Lesions of the mucosa may have localized causes, but may also be symptoms of systemic diseases. Thus, changes in the oral mucosa are also features of many skin diseases and infectious dermatoses, among others.
As an immunological organ, the oral cavity forms a complex biological functional circuit and is involved in many diseases [1].
Often older patients affected
As shown in an epidemiological study from Denmark, lesions of the oral mucosa are particularly common in the elderly population [2]. One or more lesions of the mucosa were present in 75% of all subjects studied (n=668, 65-95 years). Lingual varicosis (28.3%) was the most common, followed by gingivostomatitis (12.7%), candidiasis (11.8%), and split tongue (9.1%). In addition to a medical examination, salivary flow was measured in stimulated and unstimulated states, and a survey was conducted regarding dry mouth (xerostomia), as well as tobacco and alcohol consumption.
Most often, the manifestation of lesions was associated with smoking and xerostomia. Varicosis was more frequent in subjects with systemic diseases and regular use of medications, especially if they were preparations against cardiovascular diseases. The disorders split tongue and atrophy of the oral mucosa were positively correlated with female sex, dry mouth (xerostomia), and low unstimulated salivary secretion. Oral candidiasis had positive correlations with age, male sex, smoker, >3 disease, regular medication use, low salivary flow rate, and typically occurred in the context of gingivostomatitis, split tongue, atrophy of the oral mucosa, and glossitis rhombica mediana.
Early detection crucial
The oral mucosal lesions mentioned are benign changes, which have a prevalence between 6-62% in relation to all age groups [3]. Early detection and treatment have a favorable effect on the prognosis and the risk of malignant sequelae. In addition to careful inspection and history, biopsies and microbiologic analyses can be informative diagnostic tools for narrowing down etiologic factors, and especially in the case of premalignant or malignant lesions, early diagnosis increases the chances of treatment [3].
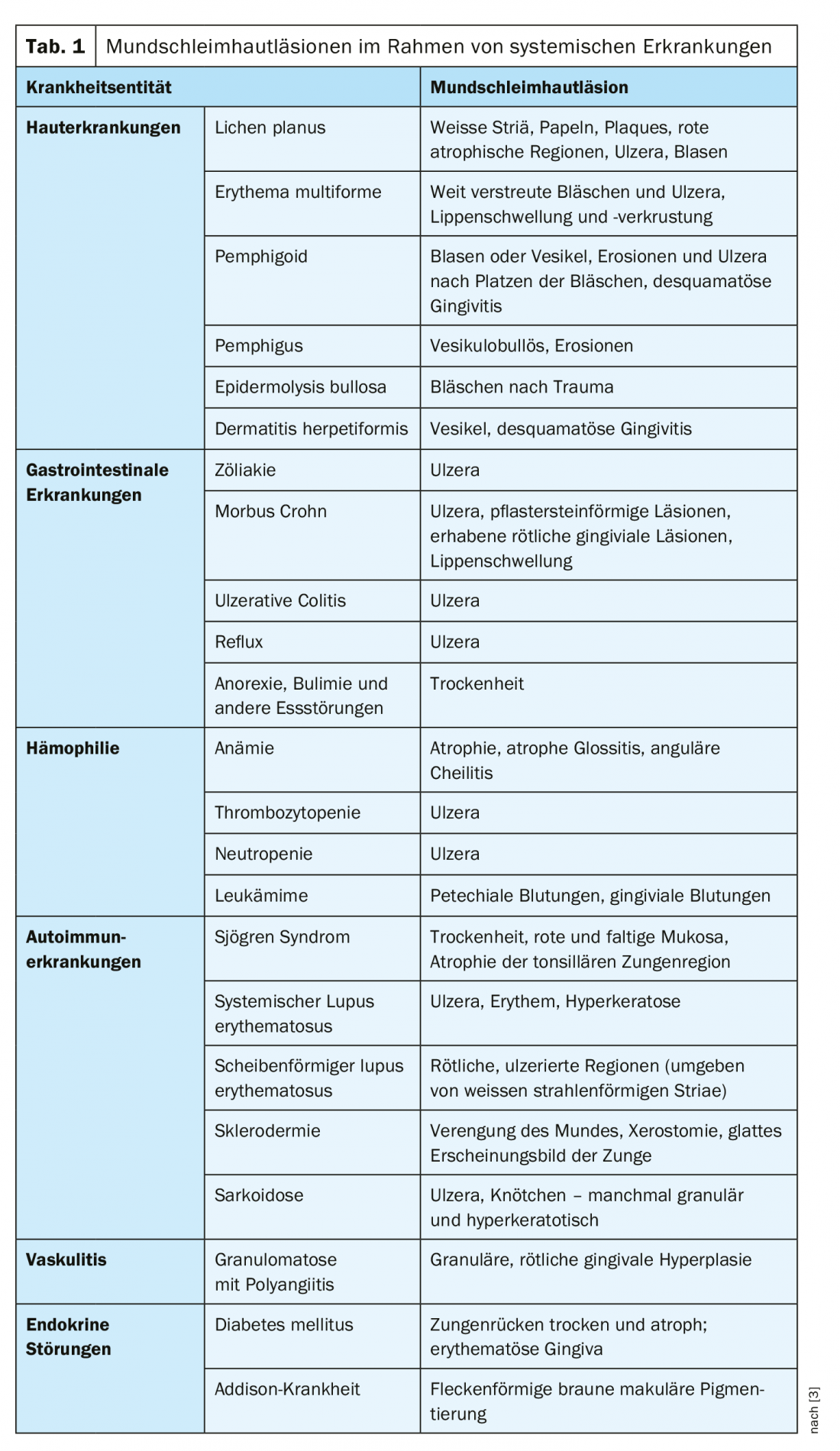
Changes in the oral mucosa may underlie localized or systemic causes of disease [2,3]. In addition to skin diseases (e.g., lichen planus, erythema multiforme, pemphigoid, pemphigus, epidermolysis bullosa, dermatitis herpetiformis), the latter may include gastrointestinal disorders, hemophilia, autoimmune diseases, vasculitis, or endocrine disorders (Table 1). In total, there are over 200 diseases associated with oral mucosal lesions [3]. Among local factors, mechanical irritation or trauma are among the most common causes. Deficiencies of certain nutrients can also lead to mucosal lesions.
Viral causes possible
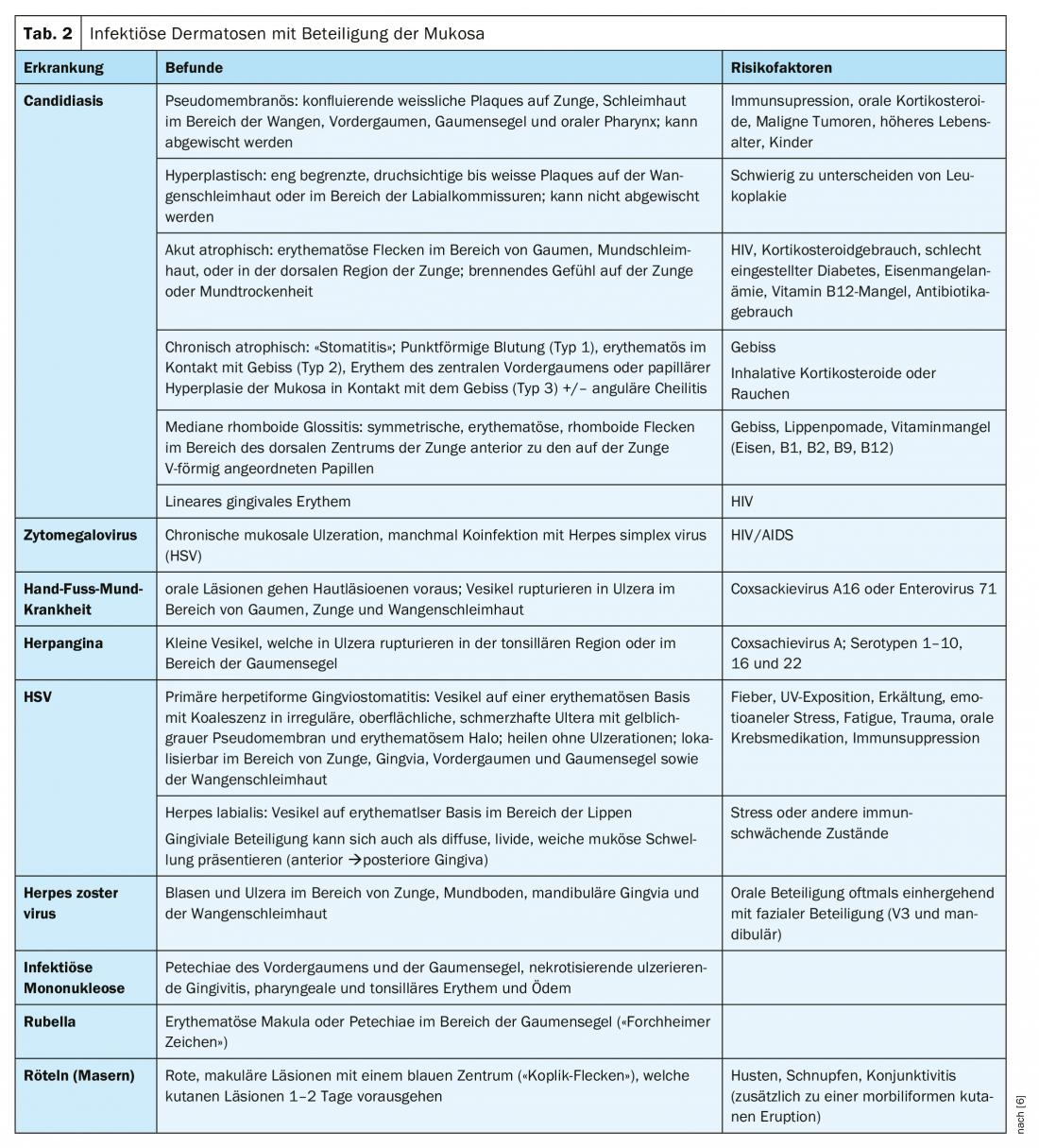
Some lesions of the oral mucosa occur almost exclusively in immunocompromised individuals [4]. They are often asymptomatic changes without malignant potential [5]. Underlying immunosuppressive factors should be clarified and treated [5]. These oral mucosal lesions include oral hairy leukoplakia [3]. This is a symptom of reactivated Epstein-Barr virus, with leukoplakia typically localizable to the posterior portion of the tongue (bilateral, whitish in color, corrugated metal-like surface) [4]. Classic features of oral hairy leukoplakias are whitish plaques laterally on the buccal oral mucosa and on the margin of the tongue [5]. Most often, this condition is asymptomatic and does not require treatment. However, oral hairy leukoplakia may be associated with secondary infection of Candida. Candidiasis is one of the most common infectious dermatoses associated with oral mucosal abnormalities (Table 2).
Herpes simplex virus can lead to multiforme erythema, an acute recurrent immune-mediated mucocutaneous disease (Table 2) [6]. Involvement of the oral mucosa is present in approximately 70% of cases, and children and adolescents are frequently affected [6]. Most often, the mucosa around the tongue, as well as the cheeks of the gingvia are involved, with lesions appearing as edematous and erythematous macules, vesiculobullous lesions, or erosions [6]. Treatment is usually symptomatic and self-limiting. An overview of other infectious dermatoses with oral mucosal involvement is provided in Table 2.
“Burning Mouth Syndrome.”
Burning mouth syndrome (BMS) is characterized by intraoral burning and stinging sensations, mainly affecting the tongue region. Primary forms are idiopathic in origin, secondary forms have one or more underlying causes [5]. Burning pain occurring in the context of BMS can be associated with significant limitations in daily functioning and quality of life for those affected.
Regarding secondary forms of BMS, the following diagnostic procedure is recommended [5]: Medical history, oral cavity examination, laboratory analyses (blood count including hematological parameters; iron, iron absorption; vitamins B1, B2, B6, B12, D3 and folate; zinc; TSH; glucose, HbA1c). A study conducted by the Mayo Clinic (USA) in a sample of 70 patients concluded that xerostomia was present in 28.6% of cases and 24.3% of all patients were denture carriers [5].
The pathophysiology of primary BMS has not yet been fully elucidated [7]. Most commonly used therapeutic interventions include tricyclic antidepressants, α-lipoic acid, clonazepam, and cognitive behavioral therapy [7]. Patient education and monitoring of pain are important factors [7].
Literature:
- Fistarol SK, Itin PH: Oral mucosa as a mirror of systemic diseases. Dermatologist 2009; 60: 866-877. DOI 10.1007/s00105-009-1802-5 http://doc.rero.ch/record/313979/files/105_2009_Article_1802.pdf.
- Lynge Pedersen AM, et al: Oral mucosal lesions in older people: relation to salivary secretion, systemic diseases and medications., First published: 07 March 2015 https://doi.org/10.1111/odi.12337
- Willberg J, Välimaa H, Gürsoy M, Könönen E: Diagnostics of oral mucosae: Histology and microbiology – clinical relevance. TANDLÆGEBLADET 2015; 119: no. 3. www.tandlaegebladet.dk/sites/default/files/articles-pdf/TB032015-184-197.pdf
- Slots J: Oral viral infections of adults. Periodontol 2000 2009; 49: 60-86.
- AAD: Ten Tongue Troubles, CP1140017-1. Roy S. Rogers, III, MD, Professor of Dermatology, Mayo Clinic, College of Medicine.
- Ashack KA: Dermatologic Manifestations in the Oral Mucosa, The Dermatologist 2019; Jul 15, 2019, www.the-dermatologist.com/article/dermatologic-manifestations-oral-mucosa
- Moghadam-Sia S, Fazel N: A diagnostic and therapeutic approach to primary burning mouth syndrome. Clin Dermatol 2017; 35: 453-460.
DERMATOLOGY PRACTICE 2019; 29(6): 37-39