An Internet search returns approximately 57 million results for the term “burnout.” Much better is the knowledge yield that the participants of the 1st Burnout Symposium in Pfäffikon could take away. What burnout experts and the Institute for Occupational Medicine ifa consider to be state of the art for prophylaxis, therapy and rehabilitation is much more helpful for dealing professionally with “burned out” people than googling umpteen times.
The motto of the first Burnout Conference of the Institute of Occupational Medicine ifa in Baden under the scientific direction of Dr. Claude Sidler was “Burnout, the way back”. The reintegration of patients with mental and psychiatric illnesses is becoming increasingly important; these illnesses have increased 8 times as rapidly in IV discharge statistics as somatic illnesses over the past 25 years. However, the prevalence of mental disorders per se is not increasing, as Dr. Niklas Baer from the IV in Liestal pointed out. Rather, he said, it is an increasing awareness and greater focus on mental health problems, as well as a change in the assessment of work ability, that has contributed to this increase. Counseling and support for those affected should therefore be appropriately coordinated with the employer whenever possible.
Back to the lion’s den
Under labor law, an employee who falls ill is required to seek maximum treatment. But what happens if a burnout patient who has undergone therapy returns to the lion’s den without anything having changed? “The prognosis is lousy without changes in the workplace,” Dr. Sidler pointed out. Reintegration is not easy, but it is worth a try. About 15-20% of those affected by severe burnout return to maximum work afterwards, according to the modest yield so far. From the experts’ point of view, it is therefore too short-sighted to “treat” a stressed employee in the medical practice in such a way that adverse working conditions are endured for a further period of time without eliminating the causes. A key role is played by company physicians with their knowledge of work structures and operating procedures, Dr. Sidler emphasized.
The big question, he said, is whether things are really that bad in the workplace or whether perceived fear is the main problem. Patients who become mentally ill as a result of the work situation are often no longer very productive and disrupt the working atmosphere. Employers have a hard time dealing with people who are mentally unstable. According to one survey, they are more likely to support workers with physical illnesses and somatoform pain than people with personality disorders or depression, Dr. Baer reported. Patients with mental health problems also rank near the bottom of new hires. Top qualities that employees want are reliability and health. Stigmas are not only a problem on the employee side, however; even mentally ill people themselves would hardly give themselves a chance to get a job. “Fears are a general topic on both sides,” Dr. Baer emphasized. “They should definitely be addressed. Good contact with the boss and positive feedback are hugely important.”
In a study on the difficult employee, people who deny mistakes and act moody were rated as most problematic for bosses. According to this research, managers can be categorized into four types: Activists (15%), Zuwarter (24%), Performance Demanders (47%), and those who call for professional help (14%). Reactions in teams were also surveyed: the more anger built up, the more sympathy for the sick colleague decreased and the sooner termination occurred. “There are many reasons to get a doctor involved early on, before compassion drops to zero,” Dr. Baer said. Bosses should respond by showing appreciation, providing clear guidance on expectations, and requiring the troublesome employee to go to the doctor. And earlier than before! The average time to part with a difficult employee is about 2.8 years, a long time of suffering for both parties.
This is how SBB does it
The SBB has already reacted to the burnout problem in the ranks of its 29,000 employees, as personnel manager Markus Jordi reported. “Health has to be a management issue, since absences due to illness have so far cost the company 120 million francs a year,” he said, describing the business side. The basic assumption is that better leadership also means fewer days of absence. At the first sign of a reduction in performance, the primary goal is to restore the ability to work, he said. On the SBB intranet, every employee can find the definition of burnout and the request to contact the medical service for collegial advice if there is any indication that they are affected. Requirement and reward must be right for the individual’s job satisfaction, according to another SBB management rule. This is also important during reintegration, Jordi said.
The consequences of frustration in the workplace can be physical and psychological. Dieter Kissling, M.D., Baden, has been involved in workplace health promotion for many years, founded ifa and advises large companies in Switzerland. For him, burnout is an anxiety disease. “We have to infiltrate bosses with foils,” as far as his experience goes. The first male reflex among managers when an employee is affected is defense: “That has nothing to do with me. If awareness is successfully raised, leadership behavior improves. The demand for constant accessibility and an imbalance between work and leisure time cannot be solved by the individual; here, managers must learn to recognize those at risk and take action. Room for maneuver and decision-making authority are important needs of employees.
Maslach Burnout Inventory
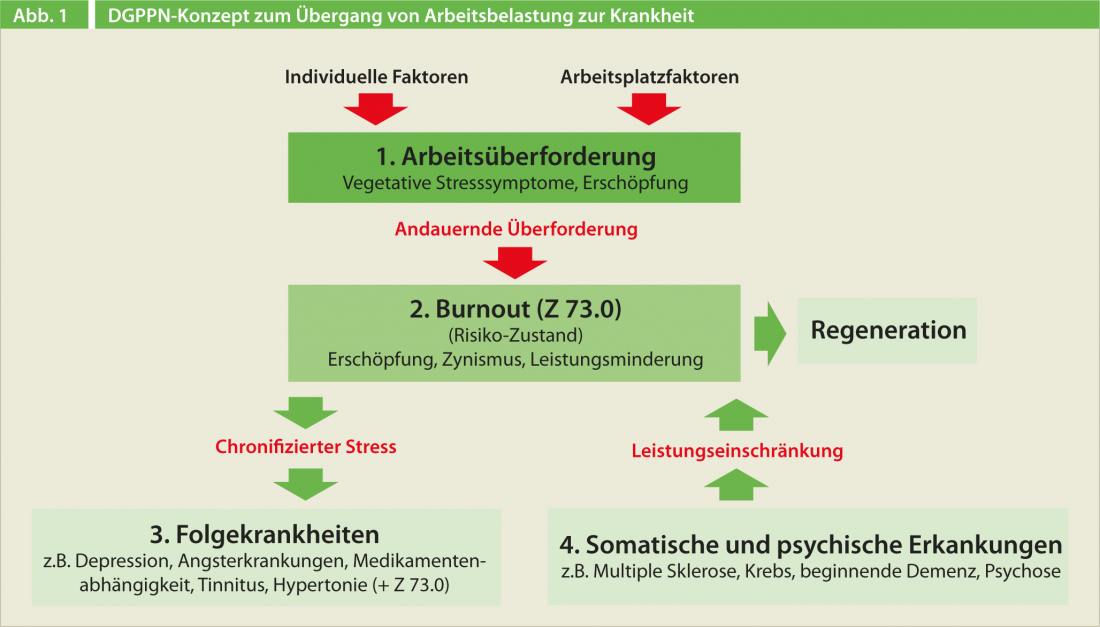
Dr. Beate Schulze from Zurich is a sociologist and psychologist who studies risk and resilience factors for burnout as well as prerequisites for commitment and motivation in a globalized working world. Together with experts, she founded the Swiss Expert Network on Burnout. For them, burnout is more than exhaustion, but not yet depression. The position paper Burnout of the German Society for Psychiatry, Psychotherapy and Neurology (DGPPN) from March 2012 summarizes the problem of coding very well, according to their note(Fig. 1) [1, 2]. An overlap between severe burnout and depression leads to a confusion of terms between the occupational psychology concept of burnout and the medical diagnosis of a depressive episode.
Established occupational psychological tests are suitable for recording the burnout syndrome in clinical practice. The best validated is the Maslach Burnout Inventory (MBI). Burnout develops as a sustained stress response to chronic workloads with three core symptoms:
- Exhaustion refers to the feeling of being both emotionally and physically drained.
- Cynicism describes a detached, indifferent attitude toward work.
- Ineffectiveness describes the feeling of professional failure as well as the loss of confidence in one’s own abilities.
In addition, there are two other criteria:
- Burnout is generally work-related.
- Inappropriate expectations and high emotional demands play an important role.
In a prospective study from Finland, which examined the relationship between burnout and depression over a period of seven years, it was shown that burnout can specify the development of depressive symptomatology and, subsequently, life dissatisfaction. In contrast, there was no evidence that depressive symptoms inversely increase the risk of burnout. On the positive side, work-related well-being and engagement were associated with high satisfaction and not depression. Thus, it is clear that the experience of the work situation shapes overall health and life satisfaction [3].
Inpatient or outpatient?
Barbara Hochstrasser, M.D., Chief Physician of the Hasliberg Private Clinic, evaluates the need for a stay with burnout patients as a first step, whereby symptoms (DD neurasthenia, depression, chronic fatigue), social environment and what a patient hopes to gain from a stay are already clarified. 80-90% of inpatients suffer from major depression. Accordingly, the therapy is multimodal, but always with a focus, depending on the needs and deficits. “We don’t do a little bit of everything, but teach patients strategies they can use in the long term.” Depression usually improves more quickly than fatigue, he said, and it’s important not to put patients back on their feet too soon. A stay in Hasliberg lasts eight to twelve weeks.
Milan Kalabic, M.D., Chief Physician of the Teufen Clinic, demonstrated that burnout can be treated very well on an outpatient basis. But to prevent patients from burning out in the first place, sensitive primary care physicians are needed, he hopes. A warning symptom could be, for example, that a person is still excessively stressed even during leisure time or that alcohol is used to relax. Escape activism and sleep disturbances are quasi “red flags.” “The soul needs rest in order to be felt,” the psychiatrist said. The four-week outpatient therapy in Teufen includes psychotherapy as well as moderate and regular medical training. The success rate is very good, with 82% of those treated fully able to work after one year.
Medication according to target symptom
Dr. med. Hanspeter Flury from Rheinfelden pointed out that medication for burnout is indispensable in very severe forms. The overall treatment plan he creates with the patient includes psychopharmacology as an integral part, he said. Medication is used according to diagnosis and target symptom according to state of the art, early and intensively. An entry point about sleep disturbances or pain or nervousness could pave the way, he said. “Recover, orient, change” are the guardrails. Care must be taken not to underestimate the time factor. There is no need to rush, one should take time for the dosage of the medication. The patient’s feeling of being in control helps him. Trittico®, Remeron® and Surmontil® drops have proven effective for sleep disorders. Efexor® and Remeron® can be combined very well. Medication for severe burnout cases should be embedded in an overall multimethod, multiphasic treatment plan that also includes psychotherapy, family discussions, body-centered and workplace-centered interventions, Dr. Flury emphasized.
Source: Symposium “Burnout – The Way Back” on December 6, 2012 in Pfäffikon.
Literature:
- DGPPN position paper on burnout available for download at www.dgppn.de
- Maslach C, Jackson SE: The measurement of experienced burnout. J Occupat Behav 1981; 2: 99-113.
- Hakanen JJ, Schaufeli WB: Do burnout and work engagement predict depressive symptoms and life satisfaction? A three-wave seven-year prospective study. J Affect Disord 2012; 141(2-3): 415-424.











