In addition to wound cleansing and debridement/excision, adequate wound dressings in conjunction with topical antimicrobials are important components of the local treatment of burn wounds to contain the potential hazard of wound infection. In this context, consideration of the wound characteristics as well as the individual tolerability of the active ingredients used is crucial.
Burn wounds are at increased risk for local infection, which can spread to invasive infection without appropriate intervention [1]. To counteract this, infection control measures are needed.
Is the burn superficial or deep?
The two wound experts Prof. Mayer Tenenhaus, University of California, San Diego (USA), and Prof. Hans-Oliver Rennekampff, Rhein-Maas Klinikum, Aachen (Germany), recommend the following procedure [1]: Treatment of the burn wound generally depends on the depth of the burn, localization, wound area, as well as the general condition of the patient [2]. Shortly after a burn accident, the determination of the burn depth can be difficult, respectively different wound depths are present, so that more than one local treatment strategy is required [1].
Superficial burn wounds (grade 1 or 2a): The dressing material should promote wound healing and re-epithelialization. Generally, superficial burns do not require antimicrobial treatment, but if the wound area is large, the use of additional topical antimicrobials may be considered to prevent bacterial colonization while maintaining a moist wound environment. Because superficial second-degree burns are not always easily distinguished from deeper burns, topical antimicrobials are often used here. Generally, a combination of antimicrobial ointments or creams (e.g. Polysporin) covered with a non-adherent dressing (e.g. Mepitel or Adaptic) is used initially. If the burn is localized around the eyes, an ophthalmic ointment without steroids is recommended.
Deep burn wounds (grade 2b, 3, or 4) require excision and coverage by flapoplasty and skin grafts. Deep burn wounds often have a mixture of wound characteristics with varying permeabilities and impaired barrier function. In these wounds, the function of topical agents is to delay the onset of invasive infection in advance of surgical excision of necrotic tissue. In deep wounds, excision can reduce the bacterial load and, consequently, morbidity and mortality. If debridement and/or excision are not immediately followed by coverage with skin grafts, fine mesh gauze combined with topical antimicrobials may be used as an interim solution. Typically, these are silver-containing substances or wound dressings (e.g. sulfamylon or acticoat).
|
Nanocrystalline silver coated wound dressings: strong antimicrobial effect The bacteriostatic effects of silver-containing wound materials result from the release of silver ions. Nanocrystalline silver-coated wound dressings (e.g. Acticoat) are characterized by the fact that they contain very small, porous silver particles, which leads to a strong increase in the surface area where ionization and dissolution of silver ions takes place. This results in stronger antimicrobial activity compared to other silver formulations and requires less frequent dressing changes [3]. Frequent wetting with water is required to maintain antimicrobial activity. In a systematic review, the use of nanocrystalline silver was associated with a lower incidence of infection compared with silver sulfadiazine (9.5% vs. 27.8%, odds ratio 0.14; 95% CI, 0.06-0.35) [4]. In addition, dressing changes were associated with less pain. |
Colonized/contaminated/infected burn wounds: If there is suspected or confirmed contamination with methicillin-resistant Staphylococcus aureus (MRSA) pathogens, which are among the most common multidrug-resistant germs, targeted use of complementary topical antimicrobials is appropriate (e.g., mupirocin ointment). Other treatment options (e.g., mafenide) may be useful in the case of heavily colonized or infected burns (adjunctive to systemic antibiotics).
In summary, it is important in the local therapy of burn wounds that the spread of pathogens is counteracted, but there is no universal consensus on which wound dressings and topically applied agents are optimal for this purpose, although substances with antimicrobial activity have been shown to contribute to a reduction in the incidence of invasive wound infections [2].
Silver has been used in wound treatment for several decades. Widely used compounds include silver sulfadiazine, a complex of silver and sulfadiazine (a sulfonamide) [8]. Silver sulfadiazine (SSD) cream (1%) covered with fine mesh gauze, among others, is also used in many centers specializing in burn care [6]. That SSD is associated with antimicrobial activity was demonstrated by a reduction in bacterial colonization. However, in wounds involving more than 50-60% of the total body surface area, prevention or suppression of bacterial colonization is not consistently guaranteed [7]. Otherwise, silver has been offered in the recent past mainly incorporated into wound dressings. The use of silver-containing dressings is particularly useful in cases of relevant bacterial colonization of a wound.
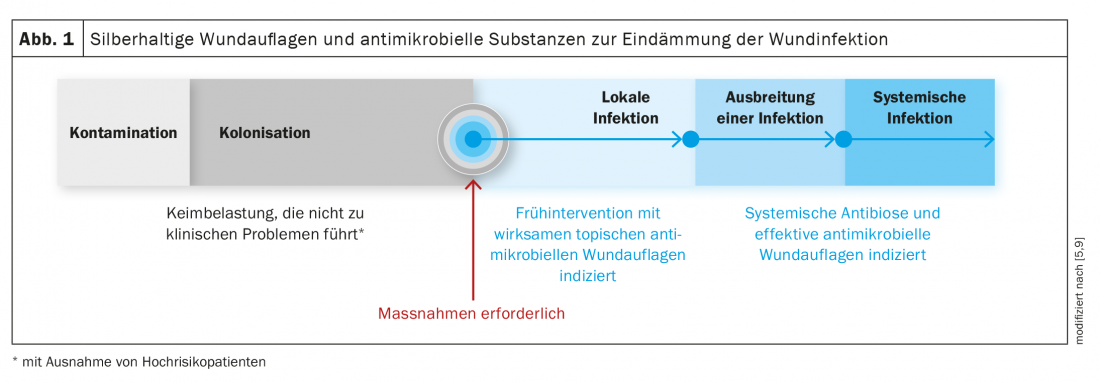
The wound stage and degree of exudation must be taken into account when selecting the wound dressing. The wound environment should be kept moist to ensure the activity of the silver ions. Figure 1 shows the wound condition in burn wounds at which the use of silver-containing products is appropriate. Additional antibiotics are indicated only when an infection spreads or develops into a systemic infection. For some years, nanocrystalline silver has also been used, which has stronger antimicrobial activity than conventional silver (box) .
Literature:
- Tenenhaus M, Rennekampff H-O: Topical agents and dressings for local burn wound care. Last updated: Mar 27, 2020, www.uptodate.com/contents/topical-agents-and-dressings-for-local-burn-wound-care (last accessed 07/02/2021).
- German Society for Burn Medicine (DGV): Treatment of thermal injuries of the adult, s2k guideline, AWMF register number: 044-001 – as of 1 August 2018, (last accessed 02.07.2021).
- Dunn K, Edwards-Jones V: The role of Acticoat with nanocrystalline silver in the management of burns. Burns 2004; 30 Suppl 1: S1.
- Gravante G, et al: Nanocrystalline silver: a systematic review of randomized trials conducted on burned patients and an evidence-based assessment of potential advantages over older silver formulations. Ann Plast Surg 2009; 63: 201.
- Woodmansey EJ, Roberts CD: Appropriate use of dressings containing nanocrystalline silver to support antimicrobial stewardship in wounds. Int Wound J 2018; 15(6): 1025-1032.
- Norman G, et al: Antiseptics for burns. Cochrane Database Syst Rev 2017 Jul 12;7(7): CD011821.
- Nadworny et al: Anti-inflammatory activity of nanocrystalline silver-derived solutions in porcine contact dermatitis. J Inflamm (Lond) 2010; 7: 13.
- SAfW: Wound Compendium of the Swiss Society for Wound Management 2012.
- Ayello EA, et al: International consensus. Appropriate use of silver dressings in wounds. An expert working group consensus. Wounds Int 2012; 1-24.
DERMATOLOGY PRACTICE 2021; 31(4): 36-38