When patients come to the office with skin lesions that are suspicious of skin cancer, often even the primary care physician is unsure how to proceed. Prof. Dr. med. Ralph Braun, Dermatology Clinic University Hospital Zurich, provided information at the Swiss Family Docs Congress about common skin changes and their assessment. He pleaded for constant training on this topic.
(ee) There is a great deal of interest among the general public in having suspicious skin changes checked: on National Skin Cancer Day, when dermatologists offer a free checkup, long lines form in front of the practices. The family doctor is often the first port of call for skin changes. A survey of 1200 primary care physicians found that 39% felt unsure about evaluating skin lesions suspicious for malignancy, and 25% felt very unsure. According to one study, one-day training in skin lesion assessment has no long-term effect. Rather, constant continuing education is necessary.
Watch for incidental findings in the family practice setting
The speaker emphasized the important function of the family doctor: “Unlike us dermatologists, family doctors also see incidental findings in patients who actually come to the practice for something else.” Switzerland has the highest rate of new melanoma cases in the world after Australia and New Zealand. However, mortality has remained the same in recent years, indicating that melanomas are increasingly diagnosed at early stages with good chances of cure. The incidence rate of white skin cancer is so high that these tumors are not even recorded in tumor registries.
Non-melanocytic skin lesions
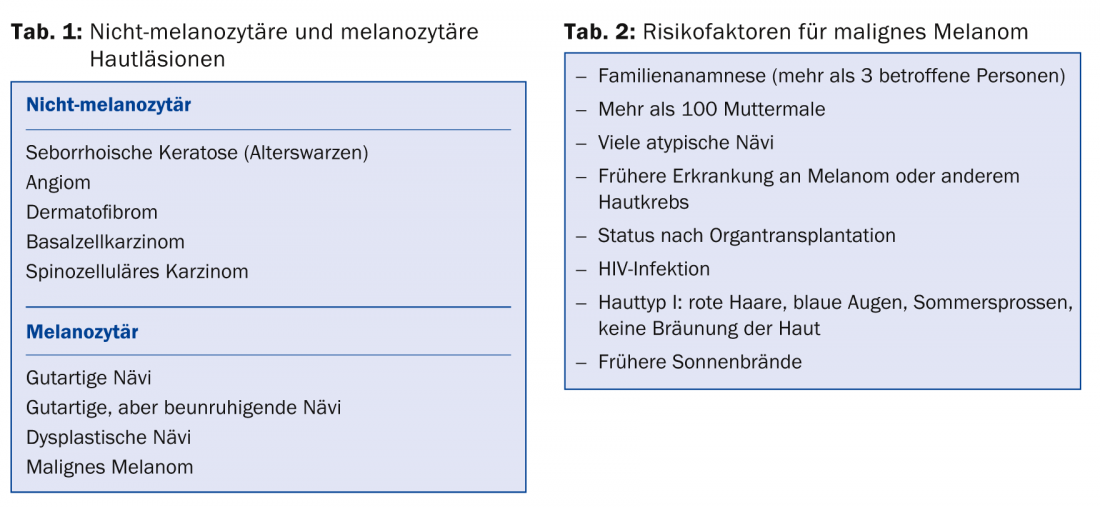
Among the lesions suspicious for skin cancer, a rough distinction is made between non-melanocytic and melanocytic skin manifestations (Tab. 1) . The lecturer informed about typical characteristics of benign non-melanocytic skin manifestations, so that a differentiation from skin tumors is better possible:
- Seborrheic keratoses (age warts) are sharply defined and look a bit like they were put on the skin (chewing gum).
- Angiomas are red and sharply demarcated – they can sometimes turn black overnight.
- Dermatofibromas are usually very hard and tend to pull inward.
Basaliomas
Basaliomas are the most common form of skin cancer. They usually occur in light-exposed areas, are broad-based and nodular with waxy, pearly areas, and may ulcerate centrally. Dark basal cell carcinomas also occur, and large vessels are often seen on the lesion. Basal cell carcinomas are also characterized by great vulnerability. “Any skin lesion that is new to a light-exposed part of the body, is raised, and does not heal properly is a basal cell carcinoma until proven otherwise,” the speaker said. “This rule applies to younger individuals as well.” Although there are good treatment options for basal cell carcinoma, patient morbidity is high when multiple lesions occur.
Spinalioma
Spinaliomas can metastasize, which is not uncommon, especially in individuals with immunosuppression. In organ transplant patients, spinaliomas are a frequent cause of death; therefore, these patients should be closely monitored dermatologically. Spinaliomas often affect the scalp, tend to field cancerize, and form crusts that the patient scrapes off, but then reform. The differential diagnosis to eczema is often not easy, but eczema usually disappears after three weeks of therapy. If in doubt, a biopsy must be taken. “UV light is the gasoline that keeps the cancer cells’ engine running,” Prof. Braun said. “That’s why consistent sun protection is very important in spinalioma.”
Melanocytic skin lesions
There are many different forms of benign nevi. As a rule, in them the skin fielding (as in the surrounding skin) is visible. More difficult to evaluate are benign nevi with a worrisome shape or rapid growth. These include, for example, the Sutton nevus, which is surrounded by a depigmented area. In young people, Sutton nevi are harmless; in older people, they are judged to be melanoma until proven otherwise. Congenital nevi are brown and usually hairy. In case of large extension or localization in the face, they burden the patients resp. their parents strongly. Because the risk of degeneration is high, patients must be closely monitored. The situation of patients with many dysplastic nevi is problematic, as they often show features suggestive of malignancy. These patients also require regular monitoring.
Malignant melanoma
In malignant melanoma, a distinction is made between different forms and stages, for example according to tumor thickness (Breslow) and depth of penetration (Clark). 50-70% of patients have superficial spreading melanoma, 15-20% have nodular melanoma, and 5-10% have melanoma arising on lentigo maligna. Nodular melanomas tend to grow rapidly in depth and metastasize. Acro-lentiginous melanomas form in the nails and on the palms of the feet and hands; a dark longitudinal stripe in a nail should always be clarified. Several factors increase the risk of melanoma (Table 2).
How should I examine the patient?
Early stage melanomas can be cured with simple surgery in 98% of cases. Therefore, early diagnosis is very important. Prof. Braun showed how the examination of the skin should be performed:
- Patient stripped down to underwear
- Systematic examination of the entire body, if possible always according to the same scheme, so that no body region is forgotten
- Do not forget “hidden” areas of the skin: Soles of feet, spaces between toes, behind ears, scalp, body folds.
- Good lighting, possibly illuminated magnifier as an aid
- Watch for “ugly ducklings,” skin lesions that look different from the others
- Comparison of the actual condition with preliminary images
Self examination is useful
It is useful to recommend self-examination to patients and to advise them to look at poorly accessible parts of the body with a mirror. In patients with many dysplastic nevi, dermatology now relies on total body photography, which also allows efficient 3D imaging. For those interested, the dates of the next dermoscopy courses are posted at www.dermoscopy.ch.
Source: Swiss Family Docs Conference, August 28-29, 2014, Zurich
HAUSARZT PRAXIS 2014; 9(10): 44-45