Transmural response (TR) and healing (TH), as assessed by intestinal ultrasound (IUS), are becoming increasingly important as treatment goals in Crohn’s disease (MC). A study team from Switzerland, Germany and Austria investigated the extent to which this can also apply to ulcerative colitis (UC). They want to find out whether early changes in the IUS can be a predictor of future response and remission after one year of therapy.
Crohn’s disease and ulcerative colitis are progressive diseases with a destructive course. In line with the “treat-to-target” approach, regular monitoring of the disease using objective parameters is necessary. The TRUST and TRUST&UC studies already showed a good correlation between changes in intestinal ultrasound (IUS) parameters (e.g. intestinal wall thickness, BWT), laboratory parameters and endoscopy, explained PD Dr. Luc Biedermann, Head Physician at the Department of Gastroenterology and Hepatology, University Hospital Zurich [1]. The TRUST-BEYOND study is an ongoing, prospective, non-interventional, multicenter study in patients with active Crohn’s disease or ulcerative colitis who were receiving therapy with biologics or Janus kinase inhibitors at baseline. The aim of the study is to assess the predictive value of transmural response (TR) or transmural healing (TH), assessed at week 12, for disease progression after 52 weeks. Dr. Biedermann presented the results of an interim analysis at the annual congress of the Swiss Society of Gastroenterology (SGG) in Interlaken.
The interim analysis included 77 CU patients (63.6% male, median age 38.6 years, median disease duration 5.85 years) with clinically active disease (SCCAI 8.5 ± 2.2) with elevated BWT at baseline who had a documented visit at 12 and 52 weeks on the same therapy. In the vast majority, the most severely affected bowel wall segment was the sigmoid colon with a mean BWT of 5.22 ± 1.28 mm at baseline. At W12 after initiation of therapy, the proportion of CU patients with TR and TH was 67.5% (n=52) and 31.2% (n=24), respectively. Transmural response was defined as a reduction in bowel wall thickness of at least 25% vs. Baseline and/or normalization, TH meant normalization of BWT and color Doppler signal.
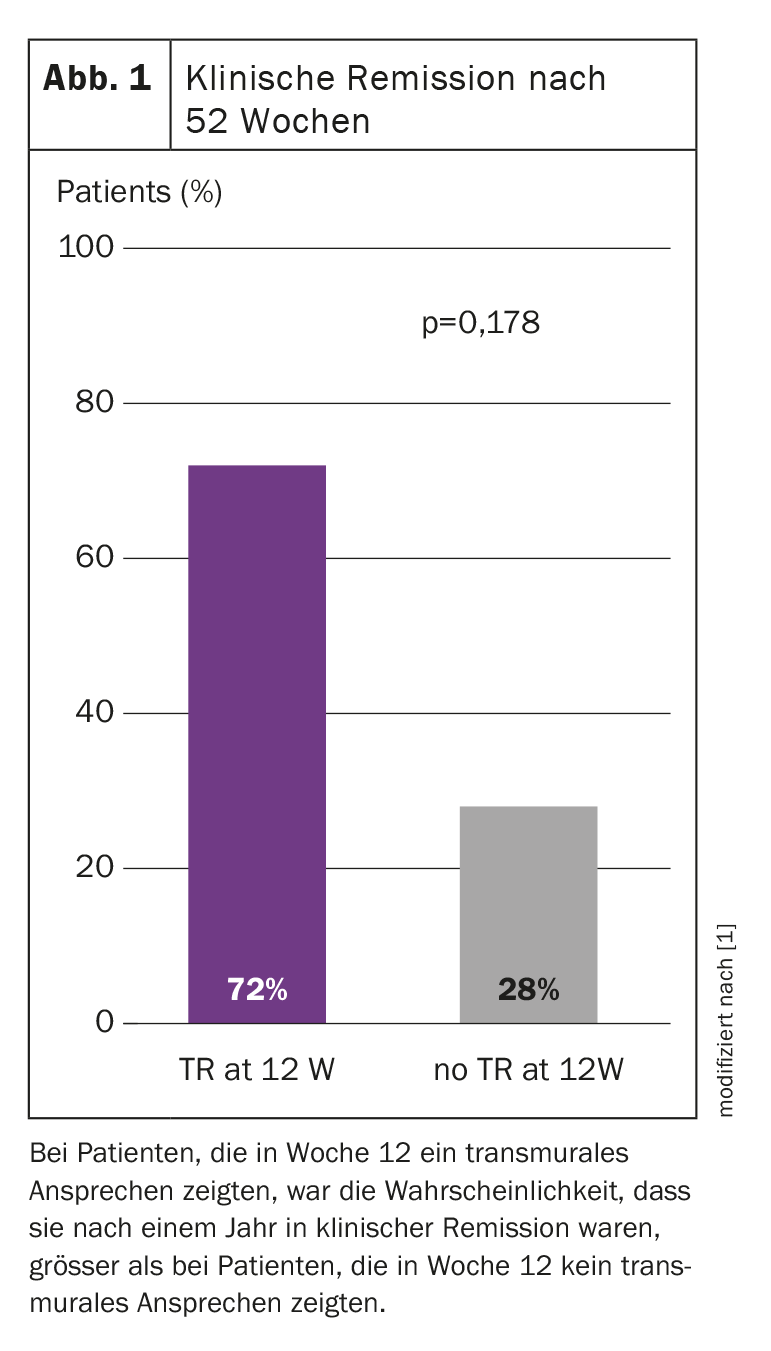
TR at week 12 brings three out of four patients into remission after one year
At W52, the rates of CU patients increased to 77.9% (n=60) for TR and 41.6% (n=32) for TH. Over the course of the study, patients with TR had a numerically lower SCCAI score at W12 and W52 and lower fecal calprotectin levels than patients without TR. Of note, 72.2% (n=39) of patients with TR at W12 were in clinical remission at W52 compared to 27.8% (n=15) of patients without an early transmural response (p=0.178) (Fig. 1). “So if you achieve a response at week 12, three out of four of your patients will be in clinical remission after one year. If you don’t achieve TR at 12 weeks, only one in four will be. In other words, ultrasound at three months seems to be an excellent and elegant predictive tool in CU,” Dr. Biedermann explained. As already observed in Crohn’s disease, the results indicate that the IUS has a predictive value to a certain extent in ulcerative colitis, he concludes.
Congress: SGG Annual Congress 2023
Source:
- Biedermann L: Lecture “One-year intestinal ultrasound improvements in UC patients on biologic or JAKi therapy – interim results of the TRUST BEYOND study”; Annual Congress of the Swiss Society of Gastroenterology (SGG), Interlaken, 14.09.2023.
GASTROENTEROLOGY PRACTICE 2023: 1(2): 25 (published 28.11.23, ahead of print)