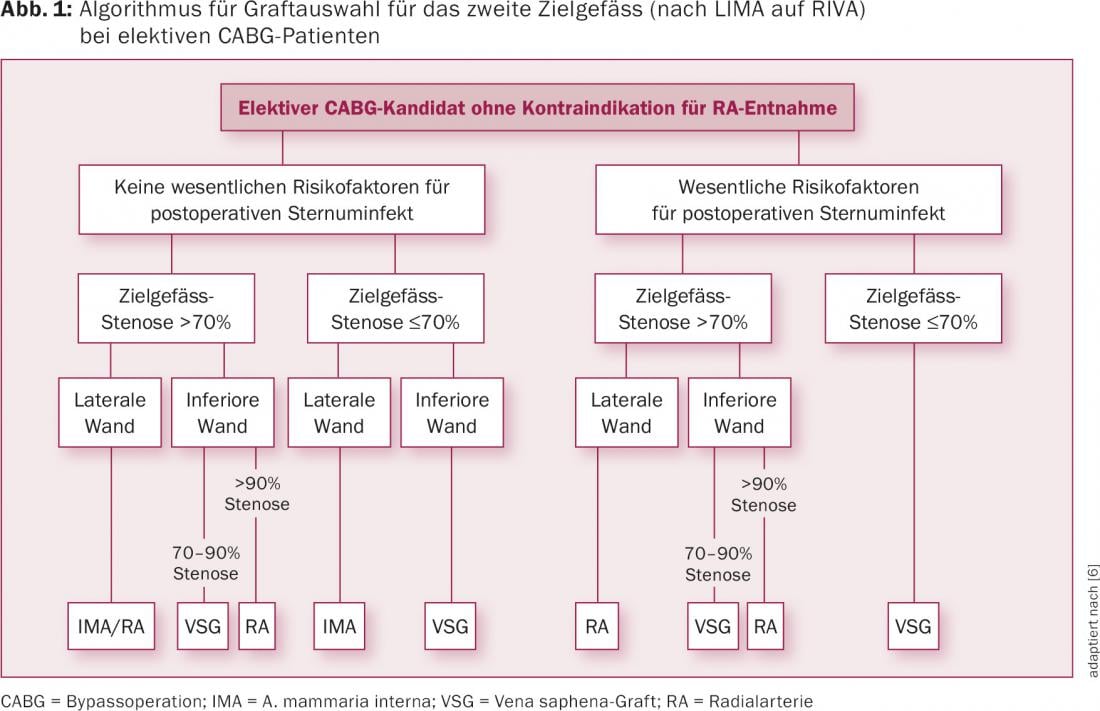
Today, the choice of graft material as well as the principle decision as to which coronary vessels should all be treated are clearly individualized and best made in a team meeting for surgical planning. The rough principles “IMA on RIVA, the rest with venous grafts” as well as “connect everything” no longer correspond to a differentiated modern concept of coronary surgery. It should also be noted that with the significantly improved results of PCI, combined therapy procedures (so-called hybrid procedures) are increasingly being used. This is a very helpful procedure, e.g. in case of re-CABG, where quite often the decision is made to revascularize the more accessible main vessels (RIVA and RCA) by CABG and the RCX with PCI.
Off-pump?
CABG is still performed in the majority of cases worldwide with use of the heart-lung machine (HLM) in combination with immobilization (cardioplegia) of the heart. The advantages of an immobilized heart and blood-free surgical field with the possibility of controlled and safe anastomosis between bypass graft and coronary vessel are bought with side effects of HLM. These include, for example, foreign-surface-associated systemic inflammatory reactions, hemodilution at the HLM, and bleeding complications due to the need for anticoagulation during surgical procedures-factors that may all contribute relevantly to patient morbidity and mortality.
In off-pump procedures, a distinction is usually made between MIDCAB (“minimally invasive direct coronary artery bypass”) for revascularization of the RIVA alone via access through an anterior mini-thoracotomy and OPCAB (“off-pump coronary artery bypass”) for revascularization in coronary multivessel disease, where access is via median sternotomy as in conventional CABG with HLM. Unfortunately, the hoped-for clinical benefits with the introduction of off-pump procedures could not be confirmed. Current data indicate that even in centers with expertise in this surgical option, no significant advantages over conventional CABG are found in terms of myocardial infarction or mortality [8,9]. Both procedures achieve good clinical results, although the choice of surgical revascularization method is individual and depends on patient factors (comorbidities, life expectancy) and the experience of the surgeon or the patient. of the surgical team should be made dependent [9]. With this in mind, it makes sense to further optimize the gold standard of therapy (CABG with HLM).
Mini-ECC
With the modification of conventional HLM to the so-called minimized extracorporeal circulation (mini-ECC or MECC), negative effects of HLM can be reduced. Due to a closed bypass system and the elimination of the venous reservoir, as well as the integration of an infrared-triggered suction system or in combination with a CellSaver, the MECC has a significantly lower foreign surface area and priming volume (600 instead of 1500 ml) compared to conventional HLM, with a correspondingly higher intraoperative hematocrit (Figs. 2 and 3). Contact or complement activation is thus lower and the aseptic inflammatory reaction, which in individual cases leads excessively to postcardiotomy syndrome, is measurably reduced. The centrifugal pump drive and the modified suction device result in less damage to the blood components overall. This setting is supplemented by a newly developed low-volume cardioplegia solution (Cardioplexol) [10,11].

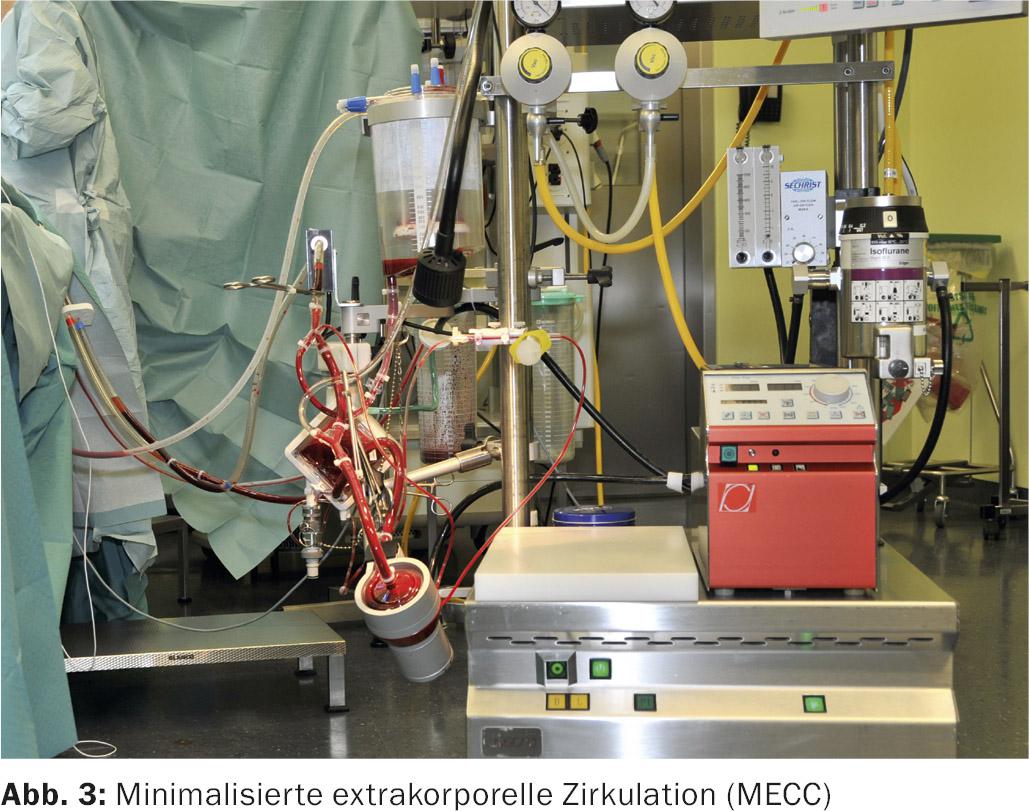
With this setting, which we have been using at Inselspital for more than twelve years and now also at Hirslanden Klinik Aarau, we have already performed more than 4000 CABG. The mortality rate for elective surgery can thus be reduced to well below 1%. In the published quality figures of the Federal Office of Public Health as well as the IQM (Initiative Quality Medicine), the mortality in CABG without prior myocardial infarction in Inselspital is 0.4% in 2014. In contrast, the mortality rate is on average 1.8% in relation to all participating hospitals in the DACH area (Germany, Austria and Switzerland) [12].
Another modification to be considered in a modern concept of coronary surgery is the biocompatible coated HLM circuits (heparin coatings and others). In terms of intraoperative quality improvement, the routine measurement of bypass flows should also be mentioned [13]. In addition, the standardized and optimized treatment concepts in the perioperative setting by colleagues in anesthesiology and intensive care medicine contribute significantly to improving the success of treatment after CABG.
Literature:
- Windecker S, et al: Revascularisation versus medical treatment in patients with stable coronary artery disease: network meta-analysis. BMJ 2014; 348: g3859.
- Windecker S, et al: 2014 ESC/EACTS Guidelines on myocardial revascularization: The Task Force on Myocardial Revascularization of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS). Eur Heart J 2014; 35(37): 2541-2619.
- Aries JD, Bauersachs J: PCI after the SYNTAX study. Reason to adjust indications? Cardiovasc 2015; 14(6): 4-8.
- Wichmann C, Eckstein F: Stable coronary artery disease. What are the indications for percutaneous intervention? Cardiovasc 2015; 14(6): 9-12.
- Mohr FW, et al: Coronary artery bypass graft surgery versus percutaneous coronary intervention in patients with three-vessel disease and left main coronary disease: 5-year follow-up of the randomised, clinical SYNTAX trial. Lancet 2013; 381(9867): 629-638.
- Gaudino M, et al: The Choice of Conduits in Coronary Artery Bypass Surgery. J Am Coll Cardiol 2015; 66(15): 1729-1737.
- Harskamp RE, et al: Frequency and Predictors of Internal Mammary Artery Graft Failure and Subsequent Clinical Outcomes: Insights From the PREVENT IV Trial. Circulation 2016; 133: 131-136.
- Diegeler A, et al: Off-pump versus on-pump coronary-artery bypass grafting in elderly patients. N Engl J Med 2013; 368: 1189-1198.
- Deppe AC, et al: Current evidence of coronary artery bypass grafting off-pump versus on-pump: a systematic review with meta-analysis of over 16 900 patients investigated in randomized controlled trials. Eur J Cardiothorac Surg 2015 Aug 13 [Epub ahead of print].
- Jenni H, et al: Autotransfusion system or integrated automatic suction device in minimized extracorporeal circulation: influence on coagulation and inflammatory response. Eur J Cardiothorac Surg 2011; 39: e139-143.
- Immer FF, et al: Minimal extracorporeal circulation is a promising technique for coronary artery bypass grafting. Ann Thorac Surg 2007 Nov; 84(5): 1515-1520.
- IQM: Quality results Inselspital University Hospital Bern. http://www.initiative-qualitaetsmedizin.de/qr/applet/d6b545dfe651a105ca48c5972168bfca33f04e9a/
- Lehnert P, et al: Transit-time flow measurement as a predictor of coronary bypass graft failure at one year angiographic follow-up. J Card Surg 2015; 30: 47-52.
CARDIOVASC 2016; 15(1): 8-12