In pediatric and adult patients with insulin-dependent diabetes mellitus, continuous glucose monitoring (CGM) is now incorporated into guideline recommendations to improve glycemic control. Continuous measurements detect glucose variability as well as hypoglycemia and are an alternative to conventional blood glucose measurements. In addition to the “time in range”, various other parameters can be calculated that help to optimize diabetes management.
CGM systems are a significant and increasingly demanded innovation in the field of DIabetic technology. In addition to type 1 diabetics, insulin-dependent type 2 diabetics can also benefit from CGM (“continuous glucose monitoring”) [1]. Continuous glucose monitoring allows patients and healthcare professionals to systematically evaluate glucose trajectories with respect to a wide range of parameters. Structured training programs are an important basis for treatment success (box) . With CGM systems, glucose levels are measured not in the blood but in the tissue fluid of the subcutaneous fat tissue. A small sensor, which is inserted through the skin into the subcutaneous tissue (abdomen or upper arm), detects the glucose level at intervals of a few minutes. Nowadays, there is a great variety of systems with different measurement methods and functions, two important categories are continuous glucose measurement (rtCGM) and flash glucose monitoring (iscCGM) [1]:
Continuous glucose measurement (rtCGM): the values are automatically sent to a receiver device (reader/smartphone on which a special app is installed). It is therefore a real-time measurement. Most systems need to be calibrated regularly
Flash glucose monitoring (iscCGM): the data from the sensor are not transmitted to a receiver via Bluetooth or radio, but are “scanned”. By scanning the sensor, the values measured continuously over the last few hours are actively retrieved using a reader (or smartphone with app). Furthermore, a prognosis of the glucose progression is made.
If certain programmed thresholds are undershot or overshot and hypo- or hyperglycemia is imminent, an alarm is triggered. There are also systems that send a warning signal before glucose levels drop or rise further before critical thresholds are reached.
Hybrid closed loop system combines CGM with insulin pump
In addition to sensor-assisted insulin pump (SUP) therapy, which automatically interrupts insulin delivery for a short time at low glucose levels, the combination of insulin pump and CGM is also the basis for hybrid closed-loop systems [1]. These consist of a continuous glucose meter, an insulin pump, and an algorithm that analyzes glucose measurements in real time. Every few minutes, a glucose value is transmitted to the device, which calculates and automatically adjusts insulin delivery as needed. This involves determining insulin requirements taking into account physiology, total daily dose of insulin, and meals. “Hybrid” means that not everything is automated yet, users have to enter information about meals themselves and deliver the appropriate bolus. In a scientific evaluation of hybrid closed-loop systems, positive glycemic effects (reduction of HbA1c) could be demonstrated [2].
Meanwhile, there are also do-it-yorself (DIY) systems that combine commercially available continuous glucose monitoring (CGM) sensors and insulin pumps with software developed collaboratively by the community [3]: Control algorithm, source code, and instructions for creating your own app are freely available on the Internet.
“Time in Range” and co.: hypoglycemias and glucose variability are recorded
In addition to the HbA1c value, continuous glucose measurement offers additional possibilities for optimizing therapy. Hypoglycemia, which is considered a cardiovascular risk factor in addition to an acute hazard, can be detected and prevented. The various evaluation software programs give the percentage of all glucose values that are in the normal range (“Time in Range”, TIR) as well as the duration in this glucose range as standard. The more glucose values are in the normal range and the fewer below and above, the better the glucose control. Good control is indicated when ≥70% of glucose values are within the normal range [1]. The following is an overview of the most important parameters based on continuous glucose measurement [1]:
- Time in Range (TIR): defined as time in target range is 70-180 mg/dl and 3.9-10 mmol/l, respectively.
- Time Below Range (TBR): time in the low glucose range/below target range is defined as a value below 70 mg/dl and <3.9 mmol/l, respectively.
- Time above Range (TAR): the cut-off for time in the higher range/above target range is values from 180 mg/dl and from 10.0 mmol/l, respectively.
- Coefficient of variation: stable if <36, unstable if ≥36
- Standard deviation
Conclusion: CGM systems have a lot to offer
In summary, continuous glucose monitoring systems combine several therapy-relevant advantages with regard to extended diabetes management goals [4]. These include:
- Simplification of glucose measurement: current glucose value can be seen on the display without much effort.
- Overview of previous glucose history: to support therapy adjustment, the previous glucose history is shown on the display with various evaluation options (e.g. time of glucose values in the normal range, number of hypoglycemic episodes).
- Prediction of future glucose progression: for both real-time glucose monitoring systems and intermittent glucose monitoring systems (FGM/iscCGM), a prediction of future glucose progression is displayed in the form of trend arrows.
- Individual assessment of glucose progression and specific influencing factors: The ability to identify effects of insulin correction, eating, drinking, and physical activity on glucose progression enables better assessment of individual influencing factors and glucose progression.
- Evaluation options: Various options enable both the patient and the physician/diabetic team to systematically evaluate glucose progressions with regard to a wide range of parameters and to obtain information on how to optimize therapy.
- Digital applications: Integrated insulin pump systems use continuous glucose monitoring data for automated regulation of insulin delivery. Continuous glucose measurement is a prerequisite for all automated controls of insulin (“artificial pancreas”).
- Improvement of therapy outcomes: CGM systems have been shown to improve glycemic control as well as quality of life, reduce diabetes-related burden, and increase treatment satisfaction [5]. An evidence-based evaluation by the German Institute for Quality and Efficiency in Health Care concluded that, regardless of age, a higher proportion of diabetics achieved an HbA1c value below 7% when using an rtCGM procedure than when using conventional blood glucose measurements [6].
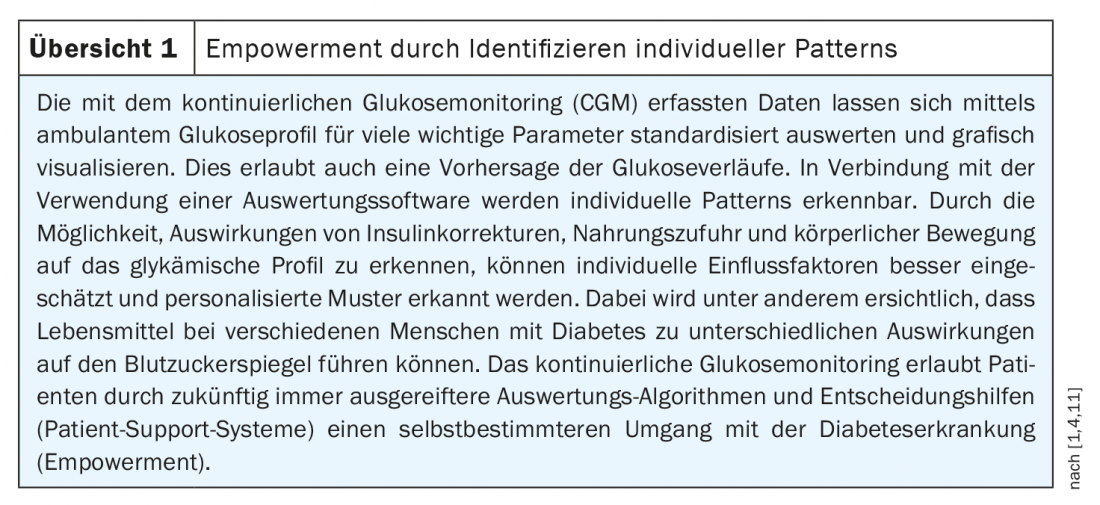
- Empowerment: Continuous glucose monitoring provides patients with a comprehensive information base for their daily therapy decisions and allows a more self-determined management of diabetes due to the various possibilities of evaluations and decision support (patient support systems). Analysis and prediction of individual patterns in glucose trajectories can provide patients and practitioners with links between lifestyle factors and glucose metabolism (Overview 1).
Congress: Diabetology without borders 2021
Literature:
- Kröger J, Kulzer B: New forms of glucose monitoring and the impact on therapy and training in Germany. Diabetes Health Report 2021, 173-182. www.deutsche-diabetes-gesellschaft.de, (last accessed 05.05.2021)
- Garg SK, et al: Glucose Outcomes with the In-Home Use of a Hybrid Closed-Loop Insulin Delivery System in Adolescents and Adults with Type 1 Diabetes. Diabetes Technol Ther 2017; 19(3): 155-163.
- Lenzen-Schulte M: Type 1 diabetes: diabetes therapy brand self-made. Dtsch Arztebl 2019; 116(29-30): A-1378 / B-1139 / C-1123.
- Kröger J, Kulzer B: Diabetes technology: new developments. Digitization and glucose monitoring are changing diabetes therapy and education. Diabetes Health Report 2021, 247-257. www.deutsche-diabetes-gesellschaft.de (last call 05.05.2021)
- Lind M, et al: Continous Glucose Monitoring vs. Conventional Therapy for Glycemic Control in Adults witch Type 1 Diabetes Treated with Multiple Daily Insulin Injections. The Gold Randomized Clinical Trial, JAMA 2017; 317; 379-387.
- Institute for Quality and Efficiency in Health Care (IQWiG) (D12-01). Continuous interstitial glucose monitoring (CGM) with real-time meters in insulin-dependent diabetes. Final Report 2015.
- Kröger J: Continuous glucose monitoring: patient-oriented evaluation. Jens Kröger, MD, Diabetology without Borders, Feb. 27, 2021.
- Kulzer B, et al: Training and treatment program for people using flash glucose monitoring. Mainz: Kirchheim-Verlag 2019.
- Hermanns N, et al: The impact of a structured education and treatment program (FLASH) for people with diabetes using a flash sensor-based glucose monitoring system: results of a randomized controlled trial. Diabetes Research and Clinical Practice 2019; 150: 11-121.
- Gehr B, et al: SPECTRUM. J Diabetes Sci Technol 2017; 11(2): 284-289.
- Kröger J, et al: AGP-Fibel Ernährung – Mit CGM postprandiale Glukoseverläufe analysieren. Mainz: Kirchheim Verlag 2020.
FAMILY DOCTOR PRACTICE 2021